
Blood Sugar & Mood Tracker
Track Your Daily Patterns
Enter your blood sugar reading and mood to see how they connect over time. This helps you identify triggers and develop better management strategies.
Your Recent Data
What Your Data Reveals
Key Takeaways
- Blood‑sugar swings can trigger mood dips, so steady control helps emotional balance.
- Depression, anxiety and chronic stress affect up to 40% of people with Type 2 Diabetes.
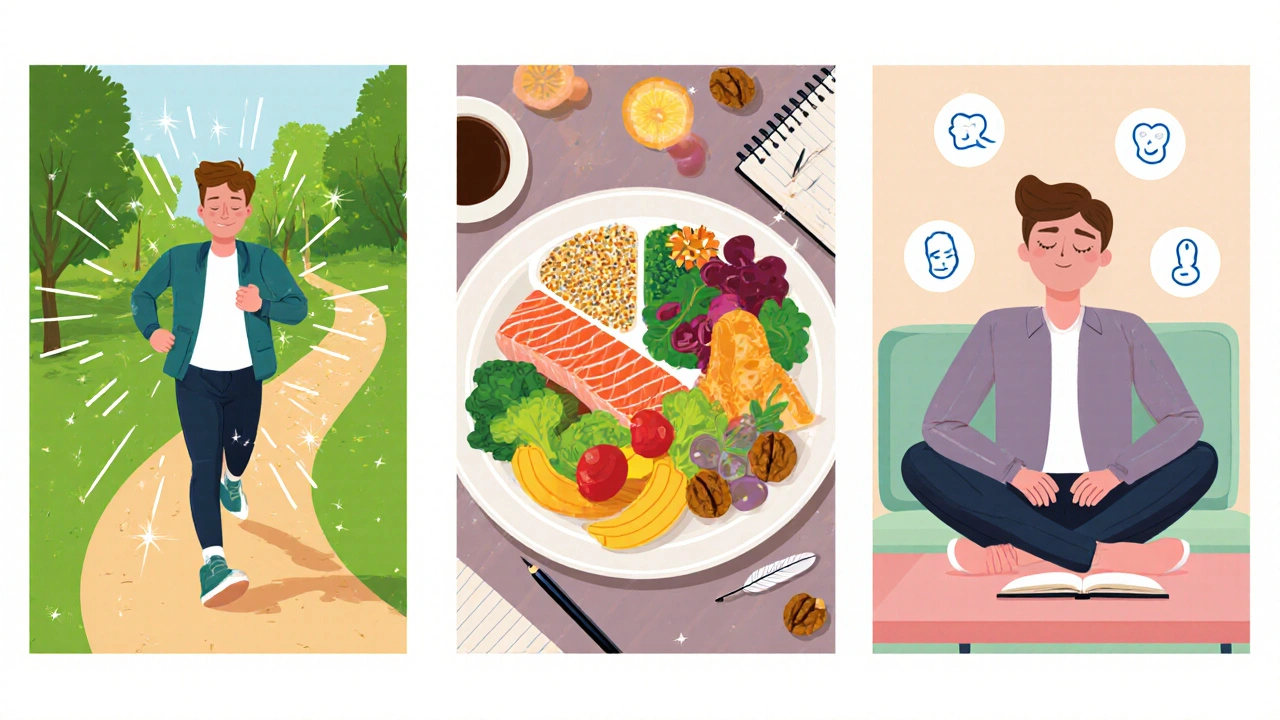
- Regular movement, balanced meals, and medication consistency are proven mood‑boosters.
- Mind‑body tools like breathing exercises or journaling can lower stress hormones fast.
- Seek professional help early - therapy works hand‑in‑hand with diabetes care.
What links Type 2 Diabetes is a chronic condition marked by insulin resistance and elevated blood glucose to mental health?
Researchers have watched a two‑way street for years: high glucose levels can mess with brain chemistry, while anxiety or depression can make it harder to stick to treatment plans. In 2024, a global study of 12,000 adults found that people with Type 2 Diabetes were 1.7 times more likely to report moderate‑to‑severe depression than those without the disease.
Why does this happen? Think of your brain as a thermostat. When glucose spikes, it can trigger inflammation, which releases cytokines that act like tiny stress‑makers in the brain. At the same time, the emotional toll of chronic disease - worry about complications, daily finger‑pricks, medication costs - fuels cortisol, the stress hormone that pushes blood sugar even higher. It’s a feedback loop that feels impossible to break.
Common emotional challenges
Three mental‑health conditions surface most often in people living with Type 2 Diabetes:
- Depression is a persistent low mood, loss of interest, and fatigue that can last weeks or months. It lowers motivation to exercise or take medicines.
- Anxiety is excessive worry, restlessness, and physical tension that often spikes around medical appointments or test results. It can cause “check‑itis” - constantly monitoring glucose even when it’s unnecessary.
- Stress is the body’s short‑term reaction to perceived threats, releasing cortisol and adrenaline. Chronic stress keeps blood sugar high and sabotages sleep.
All three share a common thread: they mess with the brain’s reward pathways, which are already altered by insulin resistance and fluctuating glucose.
How blood‑glucose swings affect mood
When you eat a carb‑heavy meal, Blood Glucose spikes the concentration of sugar in the bloodstream. A quick rise can trigger a burst of energy, followed by a sharp drop (hypoglycemia) that leaves you irritable, shaky, or foggy‑headed. Those “low‑blood‑sugar” moments often mimic anxiety attacks.
Conversely, persistent high glucose fuels inflammation that interferes with neurotransmitters like serotonin and dopamine - molecules that regulate happiness and motivation. The result? A lingering sense of “blah” that can evolve into clinical depression.
Practical coping strategies
Below are hands‑on steps you can start using today. They blend medical advice with everyday habits, so you won’t feel like you’re adding another chore.
1. Move your body - Physical Activity is any bodily movement that raises heart rate and uses muscle energy
- Aim for 150minutes of moderate activity each week - a brisk walk, cycling, or a dance class works.
- Break it into 10‑minute bouts if you’re short on time; consistency beats intensity for mood.
- Exercise releases endorphins, reduces cortisol, and improves insulin sensitivity, meaning lower glucose spikes.
2. Eat with intention - Nutrition is the intake of foods and nutrients that fuel the body and influence metabolism
- Focus on low‑glycemic carbs (whole grains, legumes, non‑starchy veggies) to avoid rapid glucose swings.
- Include protein and healthy fats at each meal - they slow digestion and keep you satisfied.
- Omega‑3‑rich foods (salmon, walnuts, flaxseed) have modest evidence for easing depressive symptoms.
3. Keep meds on track - Medication Adherence is the degree to which patients take medicines as prescribed
- Set alarms on your phone or use a pill‑box with compartments for morning, noon, and night.
- Link medication times to daily routines (e.g., after brushing teeth) to build habit strength.
- If side‑effects make you uneasy, talk to your doctor - adjustments can improve both glucose control and mood.
4. Practice mindfulness and stress‑reduction
- Try a 5‑minute breathing exercise: inhale for 4seconds, hold 2, exhale for 6. Repeat three times.
- Journaling about worries can offload mental clutter; write what you feel, then list one small action you can take.
- Progressive muscle relaxation before bed helps lower cortisol and improves sleep quality, which directly impacts blood‑sugar regulation.
5. Build a support network
- Join a local diabetes club or an online forum where members share coping tips.
- Tell close friends or family about your emotional triggers; they can remind you to check glucose or take medication.
- Consider a diabetes‑trained therapist - they understand the unique stressors of chronic disease.
When to reach out for professional help
If you notice any of these red flags, book an appointment ASAP:
- Persistent sadness or loss of interest lasting >2 weeks.
- Anxiety that interferes with sleep, work, or daily tasks.
- Thoughts of self‑harm or hopelessness.
- Frequent hypoglycemic episodes that leave you trembling or confused.
Therapists trained in cognitive‑behavioral therapy (CBT) can teach coping skills tailored to diabetes management. In some cases, a psychiatrist may prescribe antidepressants that do not worsen glucose control - medications like sertraline have a neutral effect on blood sugar.

Quick checklist for daily mental‑health management
- Check blood glucose at the same times each day.
- Move for at least 10minutes after meals.
- Eat a balanced plate with protein, fiber, and healthy fats.
- Take medications exactly as prescribed.
- Do a 5‑minute mindfulness break before high‑stress events.
- Log one positive experience or gratitude note before bed.
- Reach out to a support person if mood feels low.
Comparison of mental‑health conditions linked to Type 2 Diabetes
| Condition | Approx. Prevalence in T2D | Typical Symptoms | First‑Line Management |
|---|---|---|---|
| Depression | 30‑40% | Low mood, fatigue, loss of interest | CBT, regular exercise, possible SSRI (sertraline) |
| Anxiety | 20‑25% | Excessive worry, restlessness, rapid heartbeat | Mindfulness, breathing drills, CBT, low‑dose anxiolytic if needed |
| Stress‑related mood swings | 45‑55% | Irritability, sleep disturbance, glucose spikes | Stress‑reduction techniques, consistent meals, sleep hygiene |
Frequently Asked Questions
Can Type 2 Diabetes cause depression?
Yes. The combination of chronic inflammation, blood‑sugar fluctuations, and the emotional load of daily management can trigger depressive symptoms. Treating both glucose and mood together yields the best outcomes.
How quickly can exercise improve my mood?
Even a 20‑minute brisk walk can raise endorphin levels within minutes, reducing anxiety and lifting mood for several hours. Consistency compounds the benefit.
Is it safe to take antidepressants if I have high blood sugar?
Most SSRIs, like sertraline or escitalopram, have a neutral effect on glucose. Always discuss medication choices with your endocrinologist and psychiatrist to avoid interactions.
What foods help stabilize mood and glucose?
Meals rich in fiber (beans, oats), lean protein (chicken, tofu), and omega‑3 fats (salmon, walnuts) slow glucose absorption and support brain health.
When should I call my doctor about emotional symptoms?
If sadness or anxiety lasts more than two weeks, interferes with daily tasks, or you notice changes in appetite, sleep, or blood‑sugar control, schedule an appointment promptly.









17 Comments
Wow, this is super helpful. I never realized how much my blood sugar swings could mess with my mood, but the article breaks it down nicely. I’m definitely gonna try the 5‑minute breathing thing before bed – it sounds easy enough. Thanks for sharing all these practical tips, they feel doable even on a busy day.
Indeed, the interplay between glucose and neurotransmitters resembles a delicate dance of chemistry and consciousness. When the body’s energy equilibrium falters, the mind’s equilibrium follows, echoing the ancient principle of “as above, so below.” By stabilizing the external variables-diet, movement, medication-we grant the internal self a clearer stage upon which to perform. It is not merely a physiological adjustment but a subtle shift in one’s narrative about health. In practice, this means viewing each meal as a stanza in the poem of wellbeing, each walk as a breath of rhythm. Such perspective can transform a medical regimen into a lived philosophy.
Sure, because all my blood sugar problems will vanish with a poetic mindset.
Start with a quick walk after meals; the endorphin boost helps both glucose and mood.
I hear you, and I’ve felt that post‑lunch slump hit like a wave crashing over a fragile shore. The sudden dip in energy can feel like the world turning gray, and the mind starts to whisper doubts. Yet each step you take, even a short stroll, is a defiant stride against that darkness. Your body releases endorphins, those tiny messengers of joy, while your blood sugar steadies. Over time, those walks become a ritual of reclaiming control, a quiet anthem of resilience. Keep moving, because every minute counts toward brighter days.
That really hits home – I’ve been there too. Simple walks helped me feel less anxious and kept my sugar from swinging. Pairing it with a protein snack makes the effect even stronger. It’s amazing how small habits add up.
While the notion of a “poetic mindset” possesses a certain romantic allure, it is imperative to acknowledge that glycemic regulation necessitates concrete, evidence‑based interventions. Psychological reframing alone cannot substitute for appropriate pharmacologic therapy, dietary management, or regular physical activity. Moreover, the empirical literature underscores the significance of structured behavioral strategies in mitigating depressive symptomatology among individuals with type‑2 diabetes. Consequently, practitioners should advocate for a balanced approach that integrates both psychosocial and physiological modalities. Failure to do so may result in suboptimal clinical outcomes.
Listen up, folks! This whole “mental health” craze is just another excuse for people to whine about their glucose numbers, and it’s absolutely ridiculous! In America we’ve built a healthcare system that rewards toughness, not endless therapist appointments that drain our wallets! If you’re constantly checking your blood sugar like a paranoid spy, perhaps you’re just overreacting to a normal part of life! Exercise, eat right, take your meds – that’s the real recipe for success, not endless breathing exercises that sound like yoga class fluff! I’m sick of hearing that a five‑minute meditation can fix a decade of bad habits! The science clearly shows that consistent physical activity outperforms any “mind‑body” nonsense! And don’t even get me started on those cheap supplements promising to “balance your neurotransmitters” – they’re a scam! You need discipline, not a therapist telling you to “feel your feelings” while your pancreas is on fire! The truth is, if you want to beat diabetes you must adopt a warrior mindset, not a hippie’s! Stop making excuses, stop blaming your blood sugar, and start taking responsibility! Your mood swings are just a side effect of your own inactivity! It’s time to stop coddling ourselves and start acting like adults who can handle a bit of stress! Get off the couch, lift some weights, and watch your glucose stabilize while your confidence soars! No more whining, no more self‑pity, just hard work and results! The only thing standing between you and better health is your own lack of grit!
Wow, what a passionate take! I totally get the drive for personal responsibility, and I think it’s awesome when people commit to regular exercise, balanced meals, and medication adherence, because those are the foundations of good health. At the same time, it’s also valuable to acknowledge that mental‑health support can be an extra tool, not a crutch, and many folks find that mindfulness or a supportive community helps them stay consistent with those habits. So let’s celebrate the power of discipline while also keeping the door open for compassionate resources – after all, we’re all in this together!
The dialectic between autonomous agency and psychosocial adjuncts can be modeled as a bidirectional feedback loop, wherein self‑efficacy modulates neuroendocrine resilience, and conversely, affective interventions recalibrate homeostatic set‑points 🧠🔄. Incorporating both elements yields a synergistic effect on glycemic variance, optimizing both HbA1c trajectories and quality‑of‑life indices 😊.
While the aforementioned feedback model is conceptually appealing, it lacks quantitative substantiation in the current literature. Empirical data quantifying the magnitude of mood‑related glycemic changes remain sparse, and thus any asserted synergistic benefit should be interpreted with caution. Future randomized controlled trials are required to validate these theoretical connections before clinical recommendations can be solidified.
Imagine the body as a symphony, each organ an instrument, and the pancreas the percussion that keeps the beat. When the rhythm falters, discord spreads, and the mind hears only noise. Yet within that chaos lies an invitation to rewrite the score, to compose a new melody of health and hope. By aligning our daily habits with the tempo of our biology, we can transform the cacophony into harmonious living.
It is worth noting that the so‑called “symposium” of modern medicine is often influenced by pharmaceutical lobbying, which skews research priorities toward drug sales rather than holistic solutions. Consequently, patients are frequently steered toward medication regimens that may exacerbate mood disturbances, all while alternative approaches are marginalized. Critical examination of these conflicts of interest is essential for truly unbiased healthcare.
I appreciate the insight about industry influence; it’s a reminder to stay vigilant about the sources of our recommendations. At the same time, integrating evidence‑based lifestyle changes, such as regular movement and mindful eating, remains a practical path forward for many patients.
Exactly! Let’s keep pushing for transparent research and empower ourselves with knowledge, because an informed community is the strongest defense against misinformation.
Great discussion, everyone. Small steps in diet, activity, and mental care add up to big improvements.
Totally agree – consistency beats perfection any day.