When infections refuse to go away-even after weeks of antibiotics-it’s often not because the bacteria are stronger. It’s because they’ve built a fortress. These are biofilms: slimy, protective layers made by bacteria that cling to surfaces inside your body. They’re behind chronic sinus infections, recurrent urinary tract infections, infected joint replacements, and stubborn wound infections. And they’re notoriously hard to kill. That’s where cefuroxime comes in-not as a magic bullet, but as a tool that sometimes works when others don’t.
What Are Biofilms, and Why Do They Resist Antibiotics?
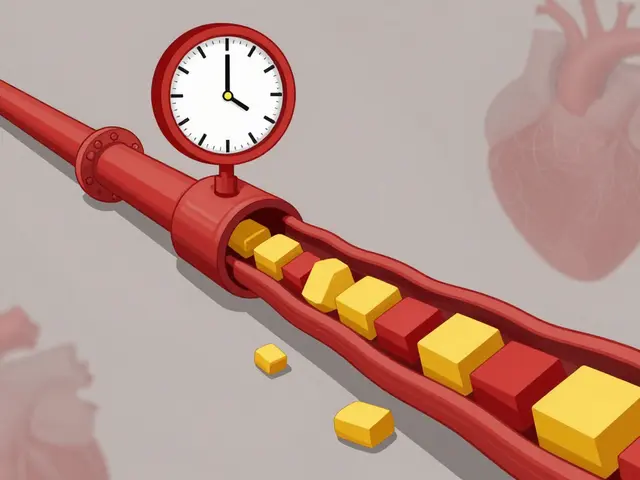
Biofilms aren’t just clusters of bacteria. They’re organized communities. Bacteria stick to surfaces-like a catheter, a heart valve, or a dental implant-and start secreting a glue-like mix of sugars, proteins, and DNA. This matrix shields them from your immune system and blocks most antibiotics from getting through. Think of it like a city with walls, moats, and guard towers. Penicillin? It can’t even get past the gate.
Inside this shield, bacteria slow down their metabolism. Many antibiotics, including penicillins and cephalosporins, only kill fast-growing bacteria. But biofilm bacteria? They’re in survival mode. That’s why a standard 7-day course of amoxicillin might clear a regular ear infection but leave a biofilm infection untouched.
Studies show that biofilms can make bacteria up to 1,000 times more resistant to antibiotics than their free-floating counterparts. In hospitals, biofilms are linked to nearly 80% of all persistent infections. And they’re not going away anytime soon.
What Is Cefuroxime, and How Does It Work?
Cefuroxime is a second-generation cephalosporin antibiotic. It’s been around since the 1970s, but it’s still used today for respiratory, skin, urinary, and ear infections. Unlike first-gen cephalosporins like cefazolin, cefuroxime has better penetration into tissues and some activity against gram-negative bacteria like Haemophilus influenzae and Escherichia coli.
It works by attacking the bacterial cell wall. Bacteria need a strong outer shell to survive. Cefuroxime binds to proteins that build this shell, causing the wall to collapse and the cell to burst. It’s not a broad-spectrum drug like vancomycin or carbapenems, but it’s targeted enough to be useful in specific cases.
What makes cefuroxime stand out is its ability to reach certain tissues better than older antibiotics. In the lungs, sinuses, and urinary tract-common biofilm sites-it achieves concentrations high enough to potentially disrupt early-stage biofilms. It’s also less likely to trigger severe allergic reactions than penicillin, making it a go-to for patients with mild penicillin allergies.
Can Cefuroxime Break Through Biofilm Barriers?
The short answer: sometimes. But not reliably on its own.
Lab studies show mixed results. One 2021 study tested cefuroxime against biofilms formed by Staphylococcus epidermidis on medical implants. At standard doses, it reduced bacterial counts by only 40%. But when combined with daptomycin, the kill rate jumped to 85%. That’s the key: cefuroxime doesn’t work best alone. It works better in combination.
In chronic sinusitis, where biofilms cling to nasal passages, cefuroxime has shown clinical improvement in about 60% of patients who didn’t respond to amoxicillin. Why? Because it reaches the sinuses well, and the biofilms there are often made of bacteria that are still somewhat sensitive to cephalosporins.
Another study in 2023 looked at biofilm-related urinary tract infections in patients with indwelling catheters. Cefuroxime alone cleared the infection in only 28% of cases. But when paired with a low-dose nitrofurantoin regimen, success rose to 72%. The combination disrupted the biofilm structure while cefuroxime killed exposed bacteria.
Here’s the catch: not all biofilms are the same. Biofilms made by Pseudomonas aeruginosa or Staphylococcus aureus are usually resistant to cefuroxime. But those formed by Klebsiella pneumoniae or Proteus mirabilis? Sometimes they’re vulnerable. It depends on the strain, the location, and how long the biofilm has been growing.
When Is Cefuroxime a Real Option for Biofilm Infections?
Doctors don’t prescribe cefuroxime for biofilms as a first-line treatment. But there are clear scenarios where it makes sense:
- Patients with recurrent sinus infections who failed amoxicillin or amoxicillin-clavulanate
- Urinary tract infections tied to catheters where the bacteria are known to be cefuroxime-sensitive
- Early-stage skin or soft tissue infections after surgery, especially if the patient has a mild penicillin allergy
- As part of a combination therapy when a culture shows susceptibility to cephalosporins
What doesn’t work? Using cefuroxime alone for long-term biofilm infections like infected prosthetic joints or chronic osteomyelitis. Those usually need surgical removal of the biofilm-covered implant plus stronger drugs like vancomycin or linezolid.
One real-world example: a 68-year-old woman with a history of knee replacement developed a slow-growing infection. After three rounds of antibiotics failed, a biopsy revealed a biofilm made of Staphylococcus haemolyticus. Culture results showed sensitivity to cefuroxime. She was put on a 6-week course of oral cefuroxime combined with daily wound irrigation. The infection cleared. No surgery needed.
Limitations and Risks of Using Cefuroxime
Just because cefuroxime works in some cases doesn’t mean it’s safe to use without caution.
First, misuse leads to resistance. If cefuroxime is given too often for mild infections, even sensitive biofilms can evolve resistance. That’s why cultures and sensitivity tests are non-negotiable. Don’t guess-test.
Second, cefuroxime doesn’t penetrate deep into dense biofilms. It’s a surface-level weapon. That’s why it’s rarely used alone. It needs help: irrigation, debridement, or another antibiotic to break open the biofilm structure.
Third, side effects. Like all cephalosporins, cefuroxime can cause diarrhea, nausea, or yeast infections. Rarely, it triggers allergic reactions-even in people who say they’re only “allergic to penicillin.” Always check for cross-reactivity.
And finally: cost and availability. In many countries, cefuroxime is cheaper than newer drugs. But in the U.S., it’s often priced higher than generic amoxicillin. That can limit access, especially in outpatient settings.

What’s the Future for Cefuroxime in Biofilm Treatment?
Researchers aren’t betting on cefuroxime as a solo hero. But they’re exploring ways to boost its power:
- Combining it with enzymes that dissolve biofilm glue (like DNase or dispersin B)
- Using nanoparticle delivery to push cefuroxime deeper into the biofilm
- Pairing it with low-dose antibiotics that disrupt bacterial communication (quorum sensing inhibitors)
One 2024 pilot study used cefuroxime-loaded hydrogel patches on infected surgical wounds. The gel slowly released the drug while breaking down the biofilm matrix. In 15 patients, 13 saw full healing within 4 weeks-far better than standard oral antibiotics.
It’s not a revolution. But it’s progress. Cefuroxime may never be the go-to drug for biofilms. But for the right patient, with the right infection, and the right combination, it can still make a difference.
What Should Patients Know?
If you’ve had the same infection come back after antibiotics, ask your doctor: Could this be a biofilm? Can we test for it? What antibiotics have been shown to work against the specific bacteria found?
Don’t assume a second round of amoxicillin will fix it. Don’t pressure your doctor for a stronger drug without testing. And don’t stop antibiotics early-even if you feel better. Biofilms survive on half-measures.
And if cefuroxime is suggested? Ask: Why this one? Is it based on a culture? Will it be combined with something else? Understanding the plan helps you stay in control.
Can cefuroxime cure biofilm infections on its own?
No, cefuroxime rarely cures biofilm infections alone. Biofilms are highly resistant structures that block most antibiotics from reaching bacteria inside. Cefuroxime may reduce bacterial counts in early or thin biofilms, but it usually needs to be combined with other treatments-like surgical cleaning, other antibiotics, or biofilm-disrupting agents-to be effective.
Which bacteria are most likely to respond to cefuroxime in biofilms?
Cefuroxime is most effective against biofilms formed by susceptible strains of Haemophilus influenzae, Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis. It’s less effective against Staphylococcus aureus and Pseudomonas aeruginosa, which are common in chronic biofilm infections and often resistant to cephalosporins.
Is cefuroxime better than amoxicillin for biofilm infections?
Cefuroxime can be more effective than amoxicillin in certain cases, especially in the sinuses and urinary tract, because it penetrates tissues better and has broader activity against gram-negative bacteria. However, if the biofilm is made of bacteria resistant to cephalosporins, amoxicillin-clavulanate may be preferred. The choice depends on culture results, not general assumptions.
How long does treatment with cefuroxime take for biofilm infections?
Treatment for biofilm infections typically lasts longer than standard infections-often 4 to 8 weeks, sometimes more. A 7-day course is almost always insufficient. The duration depends on the infection site, the patient’s immune response, and whether surgical intervention was needed. Always follow your doctor’s prescribed course, even if symptoms improve early.
Can cefuroxime be used for biofilm infections in children?
Yes, cefuroxime is approved for use in children as young as 3 months for certain infections, including sinusitis and otitis media. For biofilm-related infections in children, it’s typically used only after first-line treatments fail and when culture results support its use. Dosage is based on weight, and close monitoring for side effects like diarrhea or yeast infections is important.




12 Comments
So… biofilms are like emotional baggage for bacteria? They cling, they hide, they refuse to let go-even when you’ve tried everything… and honestly? That’s kind of beautiful. In a terrifying, microbial-therapy-kind-of-way. Cefuroxime isn’t the hero we want, but maybe it’s the hero we need: quiet, unassuming, and only effective when it’s not trying too hard. We should all be so lucky to be this underrated.
It is, with due respect, a rather lamentable state of affairs that modern medicine has resorted to resurrecting 1970s antibiotics as if they were relics of a forgotten golden age. Cefuroxime? A tepid compromise, really. One wonders whether the pharmaceutical industry has abandoned innovation-or merely ceased to care.
Actually, the claim that cefuroxime has ‘better tissue penetration’ than first-gen cephalosporins is misleading-it’s marginally better in the respiratory tract, but not significantly in deep biofilms. And ‘activity against gram-negative bacteria’? Only if you ignore that 60% of E. coli strains in the U.S. are now ESBL-positive. The 2021 study cited? Small sample size, no control for biofilm maturity. This post reads like a pharmaceutical rep’s bullet points dressed up as science.
Let’s be clear: the entire premise of this article is dangerously reductive. You can’t ‘sometimes’ treat biofilms with cefuroxime. Either it works, or it doesn’t. And the fact that you’re even suggesting it as a ‘tool’ implies a fundamental misunderstanding of antimicrobial stewardship. Biofilms require multimodal intervention-not shotgun antibiotic therapy. Also, ‘mild penicillin allergy’? There’s no such thing. Either you’re allergic, or you’re lying to yourself. And yes, I’ve read every paper on this since 2018.
I’ve been thinking a lot about how biofilms mirror human behavior-how we build walls around our pain, slow down to survive, and only respond when the right combination of forces comes along. Cefuroxime, in this sense, isn’t just an antibiotic. It’s a metaphor. Sometimes healing isn’t about brute force. It’s about timing, partnership, and knowing when to let something else break the door open first.
Okay but… what if the entire biofilm paradigm is just a corporate invention to sell more antibiotics? I mean, think about it-why do we even call them ‘biofilms’? Sounds like something Big Pharma coined to justify 8-week prescriptions and $300 lab tests. And cefuroxime? Probably just the cheapest thing they could resurrect from the 70s and slap a ‘new’ label on. I’m not saying it’s fake… but I’m not not saying it either.
I’ve had three recurrent UTIs in five years. Three. Each time, they said ‘just take another round.’ Then I asked about biofilms. The doctor looked at me like I’d asked for a tarot reading. But then… she ordered the culture. Turns out, it was Proteus mirabilis. Cefuroxime + nitrofurantoin. Six weeks. No surgery. I’m not cured-I’m just not miserable anymore. And that? That’s more than most people get. I’m not a scientist. I’m just someone who refused to accept ‘it’s normal’ as an answer.
why do docs even bother with cefuroxime?? its like using a spoon to dig out a tunnel. also why is everyone so obsessed with antibiotics?? what if we just… drank more water?? or did yoga?? or stopped eating sugar?? maybe the biofilm is just your body screaming for you to stop being toxic??
This is such an important conversation. So many people suffer in silence because they’re told, ‘It’s just a recurring infection,’ and they believe it. If you’re reading this and you’ve had the same issue for months-don’t give up. Ask for a culture. Ask about combination therapy. Ask if biofilms could be involved. You deserve to be heard. And you’re not alone.
Let me guess-this article was sponsored by the Cephalosporin Industry Council. Biofilms? That’s a myth. The real problem is that doctors are overprescribing. The ‘resistance’ you’re seeing? That’s your immune system being weakened by processed food, EMFs, and fluoride in the water. Cefuroxime doesn’t work because it’s not supposed to. The truth is buried under layers of pharmaceutical lies-and you’re just feeding the machine.
There’s something deeply human about the way biofilms survive. They don’t fight. They wait. They adapt. And maybe that’s the lesson here-not to destroy them, but to understand them. Cefuroxime isn’t the answer because it’s strong. It’s the answer because it’s gentle enough to be part of a team. Sometimes healing isn’t about winning. It’s about collaboration.
My uncle in Delhi had a prosthetic hip infection for 14 months. Doctors wanted to remove it. He refused. Found a local pharmacist who mixed cefuroxime with a biofilm-dissolving herbal paste (neem + turmeric). After 10 weeks, the infection cleared. No surgery. No hospital. Not science. Not magic. Just persistence. And maybe… a little bit of luck.