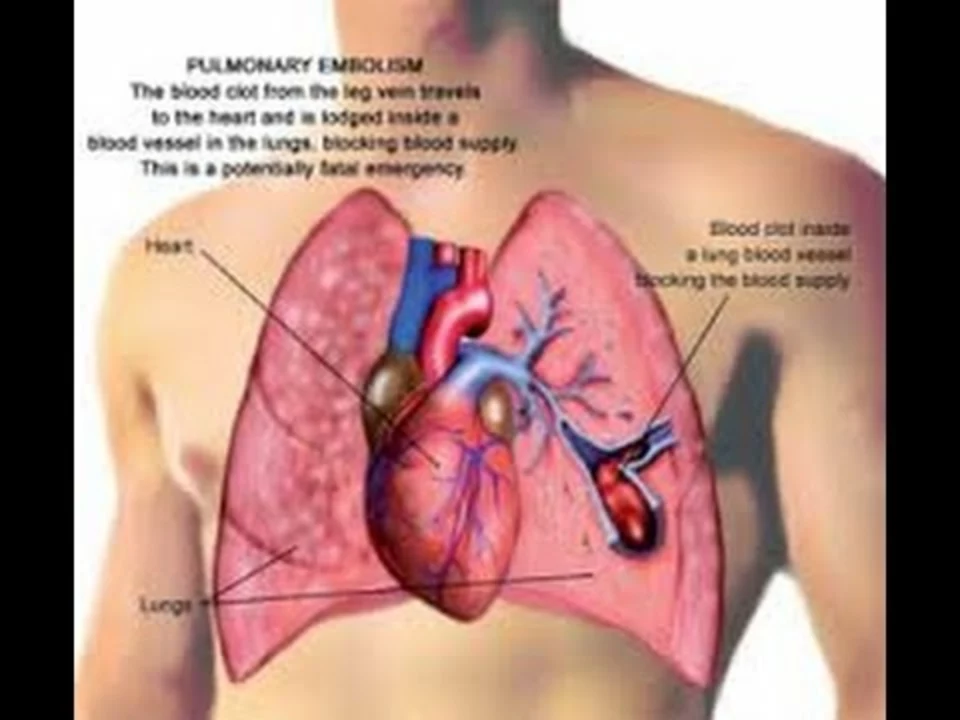
Understanding Pulmonary Embolism and Its Impact
When we talk about pulmonary embolism, it's essential to understand what it is and how it affects our body. Pulmonary embolism is a blockage in one of the pulmonary arteries in your lungs, typically caused by a blood clot. This blockage can hinder blood flow to the lungs and reduce oxygen levels in the body. As a result, it can have severe consequences on our heart and lungs, which are vital organs responsible for pumping blood and supplying oxygen to the body. In this article, we will discuss how pulmonary embolism affects your heart and lungs and the potential complications it can cause.
The Connection Between Pulmonary Embolism and Heart Function
One of the most significant impacts of pulmonary embolism is the stress it places on the heart. When a blood clot blocks the flow of blood in the lungs, the heart has to work harder to pump blood through the remaining vessels. This increased workload can result in higher blood pressure in the pulmonary arteries (pulmonary hypertension) and strain the right side of the heart (right ventricular strain).
Over time, this strain can lead to right heart failure, where the right side of the heart becomes weakened and unable to pump blood effectively. In severe cases, a massive pulmonary embolism can cause sudden death due to the heart's inability to cope with the increased strain. Therefore, it's crucial to recognize the symptoms of pulmonary embolism and seek immediate medical attention to prevent these severe complications.
Effects of Pulmonary Embolism on Lung Function
Aside from the heart, the lungs also suffer the consequences of a pulmonary embolism. The clot obstructs the flow of oxygen-rich blood to the lung tissue, causing the affected area to become oxygen-deprived. This lack of oxygen can lead to the death of lung tissue (pulmonary infarction) and result in decreased lung function.
Moreover, as the blood clot dissolves and the body works to repair the damaged lung tissue, scar tissue may form, further impairing lung function. In some cases, pulmonary embolism can also cause fluid to accumulate in the lungs (pulmonary edema), leading to shortness of breath and reduced lung capacity. All these factors contribute to the debilitating impact of pulmonary embolism on lung function and overall health.
Recognizing the Symptoms of Pulmonary Embolism
Early detection and treatment are crucial in managing the effects of pulmonary embolism on the heart and lungs. Some common symptoms of pulmonary embolism include sudden shortness of breath, chest pain that worsens with deep breathing or coughing, rapid heart rate, lightheadedness, and coughing up blood.
However, it's essential to note that these symptoms can also be indicative of other health issues. Therefore, it's crucial to seek medical help promptly if you experience any of these symptoms, as only a proper diagnosis can determine if you have a pulmonary embolism.
Prevention and Treatment of Pulmonary Embolism
Preventing blood clots in the first place can significantly reduce your risk of developing a pulmonary embolism. Some preventative measures include leading an active lifestyle, maintaining a healthy weight, staying hydrated, and avoiding long periods of immobility, such as during long flights or car rides.
If you are diagnosed with a pulmonary embolism, your healthcare provider will discuss the best course of treatment for you. The primary goal of treatment is to dissolve the blood clot and prevent new clots from forming. This may involve the use of blood-thinning medications, clot-dissolving medications, or, in severe cases, surgical intervention. Your healthcare provider will also work with you to address any underlying risk factors that may have contributed to the development of the blood clot.
In conclusion, pulmonary embolism can have severe consequences on both the heart and lungs. By recognizing the symptoms and seeking prompt medical attention, you can help minimize the impact of this condition on your overall health. Additionally, adopting a healthy lifestyle and addressing any underlying risk factors can significantly reduce your risk of developing a pulmonary embolism in the first place.








13 Comments
If you enjoy playing Russian roulette with your own circulatory system, then congratulations, you’ve found yet another excuse to ignore basic medical advice. The article casually lists risk factors, yet most people still think “I’m fine until I can’t breathe”. Pulmonary embolism isn’t some exotic rarity that belongs only in textbooks; it’s a predictable consequence of sedentary habits and careless travel. By perpetuating the myth that blood clots are “unavoidable”, we absolve ourselves of responsibility for simple preventative measures like moving around on long flights. The heart’s right ventricle becomes a tragic hero only because you chose to binge‑watch series without standing up. In short, if you value your life, stop treating your body like a disposable commodity. So next time you’re tempted to skip that stretch, remember the lungs and heart will thank you, or they’ll file a lawsuit.
First and foremost, it is essential to recognize that early detection significantly improves prognosis in pulmonary embolism cases. Clinicians typically employ a combination of D‑dimer testing, computed tomography pulmonary angiography, and risk‑assessment scores to confirm the diagnosis. In addition, patients should be educated about hallmark symptoms such as sudden dyspnea, pleuritic chest pain, and hemoptysis. Preventive strategies, including regular ambulation, adequate hydration, and weight management, play a pivotal role in mitigating clot formation. Anticoagulant therapy remains the cornerstone of treatment, with options ranging from low‑molecular‑weight heparin to direct oral anticoagulants. Finally, interdisciplinary follow‑up ensures that underlying risk factors, such as thrombophilia or immobilization, are addressed comprehensively.
The interplay between clot formation and cardiac workload invites a deeper philosophical reflection on the fragility of our physiological equilibrium. When a thrombus obstructs a pulmonary artery, the right ventricle faces an abrupt increase in afterload, reminiscent of a sudden mountain climb without preparation. This hemodynamic challenge forces the heart to redistribute blood flow, often at the expense of systemic perfusion, leading to syncope or even shock. The lungs, deprived of proper perfusion, suffer from ventilation‑perfusion mismatch, resulting in hypoxemia that can cascade into organ dysfunction. Moreover, chronic embolic events may give rise to pulmonary hypertension, a condition that rigidly reshapes the vascular architecture over time. Such remodeling not only compromises gas exchange but also imposes a perpetual strain on the right heart, fostering right‑sided heart failure. From a clinical standpoint, recognizing the subtle progression from acute dyspnea to chronic insufficiency can dramatically alter therapeutic outcomes. Anticoagulation, when instituted promptly, disassembles the clot and restores hemodynamic balance, illustrating medicine’s capacity to reverse nature’s abrupt assaults. In cases where massive emboli precipitate circulatory collapse, advanced interventions like catheter‑directed thrombolysis become indispensable. Yet, beyond pharmacology, lifestyle modifications-regular mobility, weight control, and avoidance of prolonged immobility-serve as the first line of defense. The brain, too, must be attuned to the nuanced symptomatology, for chest pain and tachycardia may masquerade as less ominous ailments. Education empowers patients to seek immediate care, thereby reducing the window for irreversible damage. On a broader scale, public health initiatives that promote active travel and hydration can diminish the incidence of venous stasis, the primary nidus for clot genesis. In summary, the cascade from pulmonary embolism to cardiac compromise underscores the intricate interdependence of organ systems. By appreciating this cascade, clinicians and patients alike can intervene early, preserving both heart and lung function for the longevity of life.
The pathophysiology of PE is basically a thrombo‑embolic occlusion that drives up pulmonary vascular resistance, which in turn forces the RV into a pressure‑overload scenario. In layman’s terms, your right heart gets squeezed like a soda can that’s been shaken too hard. This pressure surge can precipitate tricuspid regurgitation and eventually lead to cor pulmonale-yeah, that’s a fancy way of sayin the right side of your heart is failin. Imaging modalities like CTA provide high‑resolution views, but even a bedside echo can reveal RV dilatation and septal flattening. If you’re stuck on a long flight, remember the “move‑your‑legs” rule; it’s not just a myth, it’s a proven VTE prophylaxis. So, defenitely don’t ignore the subtle signs, because the cascade from clot to cardiac strain can happen faster than you think.
Take a deep breath and realize that you have the power to influence your own health outcomes. Understanding the signs of a pulmonary embolism equips you to act decisively, which can be life‑saving. By incorporating simple habits-standing up every hour, staying hydrated, and engaging in regular exercise-you reduce the risk of clot formation. Should symptoms arise, seek immediate medical attention; early intervention dramatically improves recovery prospects. Remember, your heart and lungs are a team; nurturing one benefits the other, and you’re the coach guiding that partnership.
When evaluating a patient for suspected pulmonary embolism, it is useful to apply the Wells criteria alongside a D‑dimer test to stratify risk. A low‑risk profile may allow for outpatient management with direct oral anticoagulants, whereas high‑risk patients often require hospitalization and possible thrombolytic therapy. Additionally, consider underlying hypercoagulable states, such as factor V Leiden, which may necessitate extended anticoagulation. Education about early mobilization after surgery or prolonged travel can further mitigate future events.
Obviously, most people could avoid PE by just moving around a bit more.
It is categorically insufficient to treat pulmonary embolism as a mere inconvenience; the condition epitomizes a systemic derangement of hemostatic equilibrium that demands comprehensive anticoagulant stewardship. The literature unequivocally demonstrates that suboptimal dosing regimens precipitate recurrent thromboembolic phenomena, undermining both morbidity and mortality metrics. Hence, clinicians must adhere to evidence‑based protocols, integrating pharmacogenomic data where applicable, to forestall iatrogenic complications. Anything less betrays a flagrant neglect of professional responsibility.
🚨Listen up, America!🚨 Our great nation cannot afford to have citizens collapsing on the highway because they ignored simple clot‑prevention tips. The pride of the USA is in our vigor, not in lying on the ground gasping for air! 🇺🇸 Move those legs on a 12‑hour flight, drink water, and stop acting like you’re invincible. If you don’t, you’ll be the weak link that drags the whole country down. 💪🏽💥
The article covers the basics but fails to delve into newer anticoagulant options and their comparative efficacy.
While the narrative attempts to outline the cascade from clot formation to right‑ventricular strain it often neglects the subtle interplay between endothelial dysfunction and platelet activation which, in a comprehensive view, are equally pivotal to the pathogenesis of pulmonary embolism and deserve a more nuanced discussion that integrates recent meta‑analyses on direct oral anticoagulants and their impact on long‑term morbidity the omission of such data may lead readers to underestimate the therapeutic advances that have emerged in the last decade thereby perpetuating outdated clinical practices which could be mitigated through continued education and interdisciplinary collaboration
I'm really sorry you’re dealing with this, it can feel overwhelming :( but staying informed and following your doctor’s plan can make a huge difference in recovery.
In response to the earlier admonition regarding personal responsibility, it is pertinent to underscore that patient education must be delivered with both factual precision and compassionate encouragement. Evidence indicates that structured discharge counseling, incorporating visual aids and personalized risk assessments, substantially enhances adherence to prophylactic measures. Moreover, interdisciplinary collaboration among physicians, nurses, and physiotherapists fosters a cohesive strategy that mitigates sedentary behavior during extended travel. Consequently, by integrating these evidence‑based practices, healthcare providers can effectively bridge the gap between awareness and action, thereby reducing the incidence of preventable pulmonary embolic events.