
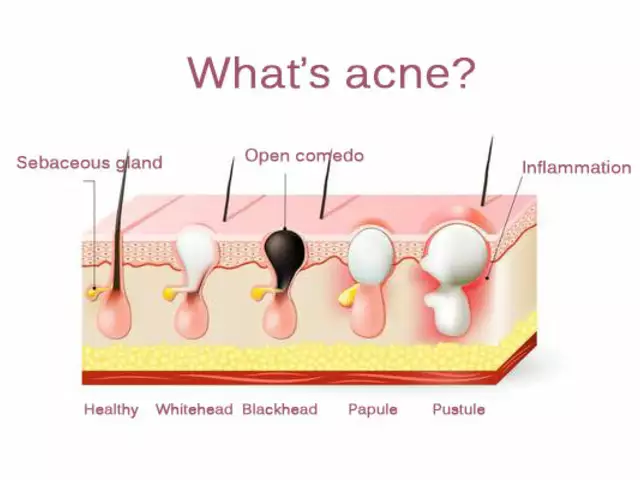
When a patient walks into a hospital or nursing home with a prescription for a brand-name drug like Xarelto, they might leave with a different pill in their hand-apixaban, for example. It’s not a mistake. It’s institutional formularies at work. These aren’t just lists of approved drugs. They’re legally enforced systems that let hospitals and clinics swap one medication for another, as long as it’s expected to do the same job. And while this sounds like a smart way to save money, it’s also a source of confusion, risk, and debate across the healthcare system.
What Exactly Is an Institutional Formulary?
An institutional formulary is a living list of drugs that a hospital, clinic, or nursing home has approved for use. But it’s more than a catalog. It’s a rulebook. It tells pharmacists when they can swap a prescribed drug for another-usually cheaper, often generic-that’s considered therapeutically equivalent. This isn’t random. It’s based on clinical evidence, cost, and safety data reviewed by a team of doctors, pharmacists, and nurses.
Florida’s Statute 400.143 (2025) gives one of the clearest definitions: therapeutic substitution means replacing a prescribed drug with a different one that’s expected to have the same clinical effect. That’s the core. It’s not about changing the treatment goal. It’s about changing the tool used to reach it.
Unlike insurance formularies, which decide what drugs a patient’s plan will pay for, institutional formularies control what drugs can be given inside a facility. A hospital might have a formulary that allows substitution only after a committee review. A nursing home might be required to swap a patient’s medication every time they’re admitted, based on its own list. These rules vary by state, by facility, and by the type of care being delivered.
Who Decides What Goes on the List?
It’s not a single doctor or a pharmacy director making these calls alone. Florida law requires a formal committee to oversee every institutional formulary. This committee must include:
- The facility’s medical director
- The director of nursing services
- A consultant pharmacist licensed and certified under state law
That’s not just a box-checking requirement. It’s a design feature. Doctors know what conditions need treating. Nurses see how patients respond to meds day-to-day. Pharmacists understand drug interactions, bioavailability, and cost trade-offs. Together, they build policies that balance safety, effectiveness, and affordability.
The committee also writes the rules: how drugs are chosen, how substitutions are documented, how prescribers are notified when a change happens, and how outcomes are tracked. These policies must be written down, updated at least once a year, and made available to regulators on demand.
And they’re not static. Formularies get reviewed quarterly. That’s when the team looks back: Did switching from lisinopril to enalapril lead to more dizziness in elderly patients? Did switching to a generic statin reduce hospital readmissions? Those answers shape the next version of the list.
How Do Substitutions Actually Work?
Most institutional formularies use a tiered system. Think of it like a pricing ladder:
- Tier 1 (Preferred): Generic drugs with proven effectiveness and lowest cost. These are the first choice.
- Tier 2 (Non-preferred): Brand-name drugs or newer generics that cost more. May require prior authorization.
- Tier 3 (Specialty): High-cost drugs for complex conditions. Often require special approval and documentation.
When a doctor writes a prescription for a Tier 2 or Tier 3 drug, the pharmacy system flags it. The pharmacist can then propose a Tier 1 alternative. If the prescriber agrees, the substitution happens. If not, the pharmacist can still dispense the original drug-but only after the doctor fills out paperwork explaining why.
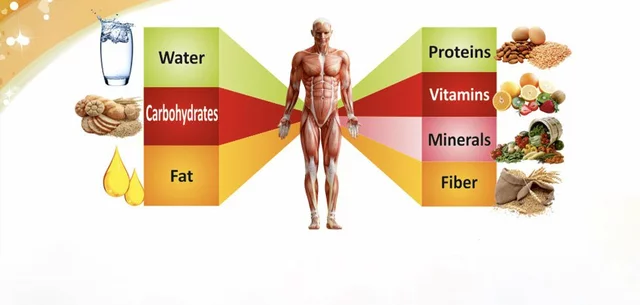
This system cuts costs. A 2023 study in the American Journal of Health-System Pharmacy found that hospitals using structured formularies reduced adverse drug events by 15-30%. Why? Because they eliminate outdated, risky, or overpriced drugs from circulation. A drug that causes more falls in older adults? Removed. A cheaper version with the same effect? Added.
But here’s the catch: substitutions aren’t always seamless. A patient might get switched from Xarelto to apixaban in a nursing home. Then, when they’re admitted to the hospital, the hospital’s formulary doesn’t recognize apixaban as a preferred substitute for Xarelto-and switches them back. The patient gets confused. The family doesn’t know why the meds changed. The doctor has to explain it all over again.

Where Do Institutional Formularies Work Best-and Where Do They Fall Short?
In long-term care, institutional formularies shine. Nursing homes have stable patient populations. Medications don’t change daily. Consistency matters. Florida’s law was written with nursing homes in mind. And it works: 94% of nursing homes have formal formularies, compared to 78% of acute care hospitals.
One Tampa nursing home director told the American Health Care Association in June 2024 that their quarterly reviews caught seven dangerous drug interactions in the first year-problems they’d never have noticed without structured monitoring.
But in emergency rooms or intensive care units? Things get messy. A patient arrives with a heart attack. They’re on a blood thinner that’s not on the hospital’s formulary. Waiting for committee approval isn’t an option. In these cases, formularies become bureaucratic roadblocks. A 2023 AMA survey found that 78% of physicians felt hindered by the paperwork needed to get non-formulary drugs approved for complex cases.
Patients, too, often don’t know they’ve been switched. AARP’s Policy Institute noted that many long-term care residents aren’t informed about substitutions. That’s a consent issue. If a patient’s doctor prescribed a specific drug for a reason-maybe because it’s easier to swallow, or it doesn’t interact with their other meds-and they’re swapped without explanation, that’s not just a policy problem. It’s an ethical one.
Implementation Challenges: Tech, Training, and Time
Setting up a formulary isn’t just about writing policies. It’s about making them work in real life.
Most facilities struggle with their electronic health records (EHR). A 2024 Florida Agency for Health Care Administration survey found that 68% of facilities had technical problems integrating formulary rules into their EHR systems. Without alerts, pharmacists miss substitution opportunities. Or worse-they make the wrong swap because the system doesn’t flag a contraindication.
Training is another hurdle. Nursing staff, who administer most medications, need the most education. On average, it takes 4-8 weeks for staff to fully understand the new workflows. And then there’s the time cost. Facilities report spending 20-30 hours per quarter just on formulary maintenance: reviewing data, updating documents, holding committee meetings.
Tools like the Academy of Managed Care Pharmacy’s Formulary Management Toolkit help. Eighty-five percent of hospital pharmacy directors say it’s essential. But even with the best tools, success depends on leadership. If the medical director doesn’t prioritize it, the formulary becomes a dusty document no one follows.
The Bigger Picture: Costs, Regulation, and the Future
Formularies are a $600 billion industry’s cost-control lever. In the U.S., 89% of all prescriptions are managed by some kind of formulary. Institutional ones cover about 27% of prescriptions in long-term care settings.
Thirty-two states now have laws similar to Florida’s. And the federal government is catching up. In March 2024, CMS announced that starting in Q3 2025, nursing home formulary compliance will be part of their public quality ratings-just like infection rates and fall prevention.
The future? AI-driven systems. By 2026, Gartner predicts 80% of healthcare systems will use algorithms that adjust formularies in real time based on patient outcomes. Imagine a system that notices patients on Drug A have more kidney issues than those on Drug B-and automatically updates the formulary without human input.
Some hospitals are already testing pharmacogenomics-using a patient’s genetic data to predict which drugs will work best. Deloitte found that 72% of healthcare executives plan to use this data in formulary decisions within five years.
But with innovation comes risk. If formularies become too automated, will they overlook rare but critical patient needs? Will cost-cutting override clinical judgment? The balance is fragile.
Final Thoughts: Safety, Savings, and the Human Element
Institutional formularies aren’t perfect. They can confuse patients, slow down care, and create administrative nightmares. But they also save lives. They stop dangerous drugs from being used. They cut waste. They bring consistency to care.
The real question isn’t whether formularies should exist. It’s how we make them better. That means:
- Training staff to explain substitutions to patients
- Building smarter EHR alerts that prevent errors
- Allowing exceptions for complex cases without drowning in paperwork
- Keeping patients in the loop
At the end of the day, a formulary is only as good as the people who use it. A well-run system doesn’t just control costs-it protects people. And that’s worth getting right.
What is therapeutic substitution in a hospital formulary?
Therapeutic substitution is when a hospital or clinic replaces a prescribed drug with a different one that’s expected to have the same clinical effect. For example, swapping Xarelto for apixaban. It’s not a random change-it’s based on evidence, cost, and safety data reviewed by a committee of doctors, pharmacists, and nurses.
Are institutional formularies the same as insurance formularies?
No. Insurance formularies determine what drugs your health plan will pay for and how much you pay out-of-pocket. Institutional formularies control what drugs can be given inside a hospital, clinic, or nursing home-and when substitutions are allowed. One is about payment; the other is about clinical practice.
Why do hospitals switch medications even when the doctor prescribed a specific drug?
Hospitals use formularies to reduce costs and improve safety by favoring drugs with proven effectiveness and lower prices-often generics. If a prescribed drug isn’t on the preferred list, the pharmacy may suggest a substitute. The doctor can still override it, but they usually need to explain why in writing.
Can patients refuse a therapeutic substitution?
Yes. Patients have the right to know what drug they’re being given and to refuse a substitution. However, if they choose the non-formulary drug, they may pay more out-of-pocket. In some cases, especially in long-term care, the facility may still require documentation from the prescribing doctor.
How often are institutional formularies updated?
By law in states like Florida, formularies must be reviewed quarterly for clinical outcomes and updated at least once a year. Many hospitals now review them monthly or bi-monthly, especially as new drugs and real-time data become available. The goal is to keep the list current with the latest evidence.
Do all hospitals have institutional formularies?
Most do. About 94% of nursing homes and 78% of acute care hospitals in the U.S. have formal formularies. But their strength varies. Some are tightly managed with strict rules and active monitoring. Others are outdated or ignored. The best ones involve real collaboration between clinical staff and pharmacy teams.


15 Comments
So, let me get this straight: a pharmacist can swap my grandma’s Xarelto for apixaban just because it’s cheaper? And no one even tells her? I’ve seen her forget her own name on a good day-how’s she supposed to know her meds changed? This isn’t efficiency, it’s negligence. I’m not mad, I’m just… disappointed. And honestly? Scared.
Of course it’s a corporate ploy. Big Pharma doesn’t want you to know this-formularies are just the FDA’s backdoor to rationing care. They’ve been pushing generics since the 90s, and now they’ve got hospitals doing their dirty work. You think apixaban is ‘therapeutically equivalent’? Ha. Ever heard of bioavailability variance? Or the fact that 17% of elderly patients on apixaban develop microbleeds that Xarelto doesn’t? The committee? They’re all on pharma payrolls. Look at the funding sources. It’s all connected. #FormularyConspiracy
Interesting read! In India, we call this 'formulary rationalization'-and honestly, it’s been a game-changer in rural clinics. We used to give patients 3 different BP meds because that’s what the rep left behind. Now? We have a strict 3-tier list. Cost dropped 60%. Mortality? Lower. But yes-communication gap is real. Patients think 'generic = weak'. Need more training, not just rules. Also, EHR integration? Still a nightmare here too. 😅
As someone who’s worked in nursing homes for 18 years, I’ve seen this go both ways. The right formulary? Saves lives. The wrong one? Creates chaos. We had a patient who was on a brand-name anticoagulant because he had a rare allergy to the fillers in generics. They swapped him anyway. He had a bleed. We had to call the doctor at 3 a.m. to fix it. The system isn’t broken-it’s under-resourced. We need more pharmacists on staff, not just policies on paper.
OMG I knew it!! They’re all just doing this to make the insurance companies happy!! It’s not about safety-it’s about profit margins!! They don’t care if you get confused, dizzy, or start hallucinating from the new med!! I had my mom switched from her 10-year-old med to some ‘equivalent’ junk and she started talking to the wall!! They’re experimenting on us!! #BigPharmaLies #FormularyTerror
man i never thought about this before but yeah my uncle got switched from one blood thinner to another and he got real dizzy for like a week. i asked the nurse why and she said ‘it’s just what the system says’. didn’t even know he had a history of falls. kinda scary how little they tell you. hope they fix it. just want people to be safe.
Bro this is so true!! In India we call it 'generic swap' and it saves so much money!! But yeah, patients get confused!! 😔 We started putting simple flyers in Hindi and Telugu next to the med cart. Now even grandma knows why her pill looks different!! 🙌 Also, EHR alerts? We built a simple SMS alert system for families!! Works like charm!! #HealthcareForAll
They’re not just swapping meds-they’re swapping your autonomy. You think your doctor chose Xarelto for a reason? Nah. They’re pressured by the hospital’s formulary committee. And who’s on that committee? People who got paid by the generic drug manufacturer. It’s all a front. They’re slowly removing every choice you have. This isn’t healthcare. It’s corporate control. And they’re watching you right now. 👁️
Great breakdown! Formularies are tools-not villains. The problem isn’t substitution-it’s poor execution. Train nurses. Fix EHR alerts. Let docs override without 10 forms. And tell patients. Simple. Done right, this saves lives. Done wrong? It’s a nightmare. Let’s fix the system, not blame the concept.
Been a pharmacy tech for 15 years. The tier system works-if you have time. In a busy ER? You’re lucky if you get 2 minutes to check a med. We’ve had cases where we swapped a med, then the patient got readmitted because the new one didn’t work with their kidney meds. We flagged it, but the EHR didn’t sync. It’s not the policy-it’s the tech. And the staffing. We’re understaffed and overworked. No one’s to blame. The system just sucks.
Oh wow, so now we’re pretending this is ‘evidence-based’? Let me guess-the ‘evidence’ was funded by the same company that makes the generic? Classic. And the ‘committee’? All friends of the hospital administrator. I’ve seen this play out in three different states. It’s not about safety. It’s about hitting budget targets. If your grandma dies because they swapped her med for a cheaper one? Well, that’s just ‘statistical variance’, right? 😏
Let’s be honest: institutional formularies are the logical endpoint of neoliberal healthcare. They reduce human beings to algorithmic data points-blood pressure, cost per pill, readmission rate. Where’s the dignity? Where’s the patient narrative? The committee doesn’t care that your drug makes your mouth taste like copper-that’s ‘not clinically significant’. You’re not a person. You’re a cost center. And this? This is the future. Welcome to the machine.
How quaint. A ‘committee’ of three people decides what drugs you get? In a world where AI predicts cancer from a single MRI, we’re still relying on a group of hospital bureaucrats with PowerPoint decks? The real innovation isn’t in formularies-it’s in the fact that we haven’t automated this entire process yet. The fact that this is still done by humans? That’s the real failure.
Yeah, I just talked to my aunt’s nurse. They’re finally adding a patient notification form. But it’s only printed in English. My aunt speaks Spanish. They’re not even trying. This isn’t about cost-it’s about who gets heard.