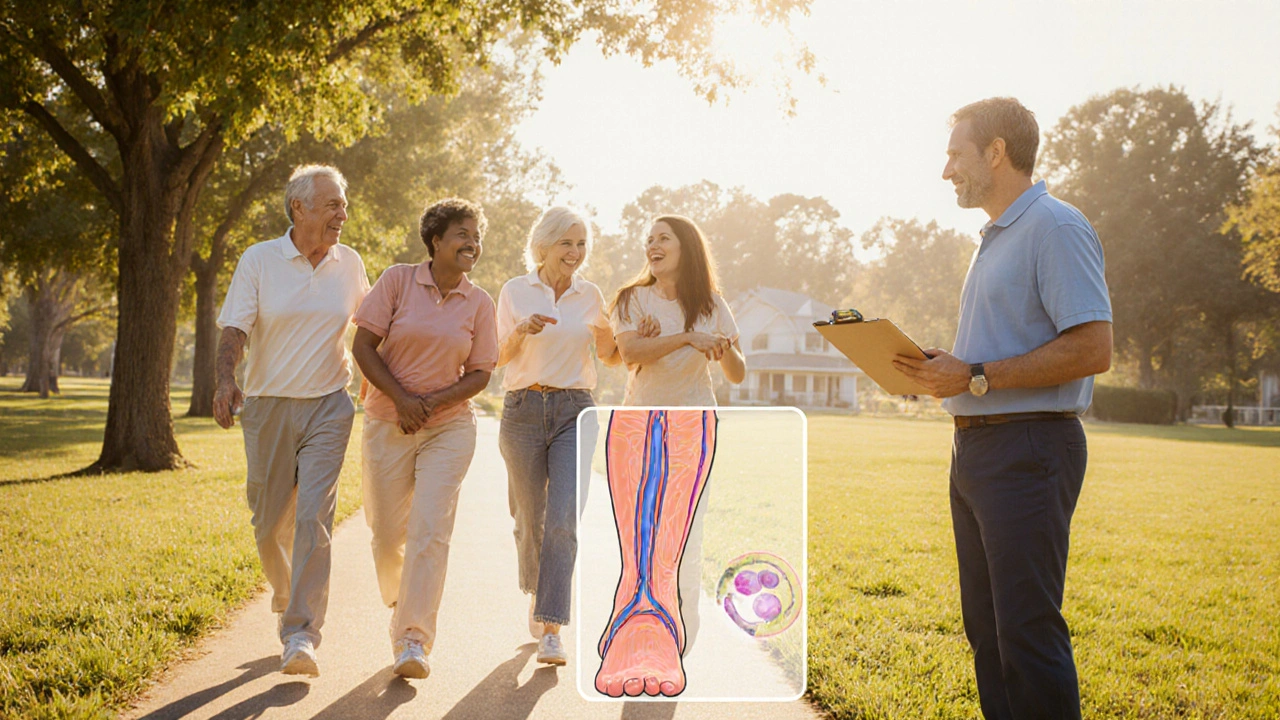
When it comes to blood clot myths are surprisingly common. A blood clot is a semi‑solid mass of platelets and fibrin that forms in a vessel and can block blood flow. The most talked‑about forms are deep vein thrombosis (DVT), which forms in the deep veins of the legs, and pulmonary embolism (PE), where a clot breaks off and travels to the lungs. Understanding the risk factors-like prolonged sitting, surgery, or inherited clotting disorders-helps you spot the real danger. Symptoms such as swelling, pain, or sudden shortness of breath trigger the need for prompt diagnosis, typically via ultrasound or CT scan. Treatment often involves an anticoagulant (blood‑thinner) and, in some cases, compression stockings. Below we separate fact from fiction so you can make sense of the hype.
Quick Guide
- Most clots form in the legs (DVT) and travel to the lungs (PE) only in serious cases.
- Clots are not caused by "cold weather" or "eating too much fat".
- Anticoagulants thin blood but do not dissolve existing clots instantly.
- Compression stockings help prevent DVT after surgery, but they won’t treat an existing clot.
- If you notice swelling, pain, or sudden breathlessness, seek medical help right away.
Myth #1: Cold Weather Makes You Clot
The idea that chilly temperatures cause blood to thicken and clot is a holdover from old folklore. In reality, the body regulates blood viscosity tightly, and ambient temperature has negligible impact on coagulation. What does increase risk in winter is reduced activity-people tend to sit longer on commutes or in front of heaters, which can lead to stasis, a key element in clot formation. So the myth stems from a correlation, not a direct cause.
Myth #2: All Clots Are Dangerous
Not every clot poses a life‑threatening risk. Small clots can form in areas like the skin (a superficial thrombophlebitis) and resolve without intervention. The serious ones are those that block major veins or travel to the lungs (PE). Understanding the difference matters: superficial clots usually cause localized redness and tenderness, while DVT leads to swelling, warmth, and sometimes a “heavy” feeling in the leg.
Myth #3: Taking Aspirin Prevents All Clots
Aspirin inhibits platelets, which helps prevent arterial clots that cause heart attacks. However, most venous clots (DVT/PE) arise from the coagulation cascade, not platelet aggregation. Therefore, aspirin alone is insufficient for most DVT risk profiles. Doctors prescribe direct oral anticoagulants (DOACs) or warfarin for proven or high‑risk venous clots because they target the cascade more effectively.
Myth #4: You Can “Break Up” a Clot With Heat or Massage
Applying heat or massaging a suspected clot is dangerous. Heat dilates vessels, potentially facilitating the clot’s migration to the lungs. Massage can dislodge a clot, causing a sudden PE. The safest approach is to immobilize the leg, elevate it, and seek medical assessment. Treatment will involve anticoagulation and, in some cases, clot‑removing procedures.
Myth #5: Once You’re On Blood‑Thinners, You’re Safe Forever
Anticoagulants reduce the chance of new clots forming and limit growth of existing ones, but they do not guarantee permanent protection. Therapy length depends on the underlying cause-temporary risk factors (like post‑surgery) may only need 3‑6 months, whereas genetic thrombophilia often needs lifelong therapy. Stopping medication without a doctor’s guidance can lead to rebound clotting.

Myth #6: Compression Stockings Cure Existing DVT
Compression stockings are fantastic for preventing clot formation after surgery or during long flights because they improve venous return. However, once a clot has formed, stockings do not dissolve it. They are used adjunctively after anticoagulation starts to reduce swelling and prevent post‑thrombotic syndrome (chronic leg pain). Misusing them as a cure can delay proper treatment.
Myth #7: Only Older Adults Get Clots
Age is a risk factor-older adults have higher clot incidence-but younger people are not immune. Athletes on hormonal contraceptives, long‑haul travelers, and individuals with inherited clotting disorders (like Factor V Leiden) can develop clots in their 20s or 30s. Recognizing personal risk profiles is key, regardless of age.
Fact‑Check Table: Myth vs. Reality
| Myth | Reality |
|---|---|
| Cold weather causes clots | Reduced activity in cold months raises risk, not temperature itself. |
| All clots are life‑threatening | Only clots that block major veins or travel to lungs pose serious danger. |
| Aspirin prevents every clot | Aspirin helps arterial clots; venous clots need anticoagulants. |
| Heat or massage breaks up clots | Heat can spread clot; massage may cause PE. Seek medical care. |
| Blood‑thinners cure you forever | Therapy length varies; stopping early increases risk. |
| Compression stockings cure DVT | They prevent clots and reduce swelling after treatment, but don’t dissolve clots. |
| Only seniors get clots | Younger adults with risk factors can develop clots too. |
How to Spot a Dangerous Clot: A Quick Checklist
- Leg swelling that’s uneven or unilateral.
- Pain or cramping that feels worse when standing.
- Warmth or redness over the affected area.
- Sudden shortness of breath, chest pain, or rapid heartbeat - possible PE.
- Recent surgery, long‑haul travel, or immobilization.
If two or more of these appear, call emergency services or visit the nearest emergency department.
Prevention Strategies That Actually Work
Beyond debunking myths, here are evidence‑based steps to lower clot risk:
- Stay mobile: Take a 5‑minute walk every hour on long flights or road trips.
- Hydrate: Dehydration thickens blood; aim for at least 2L of water daily.
- Wear graduated compression stockings: Especially after surgery or during prolonged sitting.
- Manage medications: Discuss hormonal contraceptives, hormone therapy, or chemotherapy with your doctor.
- Know your family history: Inherited clotting disorders warrant early screening.
When to Seek Professional Help
Self‑diagnosis is risky. If you notice any of the checklist symptoms, especially sudden breathlessness, treat it as an emergency. Primary care can order a duplex ultrasound for DVT or a CT pulmonary angiogram for PE. Early detection dramatically improves outcomes.

Frequently Asked Questions
Can a clot form in the arm?
Yes. Upper‑extremity DVT is less common but can occur after central venous catheters, heavy lifting, or repetitive motion injuries. Symptoms mirror leg DVT-swelling, pain, and a feeling of tightness.
Do I need lifelong anticoagulation if I’ve had a clot?
Not always. If the clot was provoked by a temporary factor (e.g., surgery), a 3‑to‑6‑month course may suffice. Persistent risk factors (genetic clotting disorders, cancer) often require indefinite therapy.
Is ultrasound reliable for diagnosing DVT?
Compression ultrasound is the gold standard for lower‑leg DVT. It visualizes veins and checks for compressibility; an inability to compress indicates a clot.
Can COVID‑19 increase clot risk?
Severe COVID‑19 triggers inflammation and endothelial injury, both of which raise clot risk. Hospitalized patients often receive prophylactic anticoagulants to counteract this.
Are there natural ways to thin the blood?
Foods rich in omega‑3 fatty acids (salmon, flaxseed) and compounds like garlic or ginger have mild antiplatelet effects, but they cannot replace prescribed anticoagulants for high‑risk patients.
Understanding the facts behind blood clot myths empowers you to act quickly, avoid unnecessary scares, and follow proven prevention measures. Stay aware, stay active, and don’t let misinformation dictate your health decisions.








15 Comments
If you’re worried about clots after a flight, the first thing to check is your mobility. Keep your legs moving every hour, stand up, stretch, and flex your calves. Deep vein thrombosis rarely appears out of nowhere; it needs prolonged stasis, dehydration, or a pro‑thrombotic trigger. Compression stockings are useful *only* after a clot has been ruled out and you’re in a recovery phase. Do not rely on “cold weather” as an excuse to stay still-use that time to walk around. If you notice swelling that’s unequal, pain that worsens with standing, or a sudden sense of heaviness, seek medical attention immediately. Remember, anticoagulants will not dissolve an existing clot in minutes; they prevent it from growing. Stay proactive and set a reminder to move every 60 minutes on long trips.
The tragedy of a silent clot is that it can strike while you’re lost in the sunrise.
Yo fam, keep that blood flowin’ like a river! 🚶♂️💦 Every hour on a long road trip, hop outta the seat and do a quick leg swing-no excuses. Hydration is key, so chug that H2O like you’re in a marathon. If you feel that weird ache in your calf, don’t ignore it; it could be the early warning sign of DVT. Stay active, stay alive, and keep the vibe positive!
Absolutely, Patrick! 🙌 Staying mobile is the #1 defense, and those simple leg exercises can make a huge difference. Adding a pair of graduated compression socks after surgery or a flight can further boost venous return. Remember to elevate the leg slightly if you notice swelling-gravity helps the blood move back up. Keep spreading the good habits, and let’s keep each other motivated! 😊
Move frequently!; Hydrate well!; Check for swelling!; Seek help if breathless!; Simple steps save lives!
Listen, folks-stop using myths as an excuse to sit on your butt. The only thing that actually kills you is *inactivity* and ignoring the warning signs. If you’re on a plane, get up every 30‑40 minutes, stretch those calves, and drink water. No one needs a lecture on cold weather; the real danger is staying still. Take charge of your health now, or you’ll pay later.
Great points already shared, everyone. Just to add a quick clarification: ultrasound isn’t just “some scan”-it specifically looks for vein compressibility, which is the gold standard for DVT diagnosis. If you’re unsure about the difference between a superficial thrombophlebitis and a deep vein clot, remember that the former usually involves only skin redness and tenderness, while the latter brings swelling, warmth, and a heavy feeling. Also, compression stockings should be worn correctly, with the right pressure gradient, to be effective. Keep the conversation going, and feel free to ask for more details!
Clot or not, the blood seeks equilibrium; interference merely delays fate.
Life’s a river and our blood is its swift current dancing through veins and arteries it’s a wild ride when a clot tries to dam the flow we gotta keep moving stay hydrated and never let that silent thief steal our breath
America ain’t gonna let some bogus cold myth keep us down we need real info not old wives tale get up move your legs and protect yourself
Honestly, all this hype about clot myths is just another scare tactic-people forget that most of us never get a DVT unless we’re just sitting around binge‑watching TV all day
I get why that feels frustrating, Mike. While it’s true that many clot cases stem from prolonged sitting, dismissing the real risks can leave folks unprepared. Remember, a single flight or a surgery can tip the balance for someone with an underlying clotting disorder. So, let’s keep spreading the practical tips-stay active, hydrate, and watch for warning signs. Together we can make a real difference.
From a hemostatic perspective, the formation of a thrombus is governed by the intricate interplay of endothelial integrity, blood flow dynamics, and the coagulation cascade, often encapsulated by Virchow’s triad. Contemporary literature delineates that venous thromboembolism (VTE) predominately arises secondary to stasis rather than hypercoagulability in the acute postoperative milieu. Consequently, prophylactic regimens employ low‑molecular‑weight heparins or direct oral anticoagulants to attenuate factor Xa activity, thereby mitigating thrombin generation. Empirical evidence underscores that compression therapy, when applied with graduated pressures of 30‑40 mmHg, expedites venous return and reduces venous hypertension, albeit without intrinsic thrombolytic capacity. It is a common misconception that thermal modalities such as heat can resolve an established embolus; thermally induced vasodilation may inadvertently facilitate embolization to the pulmonary arterial tree. Moreover, the pharmacodynamics of anticoagulants reveal a latency period before achieving therapeutic plasma concentrations, necessitating bridging strategies in high‑risk patients. Imaging modalities, notably compression duplex ultrasonography, demonstrate a sensitivity exceeding 95 % for proximal lower‑extremity DVT when performed by experienced sonographers. Conversely, computed tomography pulmonary angiography remains the diagnostic cornerstone for acute pulmonary embolism, offering both anatomical delineation and quantification of clot burden. In patients possessing hereditary thrombophilias, such as Factor V Leiden, lifelong anticoagulation is frequently advocated, balanced against the hemorrhagic risk profile. Clinical guidelines further recommend that aspirin, despite its antiplatelet properties, lacks efficacy in primary prophylaxis of venous thromboembolism, a nuance often obscured in lay discourse. Hydration status exerts a modulatory effect on plasma viscosity; hypovolemia can augment coagulability through hemoconcentration. The epidemiological surge of VTE in the context of COVID‑19 infection is attributable to endothelial dysfunction and cytokine‑mediated hypercoagulability, reinforcing the necessity for prophylactic anticoagulation in hospitalized cohorts. Ultimately, patient education should emphasize not only the mechanical aspects of mobility and compression but also the temporal dimensions of therapeutic intervention. By integrating pathophysiological insight with evidence‑based practice, clinicians can transcend mythologized narratives and deliver nuanced care. Such an approach not only reduces morbidity but also curtails the healthcare costs associated with delayed diagnosis.
That was a solid rundown, Stephen. I appreciate the way you broke down the science without drowning us in jargon. For the rest of us, the key takeaway is simple: move, stay hydrated, and follow your doctor's anticoagulation plan. Thanks for keeping it real.
Good summary, everyone. Remember, early detection saves lives.