CKD Medication Guide Calculator
Enter Your eGFR
When you have both Type 2 Diabetes and Chronic Kidney Disease (CKD), choosing the right medications isn’t just about lowering blood sugar-it’s about protecting your kidneys and avoiding dangerous side effects. For years, doctors avoided metformin in CKD patients because of fears of lactic acidosis. SGLT2 inhibitors were once limited to people with decent kidney function. But that changed. The science now shows these drugs aren’t just safe-they’re life-saving. And the rules for using them have been rewritten.
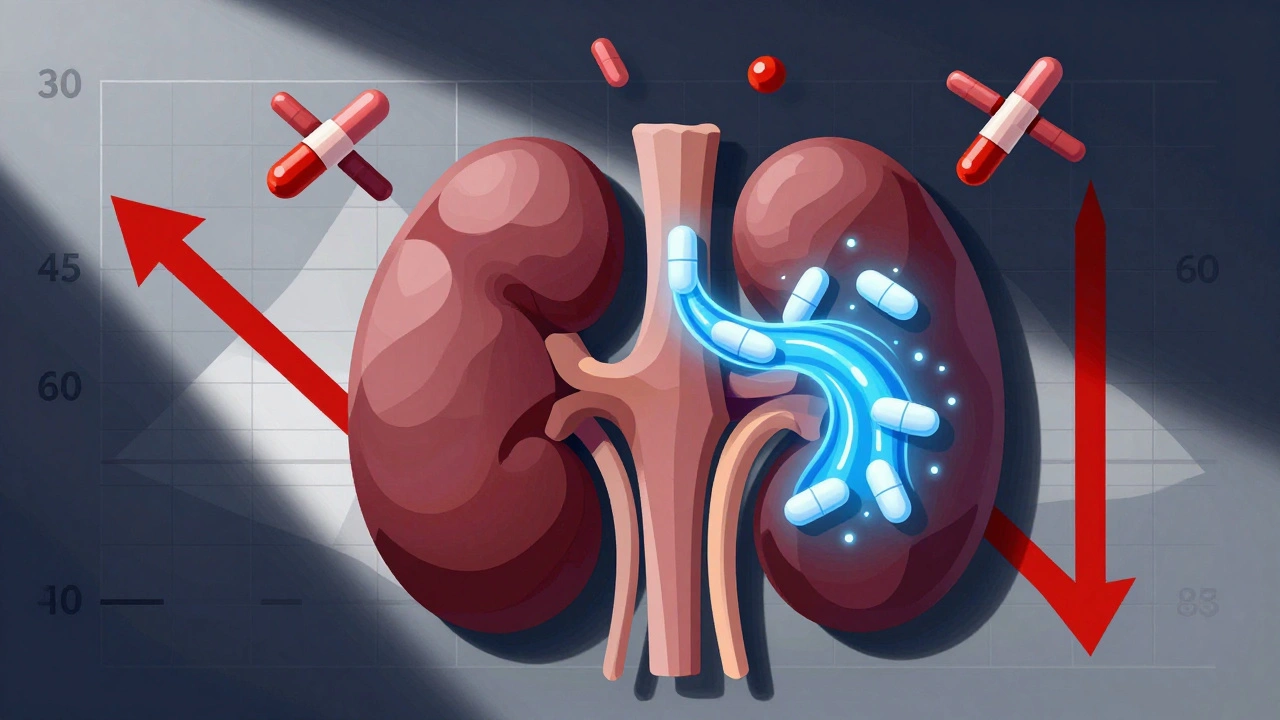
Metformin in CKD: The Old Rules Are Out
Before 2016, metformin was banned if your eGFR dropped below 60 mL/min/1.73 m². By 2020, that limit was still 45. Today? You can take it safely even if your eGFR is as low as 30. The KDIGO 2022 guidelines, backed by data from over 28,000 patient-years, made this shift official. The key isn’t avoiding metformin-it’s adjusting the dose.
Here’s how it works in practice:
- eGFR ≥60: Standard dose-up to 2,000 mg daily, split into two doses.
- eGFR 45-59: Max 1,000 mg per day. Don’t push higher, even if your blood sugar isn’t where you want it.
- eGFR 30-44: Still safe, but max dose stays at 1,000 mg daily. No need to stop unless something else changes.
- eGFR below 30: Stop metformin. This includes patients on dialysis.
Why the change? Studies like the EMPA-REG OUTCOME and DAPA-CKD showed no increase in lactic acidosis when metformin was used within these updated limits. The FDA removed its black box warning in 2016-not because the risk vanished, but because it’s now understood and manageable. The real danger? Not taking metformin when you should. People with CKD and diabetes who avoid metformin have higher rates of heart failure and death.
SGLT2 Inhibitors: The New Foundation of Kidney Care
If metformin is the old workhorse, SGLT2 inhibitors are the game-changer. These drugs-dapagliflozin, empagliflozin, canagliflozin, ertugliflozin-don’t just lower blood sugar. They reduce heart failure, slow kidney decline, and cut the risk of dying from kidney or heart problems. The evidence is so strong, KDIGO now calls them foundational therapy.
The biggest shift? You can now start them even if your eGFR is 20 mL/min/1.73 m². That’s a huge jump from the old limit of 30. And here’s the kicker: you can keep taking them even if your eGFR drops below 20. In the DAPA-CKD trial, 11% of participants had eGFR between 25 and 30 at the start-and they still benefited. The EMPA-KIDNEY trial (2023) confirmed this: empagliflozin reduced kidney failure or cardiovascular death by 28% in patients with eGFR as low as 20.
Effective doses don’t need to be high:
- Dapagliflozin: 10 mg daily
- Empagliflozin: 10 mg daily
- Canagliflozin: 100 mg daily
- Ertugliflozin: 5 mg daily
Higher doses don’t give better kidney protection. They just raise the risk of side effects. Stick to the lowest effective dose.
Safety First: What to Watch For
Both drugs are safe when used right-but they come with risks you can’t ignore.
Metformin risks: Lactic acidosis is rare-3 to 10 cases per 100,000 patient-years in the general population. But in CKD patients with eGFR under 30, that jumps to 10-50 per 100,000. The real danger isn’t steady-state CKD-it’s acute kidney injury. If you get sick, dehydrated, or have a heart attack, your eGFR can drop fast. That’s when metformin becomes risky. Always pause it during acute illness.
SGLT2 inhibitor risks: Most common side effect? Genital yeast infections. About 4-5% of women and 1-2% of men get them. Good hygiene and keeping blood sugar under control help. More serious? Euglycemic diabetic ketoacidosis (euDKA). It’s rare-0.1-0.2%-but it happens. You don’t need to be super high on sugar. Your blood sugar might only be 150-250 mg/dL, but your body starts burning fat for fuel. If you feel nauseous, have abdominal pain, or feel unusually tired, check for ketones. Stop the drug and call your doctor.
Volume depletion is another concern. SGLT2 inhibitors make you pee out more sugar, salt, and water. If you’re older, on diuretics, or already low on fluids, you might feel dizzy or faint. Drink water. Avoid alcohol. Check your blood pressure.

Combining Metformin and SGLT2 Inhibitors: The Gold Standard
For most people with T2D and CKD, the best first-line combo is metformin + an SGLT2 inhibitor. KDIGO 2022 gives this a strong 1A recommendation. Why? Because together, they do more than either drug alone.
Metformin lowers liver glucose production and improves insulin sensitivity. SGLT2 inhibitors make your kidneys dump sugar and reduce blood pressure, inflammation, and kidney pressure. The combination cuts heart failure hospitalizations by nearly half in some studies.
But don’t just add them blindly. If you’re also on insulin or sulfonylureas, you’re at risk for low blood sugar. The UK Kidney Association recommends cutting sulfonylurea or insulin doses by 20-50% when you start an SGLT2 inhibitor-especially if your HbA1c is already below 58 mmol/mol (7.5%).
Monitoring: It’s Not Optional
These drugs aren’t set-and-forget. You need to track your kidney function and watch for warning signs.
- eGFR checks: Every 3-6 months if stable. Every 1-2 months if eGFR is below 45 or if you’re sick.
- Metformin: Stop immediately if eGFR drops below 30. Restart only after kidney function returns to above 45 and the cause of the drop is resolved.
- SGLT2 inhibitors: Check for genital infections monthly in the first 3 months. Monitor blood pressure and hydration. Test for ketones if you feel unwell.
- Potassium: If you’re also on a mineralocorticoid receptor antagonist like finerenone, check potassium 4 weeks after starting, then every 3-6 months. Hold finerenone if potassium hits 5.5 mmol/L or higher.
Many doctors still don’t know the new rules. A 2022 survey found only 34% of primary care doctors knew the correct eGFR thresholds. After a 60-minute training, that jumped to 78%. If your doctor says, “You can’t take SGLT2 inhibitors if your kidneys are bad,” they’re working off outdated info. Point them to KDIGO 2022.
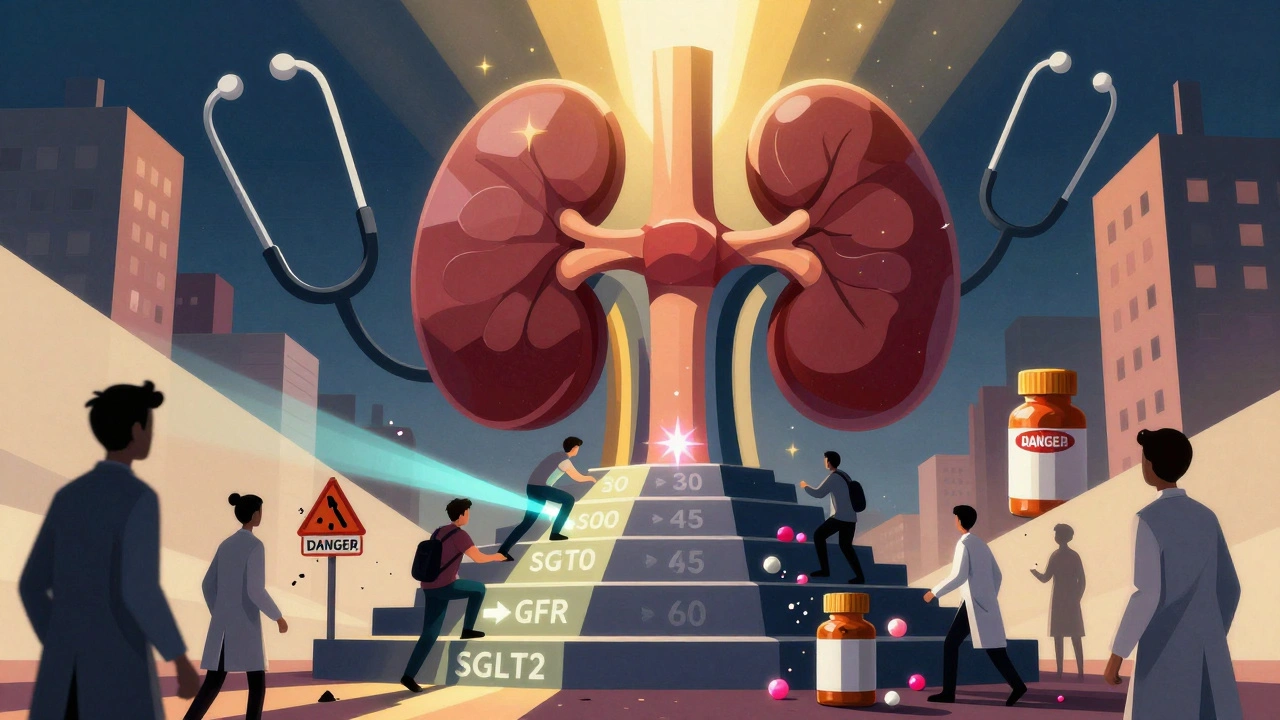
Real-World Gaps: Why So Many Patients Are Still Left Behind
Even with solid guidelines, access is uneven. At Baylor College of Medicine, 37% of patients with eGFR 20-29 weren’t getting SGLT2 inhibitors-mostly because doctors were scared. On Reddit’s r/nephrology, a nephrologist said they had to re-educate 12 primary care doctors in one month.
And cost matters. A 2023 JAMA study found SGLT2 inhibitor use in advanced CKD was over three times higher in people earning $150,000+ a year than those making under $40,000. These drugs aren’t cheap. But if your insurance won’t cover them, ask about patient assistance programs. Many manufacturers offer free or low-cost options.
The biggest mistake? Stopping metformin too early. Too many doctors pull the plug when eGFR hits 40, even though the guideline allows up to 1,000 mg daily at that level. Others wait until eGFR is below 30 to start an SGLT2 inhibitor-missing the window where they could’ve slowed kidney decline.
What’s Coming Next?
The science is still evolving. The ZEUS trial (NCT05225191), which finished enrolling patients in December 2023, is testing dapagliflozin in people with eGFR as low as 15. Results are expected in late 2025. Early data from the DAPA-CKD-Extension trial already suggest SGLT2 inhibitors may be safe even for people on dialysis.
KDIGO plans to update its guidelines again in early 2024, incorporating new data from the EMPA-KIDNEY and DELIVER trials. One thing is clear: the future of CKD and diabetes care isn’t about avoiding drugs-it’s about using them smarter, earlier, and with better monitoring.
Can I still take metformin if my eGFR is 35?
Yes. With an eGFR of 35 mL/min/1.73 m², you can safely take up to 1,000 mg of metformin per day. This is within the KDIGO 2022 guidelines. You don’t need to stop unless your eGFR falls below 30 or you have an acute illness like severe dehydration or infection.
Is it safe to start an SGLT2 inhibitor if my eGFR is 22?
Yes. As of the 2022 KDIGO guidelines, SGLT2 inhibitors can be started at eGFR ≥20 mL/min/1.73 m². The EMPA-KIDNEY trial showed clear benefits even at this level. You can continue the drug even if your eGFR drops further, as long as you’re not experiencing serious side effects like volume depletion or ketoacidosis.
What should I do if I get sick and my eGFR drops suddenly?
If you’re sick-especially with vomiting, diarrhea, fever, or dehydration-pause metformin immediately. For SGLT2 inhibitors, continue unless you’re severely dehydrated or showing signs of ketoacidosis (nausea, stomach pain, confusion). Check your eGFR once you recover. Restart metformin only when your eGFR is above 45 and stable.
Do SGLT2 inhibitors work the same in all types of kidney disease?
The proven benefits are strongest in diabetic kidney disease, which is the most common cause of CKD. They also help in non-diabetic CKD, especially if you have protein in your urine (albuminuria). But the data is less clear for rare kidney diseases like polycystic kidney disease or glomerulonephritis. Talk to your nephrologist about whether it’s right for your specific condition.
Why is my doctor still refusing to prescribe an SGLT2 inhibitor even though my eGFR is 28?
Many doctors still follow old guidelines from before 2022. They may think SGLT2 inhibitors are only for eGFR ≥30. You can ask them to review the KDIGO 2022 Clinical Practice Guideline or the ADA 2022 Standards of Care. The evidence is now overwhelming: these drugs reduce kidney failure and death, even at eGFR 20-29. Your kidney health depends on using them early.
If you have CKD and diabetes, you’re not stuck with outdated, risky treatments. The tools to protect your kidneys are here-and they’re more effective than ever. The key is knowing the current rules, asking the right questions, and making sure your care team is up to date. Don’t let fear of side effects keep you from the therapy that could keep you alive longer and healthier.



15 Comments