Warfarin Dosing Calculator
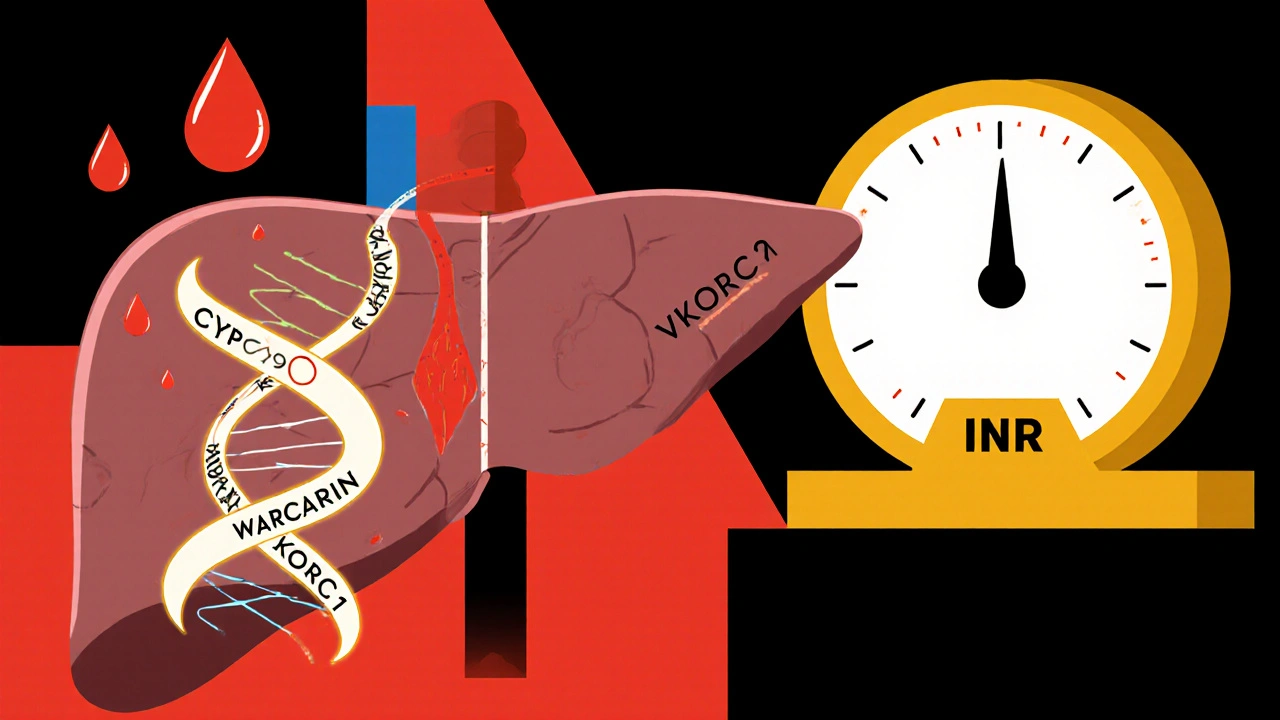
Calculate your personalized warfarin starting dose based on your genetic profile. The article explains how CYP2C9 and VKORC1 variants affect bleeding risk and dosing requirements.
Recommended Starting Dose
Please select your genetic variants above.
Every year, millions of people start taking warfarin to prevent dangerous blood clots. But for many, the drug is a balancing act-too little and clots form; too much and they bleed. And the difference between life and a hospital visit often comes down to genes you were born with, not your diet, age, or weight. Two genes, CYP2C9 and VKORC1, control how your body handles warfarin. If you carry certain versions of these genes, your risk of bleeding skyrockets-even if you’re taking what doctors call a "standard" dose.
Why Warfarin Is So Hard to Get Right
Warfarin doesn’t work the same way for everyone. It blocks a protein called VKORC1, which your liver needs to activate clotting factors. But your body also breaks down warfarin using an enzyme made by the CYP2C9 gene. If either of these processes is slower than normal, warfarin builds up in your blood. That’s when your INR (a measure of blood clotting time) spikes dangerously high.Most doctors start patients at 5 mg per day. That’s fine for some. But for others, it’s a recipe for disaster. A 2013 study in The Lancet showed that patients with certain gene variants had a 32% lower risk of major bleeding when their dose was adjusted based on genetics. That’s not a small number. It means for every 100 people tested, about 3 avoid a life-threatening bleed.
The VKORC1 Gene: Your Body’s Warfarin Sensitivity Switch
The VKORC1 gene tells your body how much of the warfarin target protein to make. The most common variant, called -1639G>A (rs9923231), changes how much VKORC1 your liver produces. If you have two copies of the A version (AA genotype), your body makes about 40% less of the protein. That means warfarin hits harder. You don’t need as much to get the same effect.People with the AA genotype often need only 5-7 mg per week. Someone with the GG version? They might need 28-42 mg per week. That’s a six-fold difference. And if you’re AA but start at 5 mg a day? Your INR could hit 6.2 in two weeks-like one Reddit user reported after his doctor ignored his genetic results. He ended up in the ER. That’s not rare. A 2020 review found patients with AA and CYP2C9*3 variants had an 83% higher chance of dangerous INR spikes in the first week.
The CYP2C9 Gene: Your Body’s Warfarin Breakdown System
CYP2C9 is the enzyme that breaks down the more powerful half of warfarin-the S-enantiomer. It’s five times stronger than the R version. Two common variants, *2 and *3, slow this breakdown way down. The *3 variant is especially dangerous. Carriers clear S-warfarin 80% slower than normal. That means even a small dose lingers in your blood for days.People with CYP2C9*3/*3 (two copies of the bad variant) may need as little as 0.5 mg per day. But without testing, they’re often started at 5 mg. The results? A 2018 study in the Journal of Thrombosis and Haemostasis found 68% of CYP2C9 variant carriers had at least one INR over 4 in the first three months. Only 42% of non-carriers did. Bleeding events requiring medical care? 18.7% vs. 9.3%.
When Both Genes Work Against You
The worst-case scenario isn’t just one bad gene-it’s both. Someone with the VKORC1 AA genotype and CYP2C9*3/*3 is in the danger zone. Their body makes less of the target protein and breaks down the drug extremely slowly. This combination can reduce the effective warfarin dose by 70-80% compared to someone with normal genes.A 2025 meta-analysis in the European Heart Journal confirmed: patients with this double-hit genotype had a 27% lower risk of major bleeding when dosed based on genetics. That’s why guidelines from the Clinical Pharmacogenetics Implementation Consortium (CPIC) now recommend testing before starting warfarin for long-term use. Yet in the U.S., only 5-15% of patients get tested. Why? Cost, lack of awareness, and slow adoption by clinics.
What Testing Actually Looks Like
Getting tested isn’t complicated. A simple cheek swab or blood draw sends your DNA to a lab. Results come back in 3-5 days. The test checks for two things: the VKORC1 -1639G>A variant and the CYP2C9*2 and *3 variants. The cost? Around $250-$500 in the U.S., but Medicare covers it under CPT codes 81225 and 81227. Many private insurers do too-if you push.Doctors use a CPIC algorithm to turn those results into a dose. For example:
- AA + *1/*1: Start at 3-4 mg/day
- AG + *1/*3: Start at 2-3 mg/day
- AA + *3/*3: Start at 0.5-1 mg/day
At Vanderbilt University Medical Center, after switching to genotype-guided dosing, patients reached a stable INR 1.8 days faster. That’s almost two full weeks of risky INR swings avoided.
Why So Many Doctors Still Ignore Genetics
Despite the evidence, many clinicians don’t test. A 2023 survey found only 38% of primary care doctors knew CYP2C9*3 reduces warfarin clearance. Others say the benefit isn’t clear enough. The American College of Chest Physicians even recommends against routine testing, citing "inconsistent evidence." But that’s based on older studies. Newer trials like REAL-Gene (2023) showed an 8.2% reduction in time outside therapeutic range-enough to prevent serious bleeds.There’s also a perception that direct oral anticoagulants (DOACs) like apixaban and rivaroxaban have made warfarin obsolete. And yes, DOACs are easier-they don’t need frequent blood tests. But warfarin is still the only option for people with mechanical heart valves or severe kidney failure. And it’s the only one you can reverse quickly with vitamin K or fresh plasma if you bleed.

Real Stories, Real Consequences
Reddit’s r/anticoag community is full of stories like these:- u/WarfarinWarrior (March 2023): "After genetic testing revealed CYP2C9*3, my dose dropped from 5mg to 2.5mg. My INR finally stabilized after six months of rollercoaster readings. I wish I’d known sooner."
- u/ClottingConfused (January 2024): "Got tested for VKORC1, found out I’m AA. Doctor started me at 5mg anyway. Two weeks later, INR was 6.2. I was in the ER with nosebleeds and bruising everywhere."
A 2022 survey of 1,247 warfarin users found 74% of those who got tested were happier with their treatment. Their satisfaction score? 7.8 out of 10. For those without testing? 6.2. The biggest complaint? Insurance wouldn’t pay.
What’s Changing Now
The tide is turning. The FDA added pharmacogenetic info to warfarin labels in 2010. In 2024, the GeneSight Psychotropic test expanded to include warfarin genes. And in 2025, the University of Florida launched the Warfarin Genotype Implementation Network (WaGIN), aiming to test 50,000 patients across 200 hospitals.Costs are falling. By 2027, testing may drop below $100. And by 2030, experts predict 60% of new warfarin users will get tested. The data is too strong to ignore. For patients on long-term therapy-especially those over 65, with a history of falls, or on multiple medications-the risk of bleeding is real. Genetics isn’t just science. It’s safety.
What You Should Do
If you’re on warfarin-or about to start-ask your doctor this:- Have you tested my CYP2C9 and VKORC1 genes?
- If not, can we order it? Medicare and many insurers cover it.
- What’s my target dose based on my genetics?
Don’t wait for a bleed to happen. Genetic testing takes days. The consequences of waiting can last a lifetime.



14 Comments