Introduction: Understanding Pulmonary Arterial Hypertension and Thyroid Disorders
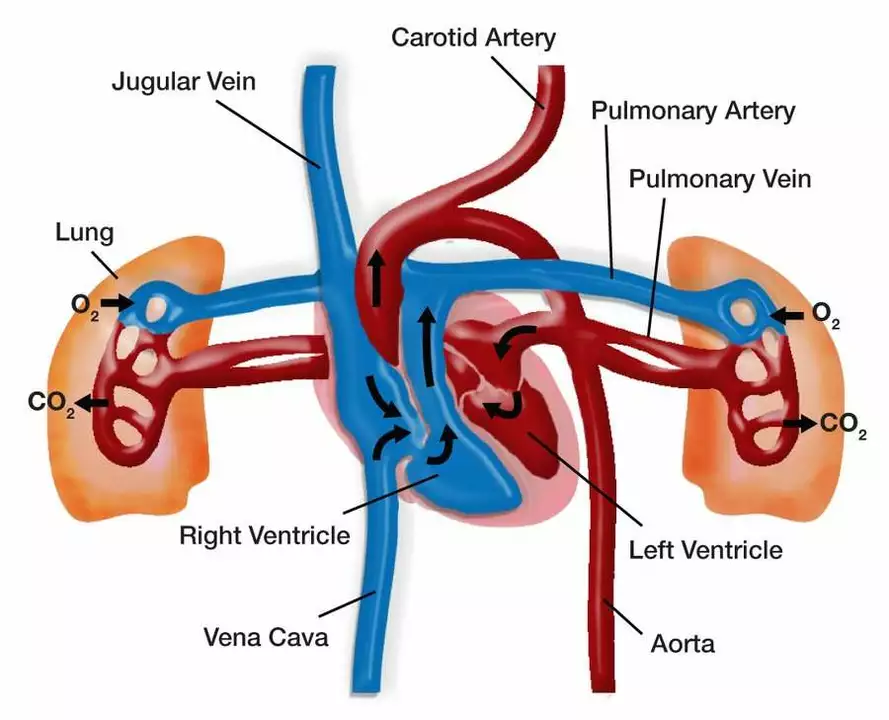
As a blogger passionate about health, I am here to discuss the connection between pulmonary arterial hypertension (PAH) and thyroid disorders. PAH is a condition characterized by high blood pressure in the arteries of the lungs, which can cause shortness of breath, fatigue, and chest pain. On the other hand, thyroid disorders involve the malfunction of the thyroid gland, which is responsible for producing hormones that regulate our metabolism. In this article, we will explore the relationship between these two conditions and how they can impact one another.
Exploring the Link Between PAH and Thyroid Disorders
Research has shown that there is a connection between PAH and thyroid disorders. Studies have found that people with PAH are more likely to have thyroid disorders, such as hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid). Moreover, it has been demonstrated that the presence of a thyroid disorder can increase the severity of PAH, making it essential to address both conditions simultaneously for optimal management and treatment.
How Thyroid Hormones Affect Pulmonary Arterial Hypertension
Thyroid hormones play a crucial role in regulating various bodily functions, including metabolism, growth, and development. They also have a direct impact on the cardiovascular system by influencing heart rate, blood pressure, and vascular tone. When thyroid hormone levels are too low (hypothyroidism) or too high (hyperthyroidism), it can lead to abnormal cardiovascular function, including changes in blood pressure and heart rate. These changes can contribute to the development or worsening of PAH, as both conditions involve the narrowing and stiffening of the pulmonary arteries, leading to increased pressure in the lungs.
Recognizing the Symptoms of PAH and Thyroid Disorders
It is essential to be aware of the symptoms associated with both PAH and thyroid disorders to seek appropriate medical care. The common symptoms of PAH include shortness of breath, fatigue, chest pain, dizziness, and swelling in the legs or ankles. Meanwhile, symptoms of hypothyroidism may include weight gain, fatigue, depression, and sensitivity to cold, while hyperthyroidism can cause weight loss, nervousness, irritability, and increased heart rate.
Diagnosing and Treating PAH and Thyroid Disorders
If you suspect that you may have PAH or a thyroid disorder, it is crucial to consult with a healthcare professional for proper diagnosis and treatment. PAH can be diagnosed through a series of tests, including echocardiography, right heart catheterization, and pulmonary function tests. Similarly, thyroid disorders can be diagnosed through blood tests that measure levels of thyroid hormones and thyroid-stimulating hormone (TSH). Once a diagnosis is confirmed, your healthcare provider will determine the most appropriate treatment options to manage both conditions effectively.
The Importance of Regular Monitoring and Adjusting Treatments
As both PAH and thyroid disorders can have a significant impact on your health, it is crucial to regularly monitor your condition and adjust your treatment plan accordingly. This may involve routine blood tests to check thyroid hormone levels, as well as routine follow-up appointments with your healthcare provider to assess the effectiveness of your treatment plan. By staying proactive in managing both conditions, you can significantly improve your quality of life and reduce the risk of complications.
Lifestyle Changes to Support Healthy Thyroid Function and Manage PAH
In addition to medical treatment, adopting a healthy lifestyle can also help manage PAH and support proper thyroid function. This can include eating a well-balanced diet rich in fruits, vegetables, whole grains, and lean protein sources, as well as getting regular exercise to promote cardiovascular health. Moreover, managing stress, getting sufficient sleep, and avoiding smoking are essential for overall well-being and can contribute to better management of both PAH and thyroid disorders.
Conclusion: Taking a Holistic Approach to Manage PAH and Thyroid Disorders
In summary, there is a clear connection between pulmonary arterial hypertension and thyroid disorders, with each condition potentially exacerbating the other. It is essential to be aware of the symptoms associated with both conditions, seek appropriate medical care for accurate diagnosis and treatment, and adopt a healthy lifestyle to support overall well-being. By taking a holistic approach to managing both PAH and thyroid disorders, you can significantly improve your quality of life and reduce the risk of complications. Remember, your health is in your hands, and being proactive in managing your conditions will help you live a happier, healthier life.








6 Comments
Clearly you’ve never dealt with real PAH patients, so this fluff is pointless.
I totally get how overwhelming it can feel when both your lungs and thyroid act up 😢. Remember to keep your doc’s in the loop and maybe jot down daily symptoms – it really helps.
It's astonishing how many self‑proclaimed health bloggers decide to sprinkle questionable correlations across their pages without a shred of critical appraisal. You claim there's a connection between PAH and thyroid disorders, yet you present it as if it's a groundbreaking revelation, ignoring decades of endocrine and cardiopulmonary research. The average reader deserves more than a cursory nod to “studies have shown” without citations that survive a simple PubMed search. Moreover, tying together two complex diseases with a generic call for “holistic management” feels like a lazy way to avoid discussing the real, nuanced treatment algorithms. Patients with pulmonary arterial hypertension cannot afford vague platitudes when their survival hinges on precise vasodilator therapy and rigorous right‑heart catheterization. Likewise, hypothyroid or hyperthyroid patients deserve targeted hormone replacement strategies, not a blanket “monitor your labs” suggestion that sounds like a checklist for the indifferent. If you truly care about your audience, you would differentiate between the pathophysiological mechanisms-such as the impact of thyroid hormone on endothelial function-rather than lumping them together under a nebulous banner. And let us not forget the socioeconomic barriers that prevent many from accessing the specialized care you so casually assume is universally available. By glossing over these barriers, you implicitly endorse a privileged perspective that marginalizes the very people who need the most concrete guidance. Sarcasm aside, the medical community expects us to uphold evidence‑based standards, not to peddle half‑baked narratives for clicks. It would be a modest improvement if you cited at least two peer‑reviewed articles and explained their relevance in plain language. Readers could then discern whether the “link” you mention is a statistically significant association or merely an anecdotal observation. In short, stop treating complex disease interplay as a marketing gimmick and start treating it with the rigor it deserves. The next time you write about such serious conditions, consider consulting a cardiologist or an endocrinologist before publishing. Otherwise, you risk becoming the author of misinformation, and that is a legacy no conscientious writer should accept. In conclusion, your enthusiasm is commendable, but enthusiasm alone does not substitute for scholarly integrity.
Thank you for bringing attention to a topic that often goes overlooked in routine clinical practice. Pulmonary arterial hypertension and thyroid dysfunction share several pathophysiological pathways, including endothelial dysfunction and metabolic dysregulation, which merit careful evaluation. Patients presenting with unexplained dyspnea should be screened for both conditions, as early identification can markedly improve therapeutic outcomes. Coordination between cardiology and endocrinology teams ensures that treatment regimens are optimized without adverse drug interactions. I encourage readers to discuss these considerations with their healthcare providers and to maintain regular follow‑up appointments for comprehensive care.
Indeed, the intertwining of cardiopulmonary and endocrine systems demands a multidisciplinary approach that cannot be overstated. By asserting the necessity of collaborative care, we underscore the gravity of managing such complex patients. Let us, therefore, champion systematic screening protocols and foster communication across specialties. Ultimately, this rigor will translate into tangible improvements in patient longevity and quality of life.
Only a half‑baked American health blog would try to mash up two serious diseases and call it science 🤦♀️. Real experts know better, so stick to the facts or stay silent.