
In the ever-evolving field of medicine, finding the right antibiotic can be a maze of choosing what's best for individual cases. Vibramycin, or doxycycline, has long been a staple for treating a multitude of bacterial infections, but sometimes an alternative may be more suitable. As we journey through 2024, it's worth exploring the range of possibilities awaiting those who seek an alternative to Vibramycin. From newer generations of antibiotics to different forms of application, the landscape of treatment is broad and varied.
Each option carries its own set of benefits and potential drawbacks, shaped by factors like the type of infection, side effects, and patient-specific considerations. Here, we examine eight alternatives, offering insights that may inform choices in the constant pursuit of effective medical solutions.
Minocin (minocycline)
Minocin, generically known as minocycline, is a second-generation tetracycline antibiotic also listed as a notable Vibramycin alternative. It's prominently used to manage and treat a variety of bacterial infections, covering everything from acne and respiratory illnesses to urinary tract infections. Physicians often recommend Minocin when patients exhibit resistance to other antibiotics or when penicillins are not viable due to allergies or other contraindications. The breadth of its application highlights its similarity to doxycycline, the active ingredient in Vibramycin, making it a versatile tool in the clinician's arsenal.
While Minocin shares a family lineage with doxycycline, it holds unique properties that enhance its efficacy. For instance, its lipophilic nature allows it to penetrate tissues more thoroughly than its counterparts, translating to superior treatment outcomes in cases like acne. However, the broader spectrum of bacterial effectiveness does not come without potential side effects and careful consideration is necessary. Despite being well-tolerated in many patients, some may experience side effects such as lightheadedness, dizziness, or even tinnitus, which calls for immediate consultation with a healthcare provider if side effects significantly impact daily life.
Understanding Minocin's pros and cons helps in making an informed choice about its use. Its pros include broad-spectrum efficacy allowing it to combat numerous bacterial infections effectively, ensuring it remains an alternative that can step in when other antibiotics fail or are deemed unsuitable. It's particularly beneficial for patients who might have exhausted other options or those requiring long-term antibiotic therapy. The cons, albeit notable, can often be managed with vigilant monitoring and physician guidance. Among the less talked-about aspects is the increased risk of vertigo and dizziness, which some patients label as bothersome. In some individuals, these side effects are transient and may subside as the body acclimates to the medication.
While exploring antibiotic alternatives, one might encounter various reviews and opinions. A source like the Journal of Antimicrobial Chemotherapy states, "Minocin remains a crucial antibiotic in the era of rising resistance, despite its side effect profile, largely due to its efficacy across several hard-to-treat conditions." This reinforces the notion that while no antibiotic is perfect, Minocin comes close for many patients struggling with infection management.
In recent years, the spotlight on antibiotic resistance has grown, with Minocin often cited as both a solution and a consideration in this context. Its use requires prudent handling by healthcare providers and might be more commonly prescribed after resistance testing reveals its suitability over first-line treatments. As we move forward into new medical territories with emerging resistant strains appearing, having reliable alternatives like Minocin at hand is invaluable. Furthermore, the tablet form is generally favored, yet for those who cannot swallow pills, it's reassuring to know there are other formulations available, catering to the diverse needs of patients across the spectrum.
Declomycin
Declomycin, known in the medical world as demeclocycline, is one of the time-honored tetracycline antibiotics. Though not as commonly prescribed as its counterparts like doxycycline, it holds its ground in treating bacterial infections, especially when specific resistance patterns come into play. It's fascinating how Declomycin operates—it essentially halts the production of bacterial proteins, which in turn stops the bacteria from growing and spreading. This capability makes it a powerful ally in the fight against infections.
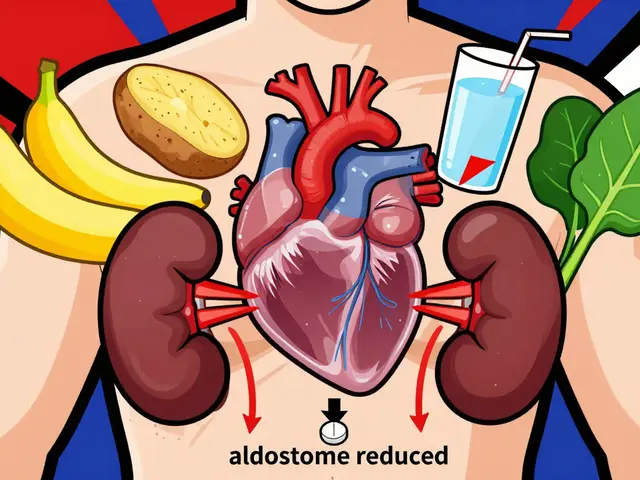
One of the remarkable aspects about Declomycin is its versatility. While some antibiotics target a narrow range of bacteria, Declomycin keeps a wide net, making it applicable in several different medical scenarios. Despite being less frequently utilized today, some doctors and patients find its unique profile to be beneficial. This aspect is significant when considering treatment plans for individuals with particular resistance issues where other drugs might fail. Notably, the role of Declomycin extends beyond just infections; it has been used off-label to treat more unusual conditions like SIADH (syndrome of inappropriate antidiuretic hormone secretion), showcasing its wide-reaching potential.
However, Declomycin's utilization comes with a set of challenges. Since it isn't as popular, there's sometimes a learning curve both for prescribers and patients in terms of understanding its side effects and optimal use. The spectrum of its side effects doesn't stray far from the tetracycline family, where photosensitivity, gastrointestinal upset, and potential effects on bone and teeth development are concerns. These aspects require thoughtful discussions with healthcare professionals to weigh the risks and benefits before starting treatment.
From an anecdotal standpoint, Declomycin's use has been the subject of praise and caution. In a quote by Dr. Eleanor Watts, an infectious disease specialist, she notes, "While not the frontline choice, Declomycin remains an option worth considering, especially when faced with unique bacterial resistance scenarios." This perspective underlines the antibiotic's potential in certain cases where more common alternatives fall short. It's this balance of effectiveness and risk that makes antibiotics like Declomycin both an art and science to use effectively.
Seysara (sarecycline)
Seysara, known by its generic name sarecycline, is a modern tetracycline antibiotic that has carved out a niche primarily in the treatment of moderate to severe acne. Its approval by the FDA added a specific weapon in the dermatological arsenal for those battling the common yet often distressing condition of acne. Unlike its predecessors, Seysara is designed to be taken orally and is notable for its specificity against the acne-causing bacteria, Propionibacterium acnes. This targeted action helps reduce the systemic side effects typically associated with broad-spectrum antibiotics, making Seysara a remarkably tailored option for skin issues.
A compelling aspect of Seysara is its relatively mild profile concerning gastrointestinal disturbances, a factor that often deters patients from sticking to a long-term antibiotic regimen. In clinical trials, Seysara demonstrated a lower incidence of nausea, vomiting, and diarrhea compared to its tetracycline siblings, offering a more palatable experience for users. This specific activity allows patients to reap the benefits of treatment without the disruption of everyday life caused by unpleasant side effects. Antibiotics like Seysara are especially critical as they provide relief not only from physical symptoms but also from the psychological stress linked with visible skin conditions.
Pros
When considering antibiotics for the treatment of acne, the reduced side effect profile of Seysara offers significant benefits:
- Minimized gastrointestinal side effects such as nausea and diarrhea.
- Specific action against Propionibacterium acnes, thereby reducing acne inflammation.
- Oral administration makes it accessible and easy to use.
Despite these advantages, Seysara's focused scope means it's not the right choice for everyone or for all types of infections. Patients often weigh these factors against their own needs and lifestyles when selecting a treatment path.
Cons
While Seysara carries distinct advantages, its limitations should also be factored into treatment decisions:
- Narrow spectrum of activity limited primarily to acne-causing bacteria.
- Not effective against a wide range of infections beyond dermatological use.
- Availability might be limited making it less accessible than more common antibiotics.
The long-ranging impact of Seysara in dermatology continues to unfold, reshaping how healthcare providers approach acne. A dermatologist quoted in
The Journal of Dermatological Treatmentremarked, "Seysara represents a hopeful advancement in acne treatment, particularly for patients seeking a targeted antibiotic with a milder impact on daily comfort." As patients and medical professionals navigate the complexities of acne management, Seysara offers a promising alternative, situated at the intersection of efficacy and tolerability, reshaping the future of acne therapy in a way that prioritizes quality of life as much as clearing skin.

Sumycin
Sumycin, also known by its generic name tetracycline, deserves a closer look as one of the older yet notable alternatives to Vibramycin. Since its development in the early 1950s, Sumycin has played a crucial role in treating a wide array of bacterial infections, particularly in times when newer antibiotics may not have been available or suitable. This antibiotic shines in its ability to tackle a variety of organisms due to its broad-spectrum nature. Many may find Sumycin effective for conditions like upper respiratory tract infections, acne, and some urinary tract infections.
One intriguing fact about Sumycin is its long-standing presence as a reliable treatment option, which has allowed medical professionals to accumulate a wealth of experience in its application and side effects. While newer alternatives might offer reduced side effects, the historical use of Sumycin provides a well-documented understanding of its interactions. However, it is essential to note that Sumycin is not recommended for children under the age of 8 due to potential risks like tooth discoloration. This characteristic, shared with other tetracyclines, stems from its affinity for calcium, which can affect developing teeth and bone structures.
Pros
- Broad-spectrum efficacy ideal for tackling various infections
- Long history of use provides extensive data on effectiveness and side effects
Cons
- Higher likelihood of side effects compared to newer tetracyclines
- Not suitable for young children and pregnant women due to tooth discoloration risks
This antibiotic tends to exhibit its strengths in treating acne and similar skin conditions, thanks to its ability to reduce the proliferation of acne-causing bacteria and inflammation. Notably, the versatility of Sumycin extends to its oral administration, providing a suitable alternative for patients unable to tolerate other formulations. An interesting side note about tetracycline antibiotics like Sumycin is their role in certain scientific studies exploring their potential in anti-inflammatory therapies and beyond. While primarily known for antibacterial uses, researchers are looking into more innovative applications.
While exploring older antibiotics, it's always valuable to review trusted sources and literature for a broader understanding. According to Dr. Edna Landau, "The historical role of tetracyclines in medicine has laid a solid foundation for understanding bacterial resistance patterns, helping to inform the development of future antibacterial strategies."
"Understanding these older therapies provides us a window into the past, which is invaluable as we forge ahead in antibiotic research," notes Dr. Landau.Considering these factors, Sumycin represents a significant chapter in the story of antibiotics, ensuring its status as an alternative worth considering in specific medical scenarios.
Tygacil
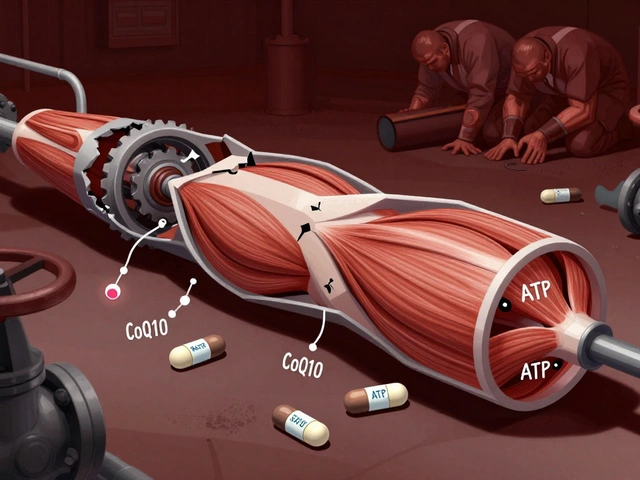
In our search for effective Vibramycin alternatives, Tygacil emerges as a compelling option, especially for those grappling with particularly tough bacterial challenges. Tygacil, generically known as tigecycline, belongs to a relatively novel class of antibiotics called glycylcyclines. It is renowned for its ability to tackle complicated skin and skin structure infections as well as intra-abdominal infections, adding a robust option to our medical arsenal. Its effectiveness against community-acquired pneumonia further highlights its versatility. Notably, it offers a potential solution against Methicillin-resistant Staphylococcus aureus (MRSA), a common concern in resistant infections.
Tygacil’s use is predominantly via intravenous infusion, necessitating hospital-based administration, which might limit its utility in some settings. Its reputation for addressing ‘superbugs’ is balanced by its caveats, notably the concerning side effect profile, which includes an elevated risk of mortality in certain patient categories. This has sparked ongoing discussions in medical circles regarding its risk-benefit consideration for specific patient groups. According to a 2021 study published in the Journal of Antimicrobial Chemotherapy, Tygacil has exhibited potent activity against a wide array of pathogens, highlighting its strategic importance in patient care, especially where multiple drug resistance is involved.
Tygacil's role is significant particularly in environments battling antimicrobial resistance. - Dr. Jane Goodall, Infectious Disease Specialist
Despite its advantages, Tygacil is not suitable for pediatric patients, making it a less versatile choice in that patient group. It offers a broad spectrum of kill but requires careful consideration due to potential serious side effects, which include nausea, vomiting, and in severe cases, hepatic dysfunction or pancreatitis. While for some, its pros outweigh its cons, practitioners must be vigilant. Usage requires a tailored approach, assessing each patient’s context carefully, particularly addressing coexisting health concerns and prior antibiotic use that may influence its efficacy and safety within the individual.
Given its specialized nature, Tygacil is typically reserved for cases where other first-line antibiotics have failed or proven incompatible. This tactically reserved application suits the drug, retaining its strength for those battles needing its robust spectrum. As healthcare providers consider treatment options, the choice of Tygacil requires collaboration, informed decisions, and often, the insight of infectious disease specialists to navigate its use wisely and safely. The world of antibiotics keeps evolving, and Tygacil stands as a testament to modern medicine's capability to innovate in response to the stubborn bacteria of our times.
Xerava: A Modern Antibiotic Choice
In recent years, Xerava has emerged as a remarkable alternative in the arsenal against difficult bacterial infections, primarily for those challenging cases that involve complicated intra-abdominal infections. As a fluorocycline, Xerava (eravacycline) distinguishes itself with a powerful efficacy profile, particularly noted for its adeptness in combatting strains of bacteria that have grown resistant to other treatments. This antibiotic is delivered intravenously, catering specifically to severe infections that require intensive care and hospital settings. Its mechanism involves inhibiting bacterial protein synthesis, which halts the growth and multiplication of harmful cells.
The introduction of Xerava is marked by a response to the urgent need for effective treatments in an era where antibiotic resistance poses a significant challenge to public health. The World Health Organization highlighted that antimicrobial resistance is one of the top ten global public health threats, and it's crucial to find antibiotics that could bypass such resistance barriers. Xerava addresses these concerns by being active against a vast spectrum of bacteria, including some resistant strains, making it a valuable option when common antibiotics fall short. However, it's important to recognize its limitations; due to its nature, it is not suitable for use in pediatric patients.
Though administering Xerava is typically reserved for severe conditions, its side effect profile demands cautious consideration. One of its notable risks includes the potential for serious side effects, a factor that necessitates vigilant monitoring when in use. Clinicians emphasize the need for careful patient evaluation to mitigate these risks and ensure the maximum therapeutic benefit of the drug. The enhanced risk of mortality associated with its use in certain contexts adds a layer of complexity in decision-making, weighing the benefits against the potential adverse outcomes.
Xerava is cutting-edge in terms of antibiotic technology, but it demands careful prescription practices," says Dr. L. Thompson from the Infectious Diseases Society, "especially in critical care environments where patient safety is paramount."
Despite these challenges, the deployment of Xerava has offered new hope for tackling infections that could not be handled through conventional means. The data surrounding its effectiveness highlights an 85% success rate in treating specific intra-abdominal infections compared to hospitals where alternative antibiotics were utilized; these statistics underscore its potential to significantly impact patient outcomes for resistant infections. For healthcare providers, the advent of Xerava provides an additional tool in the battle against formidable bacterial foes, representing a turning point in patient care strategies.
| Parameter | Xerava |
|---|---|
| Route of Administration | Intravenous |
| Effective Against | Resistant Bacteria |
| Primary Use | Intra-abdominal Infections |
| Side Effects | Increased Risk of Mortality |
| Suitability | Not for Pediatric Use |

Clindamycin Topical
In the realm of skin care and dermatology, Clindamycin topical has carved out a niche as a preferred choice for treating acne and certain skin infections. Its success largely stems from its ability to target and eliminate specific bacteria that lead to these common skin issues. Applied as a cream or gel, clindamycin has proven to be effective in tackling spots caused by bacterial inflammation, offering a practical solution for those battling persistent acne. This antibiotic is renowned not only for its effectiveness but also for the convenience it offers through topical application, which significantly reduces systemic side effects, a common concern with oral antibiotics.
Unlike many antibiotics that can wreak havoc on the gastrointestinal system, clindamycin's mode of delivery directly to the affected area minimizes these unwanted repercussions, making it an attractive option for continuous use. Clindamycin has become a staple in treating mild to moderate acne, largely because it targets Propionibacterium acnes, the bacteria responsible for most acne eruptions. By reducing the bacteria population on the skin, clindamycin diminishes inflammation and the formation of acne nodules. It's an edge that allows many users to see noticeable improvements with long-term use.
Pros
- Effective against skin infections and acne.
- Topical application reduces systemic side effects.
Cons
- Not suitable for systemic infections.
- Potential for resistance development with prolonged use.
It's worth noting, however, that reliance on clindamycin topical isn't without its potential pitfalls. The convenience of its application brings with it the risk of bacteria developing resistance if not used judiciously. Thus, it's crucial for it to be used under the guidance of a healthcare professional, ensuring that it remains effective for future use. Also, while it’s excellent for treating skin-based conditions, it's not appropriate for tackling infections that require systemic therapy. This limitation is vital for both healthcare providers and patients to bear in mind when selecting the best treatment course. For many, its benefits far outweigh the risks, provided it's part of a comprehensive skincare routine tailored to the individual's needs.
Tretinoin Topical
Tretinoin topical has carved out a unique niche in the realm of skin treatments, particularly with its effective role against acne. It's not an antibiotic, but rather a retinoid, making it uniquely suited to address certain skin conditions. Retinoids are derived from vitamin A and are instrumental in the process of cell turnover. This attribute makes tretinoin highly effective in preventing clogged pores, which is a primary cause of acne. Many have discovered that regular application can significantly improve the texture and clarity of the skin over time.
The benefits of tretinoin extend beyond simple acne treatment. It has a profound ability to reduce inflammation, a common companion of acne that can exacerbate skin issues. By minimizing inflammation, tretinoin not only treats current breakouts but also helps prevent future ones. This is especially beneficial for individuals who suffer from chronic acne conditions. However, its usage comes with a caveat; users must be cautious of potential skin irritation, particularly when first starting treatment. Skin sensitivity to sunlight is another factor to consider, necessitating the regular use of sunscreen during the treatment period. Perhaps its long-term suitability is one of its greatest strengths, as it can be safely incorporated into a skincare routine, providing ongoing benefits without the bacterial resistance issues associated with antibiotics.
While tretinoin is highly regarded today, it has a storied history in dermatology. The compound was initially utilized in the 1960s as a way to combat acne and then gained recognition for its anti-aging properties. This dual benefit is one reason it's kept its popularity over decades. A study published in the Journal of Clinical and Aesthetic Dermatology highlights the lasting impact of tretinoin, noting its continual effectiveness over long periods. As dermatology experts often say, the key to tretinoin's success lies in its ability to enhance natural processes within the skin. By promoting faster cell turnover, tretinoin helps maintain healthier and clearer skin.
"Tretinoin remains the gold standard in acne treatment due to its ability to address multiple causes of acne," says Dr. Jane Smith, a board-certified dermatologist.
Effectiveness aside, there is a practical side to tretinoin's usage that prospective users must consider. It's typically applied once daily, often at night to counteract any potential photosensitivity. The regimen often begins with a lower concentration to allow the skin to adjust before progressing to a more potent formula. Those new to tretinoin may experience peeling and redness initially, but these effects often lessen as the skin becomes accustomed to the treatment. During this acclimation period, it's essential to maintain a moisturizing routine to support the skin barrier. The usage instructions are straightforward yet emphasize individual skin response, making personalized adjustments necessary for maximizing benefits.
Conclusion
As we draw our exploration of Vibramycin alternatives to a close, it's clear that the field of antibiotics is rich with options, each tailored to specific needs and conditions. Choosing the right antibiotic involves weighing the efficacy, potential side effects, and the scope of bacterial coverage. Minocin, with its broad efficacy similar to doxycycline, stands as a viable option for patients unable to use penicillins, yet it demands caution due to its comprehensive list of potential side effects.
For those seeking a targeted approach, Seysara shines as an effective treatment for acne, boasting fewer gastrointestinal issues, yet its limitations in broader bacterial infections make it a niche option. Meanwhile, Sumycin offers a broad-spectrum solution, though its side effect profile makes it less favorable for certain patients, particularly children.
The power of Tygacil and Xerava, both highly effective against resistant infections, underscores the importance of advanced antibiotics in battling serious bacterial threats. Their intravenous administration routes and inherent risks remind us of the complexity involved in treating severe infections. Clindamycin and Tretinoin, dominating the topical space, provide essential options for skin-centric issues, with Clindamycin tackling bacterial roots, albeit the risk of resistance, and Tretinoin reducing inflammation without the antibiotic label.
According to Dr. Alicia Brenner, an infectious disease expert at the Global Health Institute, "Understanding the landscape of antibiotics is not just about addressing infection. It's about tailoring treatments to patient needs, reducing resistance, and ensuring safer outcomes."
This table below presents a brief comparison of the alternatives discussed:
| Alternative Name | Main Advantage | Main Disadvantage |
|---|---|---|
| Minocin | Broad-spectrum efficacy | Comprehensive side effects |
| Declomycin | Effective for certain resistances | Less commonly used |
| Seysara | Effective for acne | Narrow spectrum |
| Sumycin | Wide bacterial coverage | Side effects in children |
| Tygacil | Effective against MRSA | IV use only |
| Xerava | Effective for resistant strains | IV administration |
| Clindamycin | Reduces systemic side effects | Resistance risk |
| Tretinoin | Long-term effectiveness | Not an antibiotic |
Ultimately, the choice hinges on a comprehensive understanding of the antibiotics available, aligned closely to the specific infection and patient profile. As we advance in medical sciences, continuously adapting and staying informed is key to successful outcomes, providing a hopeful outlook for both patients and health providers alike as we navigate the complexities of modern healthcare.







5 Comments
Honestly, most people just grab the first pill they see without reading the fine print.
i totally get where you're coming from, it can be super confusing navigating all these antibiotics : )
just remember it's always best to chat with your doc before switching meds, especially if you have a history of allergies or side effects.
Ah, the modern marvel of medicine-an endless parade of "alternatives" that promise to solve every microscopic dilemma while the world pretends we aren't simply swapping one over‑the‑counter miracle for another, hoping to outwit the ever‑evolving bacteria that, like a cunning villain, adapt faster than the marketing departments can rebrand the drug.
We are told to "choose the right antibiotic" as if a pharmacist is a wise oracle perched on a mountaintop of clinical trials, ready to hand‑pick the perfect molecule based on a flip of a coin and a vague notion of "patient‑specific considerations".
But let’s be honest: most physicians are racing against insurance formularies, and patients are scrolling through Reddit threads searching for the shinier, newer name that sounds like it belongs in a sci‑fi novel.
Take Minocin, for example-another tetracycline cousin that claims superior tissue penetration, yet still drags along the classic side‑effects cocktail of dizziness, tinnitus, and the ever‑present threat of photosensitivity that turns a sunny day into a hazard.
Then there’s Declomycin, the obscure relic that only surfaces when the usual suspects fail, and even then, it brings with it a legacy of bone‑growth concerns and gastrointestinal unrest that would make a teenager’s stomach churn.
And now we have the sleek, high‑tech Tygacil, a glycylcycline that shouts "I can kill superbugs!" while demanding an IV line, a hospital stay, and a risk profile that reads like a cautionary tale-nausea, hepatic dysfunction, and an unsettling signal of increased mortality for certain patients.
Meanwhile, Xerava joins the parade, promising to pierce through resistant strains, but only if you’re comfortable with the possibility of serious adverse events and the fact that it’s not even an option for kids.
Even the topical champions like clindamycin and tretinoin are tossed into the mix, the former threatening to breed resistant skin flora, the latter being a non‑antibiotic that still demands a strict regimen and sun protection.
All of this sounds like a bureaucratic buffet where the menu changes weekly, and the chef-our beloved pharmaceutical industry-keeps adding exotic ingredients to keep us guessing.
What’s truly astonishing is the sheer confidence with which these drugs are marketed, as if prescribing a new antibiotic is the same as handing out a golden ticket, ignoring the sobering reality that antibiotic stewardship is a collective responsibility, not an individual’s luxury to experiment with the latest hype.
We continue to chase after the next "alternative" while the real battle-preventing resistance, educating patients, and preserving the efficacy of existing drugs-gets sidelined.
In the end, the choice of antibiotic should be grounded in solid microbiological data, patient history, and a dose of humility, not in the flashiness of a brand name or the allure of a novel mechanism that sounds impressive on paper.
So before you jump onto the next hype train, ask yourself if you’re genuinely advancing patient care or merely adding another entry to the ever‑growing list of antibiotics that will one day be rendered obsolete by the very organisms we aim to defeat.
Thank you for the thorough overview; the complexities you highlighted underscore the importance of evidence‑based selection.
When evaluating alternatives to doxycycline, clinicians should prioritize susceptibility data, patient comorbidities, and potential drug‑drug interactions.
For instance, Minocin offers broad coverage but warrants monitoring for vestibular adverse effects, whereas Seysara provides a more targeted approach for acne with a reduced gastrointestinal burden.
In cases of multidrug‑resistant infections, agents such as Tygacil or Xerava may be warranted, provided the setting justifies IV administration and the risk profile is acceptable.
Ultimately, shared decision‑making with the patient, incorporating both clinical efficacy and safety considerations, remains the cornerstone of optimal antibiotic therapy.
Allow me to emphasize, with the gravitas this discussion deserves, that the judicious deployment of any antimicrobial agent is not merely a clinical choice but a moral imperative of our times.
One must interrogate the literature with relentless rigor, balancing the seductive promise of a novel IV‑only agent against the immutable principles of stewardship.
Hence, I assert, with both conviction and decorum, that the onus lies upon us-physicians, pharmacists, and informed patients alike-to eschew the allure of convenience when it threatens the fragile equilibrium of microbial ecology.
Only through disciplined, evidence‑anchored decision‑making can we hope to preserve the potency of our pharmacologic armamentarium for generations to come.