Warfarin Genetics: How Your DNA Affects Blood Thinners
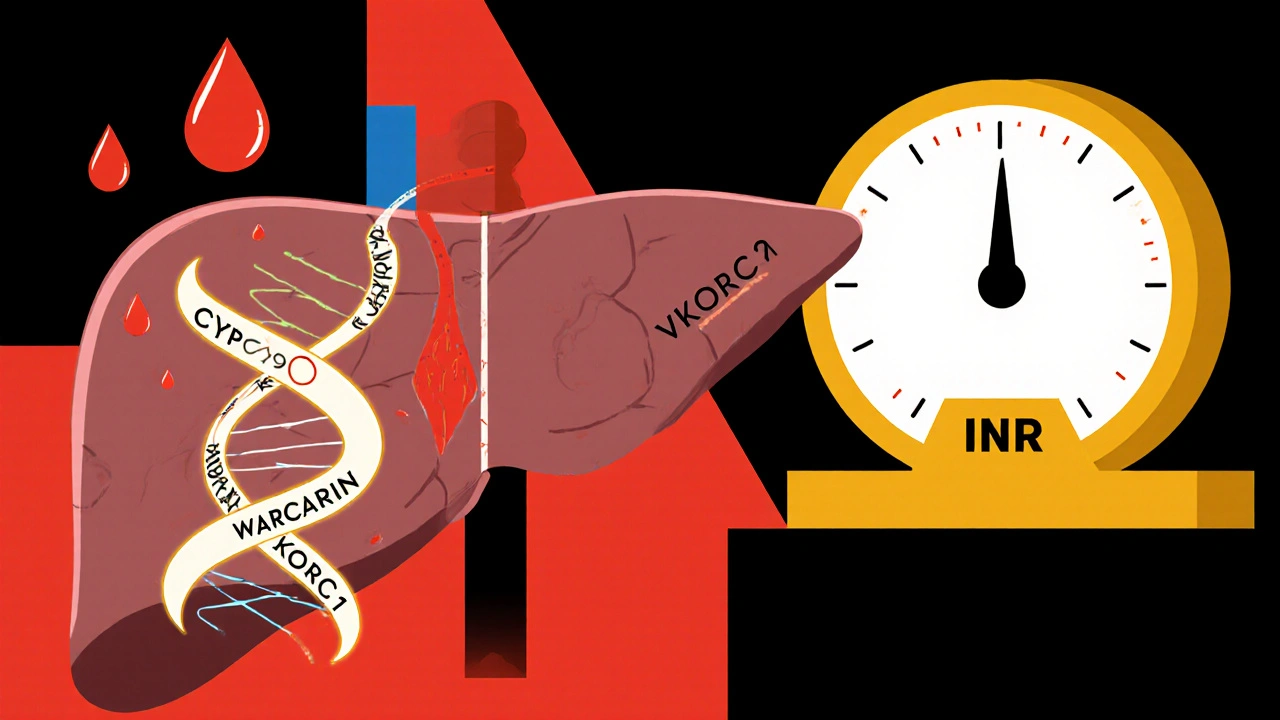
When you take warfarin, a blood thinner used to prevent dangerous clots. Also known as Coumadin, it's one of the most commonly prescribed anticoagulants worldwide, but getting the dose right isn't guesswork—it's personal. Your body doesn’t process warfarin the same way as someone else’s. That’s because your genes, especially CYP2C9, an enzyme that breaks down warfarin in the liver and VKORC1, a gene that controls how sensitive your blood is to the drug, determine how much you need. Some people break it down fast and need higher doses. Others break it down slow and risk bleeding with even small amounts. This isn’t rare—it’s normal. Studies show up to 30% of warfarin dose differences come from these two genes alone.
Doctors don’t just eyeball your dose anymore. If you’re starting warfarin, your doctor might order a simple genetic test—a cheek swab or blood sample—that checks your CYP2C9 and VKORC1 variants. That test doesn’t replace INR monitoring, but it gives a smarter starting point. For example, if you have two slow-metabolizer versions of CYP2C9, your initial dose might be cut in half compared to someone without those variants. Same with VKORC1: if your version makes you super sensitive to warfarin, even 2 mg a day could be too much. This isn’t theory—it’s in clinical guidelines from the FDA and the Clinical Pharmacogenetics Implementation Consortium. Skip the trial-and-error. Genetic testing cuts down the time you spend in the danger zone before finding your safe dose.
Why does this matter to you? Because too much warfarin can cause bleeding in your brain, gut, or joints. Too little and you could get a stroke or a clot in your lung. Neither is acceptable. And while warfarin has newer alternatives like apixaban or rivaroxaban, it’s still widely used because it’s cheap, well-understood, and reversible if needed. But its narrow window makes precision critical. If you’ve been on warfarin for a while and your dose keeps changing, or if you’ve had a bleed or clot despite following instructions, your genes might be the missing piece. You’re not doing anything wrong. Your body is just wired differently.
What you’ll find in the posts below are real-world stories and science-backed guides on how warfarin interacts with other drugs, how diet affects it, why some people respond unpredictably, and how genetic testing fits into daily care. You’ll see how CYP2C9 and VKORC1 show up in drug interactions, how lifestyle changes can make dosing harder or easier, and what to ask your doctor if you’re unsure why your dose keeps shifting. This isn’t just about genetics—it’s about survival, control, and knowing your body better than ever before.
Warfarin Genetics: How CYP2C9 and VKORC1 Variants Affect Bleeding Risk and Dosing
Warfarin dosing varies wildly based on genetics. CYP2C9 and VKORC1 variants can make you dangerously sensitive to the drug. Testing before starting can cut bleeding risk by 32% and save lives.
read more