Gallstones: How to Spot Them and What to Do
Sharp pain under your right ribs after a fatty meal? That’s one of the classic signs of gallstones. They’re very common — many people have them without symptoms, but when a stone blocks the bile flow you’ll notice. This guide gives plain answers: what causes gallstones, how doctors check for them, treatment options, and when to seek urgent care.
What causes gallstones and who gets them
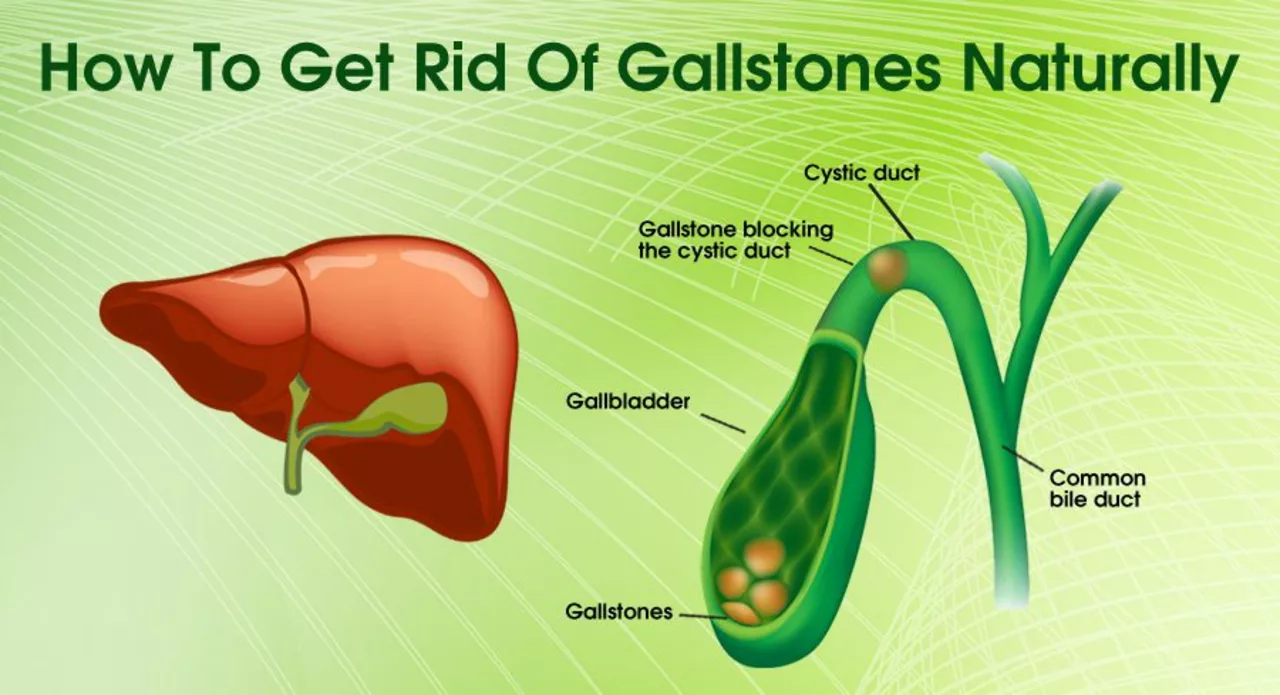
Gallstones form when the substances in bile harden. Two main types exist: cholesterol stones (most common) and pigment stones. Risk factors include being female, older age, overweight, rapid weight loss, pregnancy, certain meds and some genetic traits. You don’t need all those factors — just one can raise the chance.
Many people have silent gallstones that never cause trouble. Others get "biliary colic" — a cramping or steady pain in the right upper belly that can last from minutes to hours, often after fatty foods. Nausea, vomiting, and belching are common. If you also have fever, yellow skin or dark urine, that’s a red flag for complications.
Tests, treatments, and what to expect
Ultrasound is the first test. It’s quick and reliable for spotting stones in the gallbladder. Blood tests check for infection or blocked bile ducts. If the ultrasound is unclear, doctors may order a HIDA scan, CT, or MRCP. For stones stuck in the bile duct, ERCP can both diagnose and remove them.
Treatment depends on symptoms. If you have no symptoms, most doctors recommend watchful waiting. For pain attacks or complications, the usual treatment is laparoscopic cholecystectomy — removing the gallbladder. It’s a common, generally safe surgery and most people recover within a week to two weeks. If there’s acute infection of the gallbladder, antibiotics are used first and surgery often follows once you’re stable.
There are non-surgical options in select cases: ursodeoxycholic acid can dissolve some cholesterol stones over months, and shock-wave lithotripsy is rarely used. These are for people who can’t have surgery or have small, specific stones.
How to reduce future risk: aim for a steady, healthy weight rather than crash diets; eat balanced meals with moderate fat; stay active. If you have recurring attacks, talk to your doctor about surgery — repeated episodes can lead to cholecystitis, cholangitis, or pancreatitis, which need urgent care.
When to seek help now: severe, constant right upper pain; fever with chills; yellowing skin or eyes; repeated vomiting; or fainting. Those signs suggest an infection, blocked bile duct, or pancreatitis — all need prompt medical attention.
Quick practical tip: during a pain attack, avoid large fatty meals, use a heating pad for comfort, and check with a provider about pain control. Keep a record of when attacks happen and what you ate; that helps your doctor decide the next steps.
If you want detailed medical articles on gallbladder infections, antibiotics, or surgical options, look for resources that explain tests, recovery timelines, and what to expect after cholecystectomy. Clear info helps you make smart choices about care.
The Long-Term Effects of Living with Gallstones
Living with gallstones can have significant long-term effects on our health and well-being. Over time, these tiny deposits in our gallbladder can cause chronic pain and inflammation, making daily activities and enjoying food a challenge. In some cases, untreated gallstones can lead to more severe complications like gallbladder infection or pancreatitis. Furthermore, the constant discomfort can negatively impact our mental health, leading to increased stress and anxiety. It's essential to consult with a healthcare professional and explore treatment options to alleviate these long-term consequences and improve our quality of life.
read more