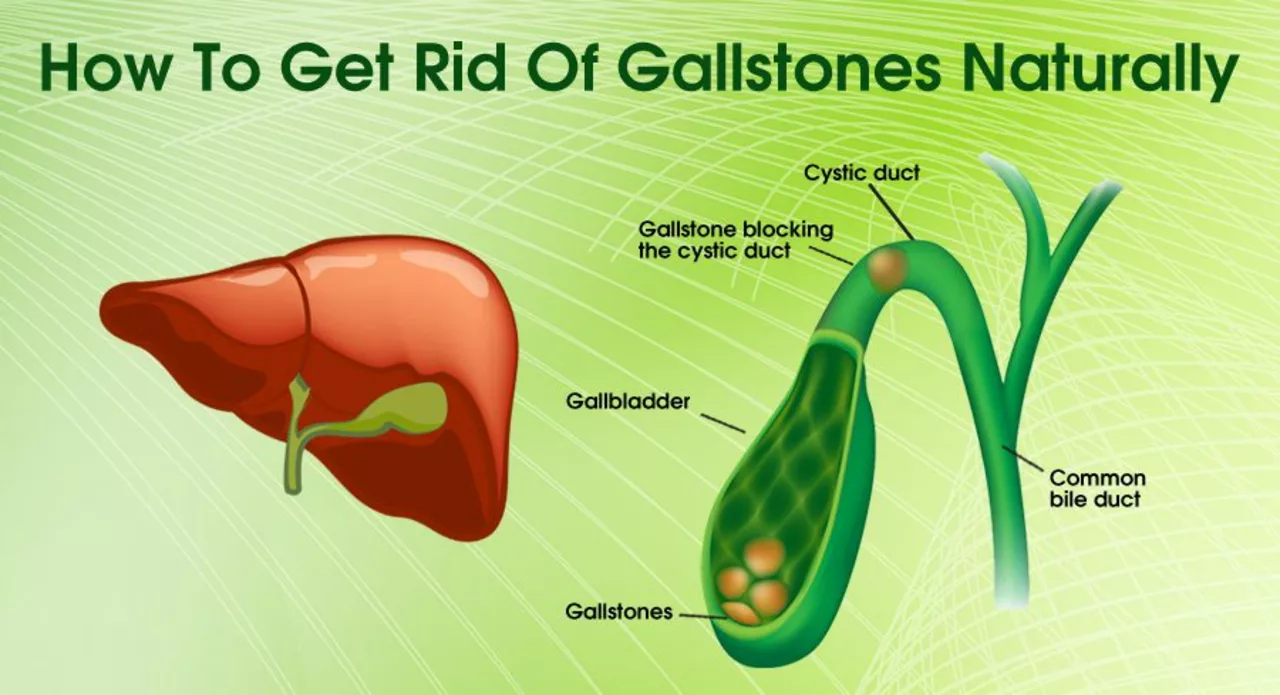
Understanding Gallstones
Gallstones are small, hard deposits that form in the gallbladder, a small organ located under the liver that stores bile. These stones can cause severe pain and discomfort, and may even require surgery for removal. In this article, we will explore the long-term effects of living with gallstones and how they can impact your overall health and well-being.
1. Chronic Pain and Discomfort
One of the most common symptoms of gallstones is chronic pain in the upper right abdomen. This pain can range from mild to severe, and it can even radiate to the back and shoulder. Over time, the constant presence of pain can take a significant toll on your mental and emotional well-being, leading to increased stress and anxiety. Additionally, the pain may cause you to avoid certain activities or social situations, which can further exacerbate feelings of isolation and depression.
2. Increased Risk of Infection
Gallstones can cause blockages in the bile ducts, which can lead to the buildup of bile and an increased risk of infection. If left untreated, these infections can become life-threatening, causing serious complications such as sepsis and pancreatitis. It is crucial to seek medical attention if you suspect an infection, as early intervention can help prevent further complications.
3. Impaired Liver Function
The liver plays a crucial role in processing and detoxifying harmful substances in the body. When gallstones block the flow of bile from the liver, the liver may become unable to effectively filter out toxins. Over time, this can lead to a buildup of harmful substances in the body, causing damage to the liver and other organs. Long-term liver impairment can result in a host of health problems, including cirrhosis and liver failure.
4. Nutrient Malabsorption
Bile plays a key role in the digestion and absorption of fats and fat-soluble vitamins, such as vitamins A, D, E, and K. When gallstones interfere with bile flow, your body may struggle to properly break down and absorb these nutrients. This can lead to deficiencies and a host of health problems, including weakened bones, vision problems, and a weakened immune system.
5. Increased Risk of Gallbladder Cancer
While gallbladder cancer is relatively rare, long-term gallstone sufferers may face an increased risk of developing this type of cancer. The exact link between gallstones and gallbladder cancer is not entirely understood, but chronic inflammation caused by the presence of gallstones is thought to play a role. It is essential to monitor your gallstone symptoms and seek medical attention if you notice any changes in your condition.
6. Complications from Gallstone Surgery
For many people, surgery is the only option for treating gallstones. While most gallstone surgeries are successful, there is always a risk of complications. These can include infection, bleeding, bile leakage, and injury to nearby organs. Additionally, some patients may experience post-surgical complications, such as diarrhea or changes in bowel habits, which can persist for months or even years after surgery.
7. Impact on Mental Health
Living with chronic pain and the constant threat of complications from gallstones can take a significant toll on your mental health. The stress and anxiety associated with gallstones can lead to depression, social isolation, and a reduced quality of life. It is crucial to seek support from friends, family, or a mental health professional if you find yourself struggling to cope with the emotional impact of gallstones.
8. Financial Burden
The cost of treating gallstones can be significant, particularly if surgery is required. In addition to medical bills, there may be indirect costs associated with lost wages, transportation to and from medical appointments, and the need for additional support or caregiving. The financial strain of dealing with gallstones can exacerbate stress and anxiety, making it even more difficult to cope with your condition.
9. Lifestyle Changes
Living with gallstones often requires making significant lifestyle changes to manage your symptoms and reduce the risk of complications. This can include dietary modifications, such as avoiding high-fat foods and incorporating more fiber into your diet, as well as increasing physical activity and maintaining a healthy weight. While these changes can be challenging, they are essential for improving your overall health and well-being.
10. The Importance of Seeking Treatment
While living with gallstones can have several long-term effects on your health and well-being, it is important to remember that treatment options are available. If you are experiencing symptoms of gallstones, it is crucial to seek medical attention promptly. Early intervention can help prevent complications, reduce pain, and improve your overall quality of life. Don't wait to take control of your health—talk to your healthcare provider about the best course of action for managing your gallstones.



12 Comments
Gallstone disease, while often perceived as a mere digestive nuisance, warrants a comprehensive understanding of its systemic ramifications.
Chronic biliary colic, if unmitigated, predisposes patients to heightened sympathetic discharge, which in turn can exacerbate cardiovascular strain.
Moreover, persistent obstruction of the cystic duct fosters a milieu conducive to bacterial overgrowth, thereby increasing the likelihood of ascending cholangitis.
The ensuing inflammatory cascade can compromise hepatic perfusion, subtly impairing the liver's detoxification capacity over years.
Beyond hepatic concerns, the malabsorption of fat‑soluble vitamins-particularly A, D, E, and K-propagates osteopenic changes and coagulopathic tendencies.
These nutrient deficits frequently manifest as nocturnal bone pain, delayed wound healing, and bruising, underscoring the need for vigilant nutritional surveillance.
Patients should therefore be counseled to incorporate vitamin supplementation under medical guidance, especially when surgical cholecystectomy is deferred.
From a psychosocial perspective, the intermittent yet severe pain episodes engender anticipatory anxiety, which can precipitate depressive symptomatology if left unaddressed.
Evidence suggests that cognitive‑behavioral strategies, coupled with appropriate analgesic regimens, alleviate both physical and emotional burdens.
Financial considerations also merit attention; the cumulative cost of imaging, laboratory monitoring, and potential hospitalizations can impose a substantial economic strain.
Insurance navigation and patient assistance programs may mitigate this impact, yet proactive dialogue with healthcare providers remains essential.
In the realm of oncology, chronic inflammation secondary to gallstones has been correlated with a modest yet notable elevation in gallbladder carcinoma risk, reinforcing the imperative for regular ultrasonographic surveillance in high‑risk cohorts.
Should surgical intervention become unavoidable, laparoscopic cholecystectomy offers a favorable safety profile, though patients must be apprised of possible postoperative sequelae such as transient diarrhea or bile duct injury.
Post‑operative dietary modification-favoring low‑fat, high‑fiber meals-facilitates adaptation to altered biliary dynamics and promotes long‑term gastrointestinal health.
Ultimately, an interdisciplinary approach encompassing gastroenterology, nutrition, mental health, and surgery provides the most robust framework for mitigating the long‑term sequelae of gallstone disease.
Engagement in shared decision‑making empowers patients to tailor their therapeutic pathway, thereby enhancing outcomes and quality of life.
It’s astounding how many people continue to ignore basic dietary wisdom and then blame the healthcare system for their own gallstone misery 🙄💢. In a country that prides itself on innovation, we should be cutting the junk foods that fuel these stones, not waiting for surgeons to fix the mess we created. If you’re not willing to adjust your lifestyle, expect the same old complications to haunt you. 🙈
Gallstones can really mess up how you absorb fats. When bile can’t flow, vitamins like D and K suffer. This can lead to weak bones and bruising.
The journey with gallstones isn’t just a physical trial; it’s an invitation to reflect on how we treat our bodies. By choosing mindful eating and gentle movement, we forge resilience that echoes beyond the biliary tract. Hope thrives when we act with intention.
i think the diet change is key.
While your exposition is commendably exhaustive, it neglects the pivotal role of sphincter of Oddi dysfunction in exacerbating biliary stasis. Contemporary literature underscores that dysmotility, rather than mere stone burden, precipitates cholestatic injury. A nuanced therapeutic algorithm should therefore integrate manometric assessment alongside cholecystectomy.
Enough of the whining! If you can’t handle a little gallstone pain, you’re not cut out for the real world 🌍💥. America built itself on grit, not on coddling over every ache. Get serious or get out of the conversation.
just remember staying hydrated and eating more veggies can really help keep those stones at bay
One must not trivialize the complex enterohepatic feedback mechanisms with such simplistic advice 😉. While increased fiber intake is beneficial, a comprehensive regimen-incorporating bile acid sequestrants, periodic ultrasonography, and individualized macronutrient distribution-constitutes a far more sophisticated prophylactic strategy.
The article covers the basics but doesn’t really dive into novel treatment options. It feels a bit surface‑level.
Indeed the superficial overview scarcely scratches the epidermal layer of a multifaceted pathology; gallstone disease, when parsed through the lens of hepatobiliary physiology, unveils a labyrinth of enzymatic interactions, microbiome perturbations, and genetic predispositions that demand rigorous scholarly inquiry. One cannot simply accept a cursory summary without interrogating the underlying mechanistic pathways-cholesterol supersaturation, nucleation factors, and gallbladder dysmotility-each of which orchestrates the chrono‑logical progression from asymptomatic microlithiasis to overt clinical syndrome. Moreover, emerging data on bile acid analogs and targeted molecular therapies portend a paradigm shift away from indiscriminate cholecystectomy toward precision medicine. To neglect these advancements is to consign patients to antiquated management and to perpetuate avoidable morbidity.
i totally get how overwhelming this can feel 😊. If you’re struggling, reaching out to a dietitian or a support group can make a huge difference. don’t hesitate to ask for help.