When you're taking an ACE inhibitor like lisinopril or enalapril to control your blood pressure, you might not think twice about eating a banana or a baked potato. But here’s the thing: those foods could be quietly raising your potassium levels - and that’s not always safe.
Why ACE Inhibitors Raise Potassium Levels
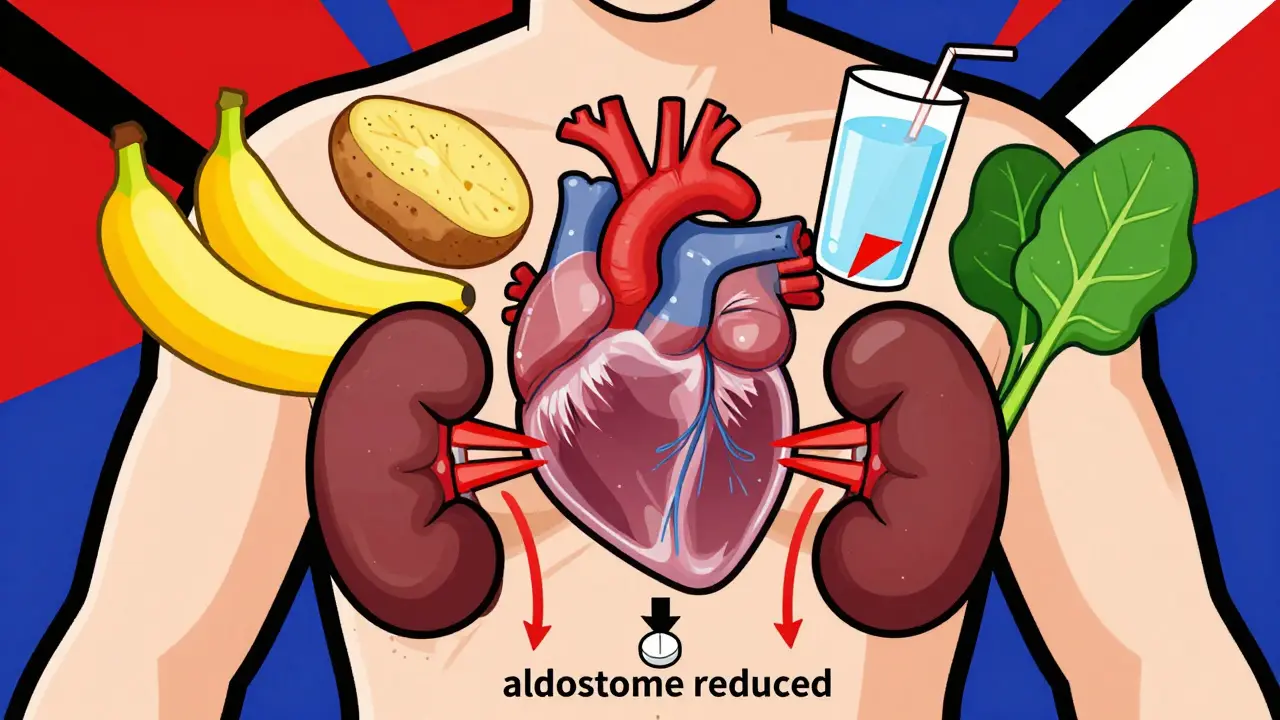
ACE inhibitors work by blocking a hormone called angiotensin II, which normally causes blood vessels to tighten. By relaxing those vessels, they lower blood pressure. But there’s a side effect you rarely hear about: they also reduce a hormone called aldosterone. Aldosterone tells your kidneys to flush out extra potassium. When it drops, your body holds onto potassium instead. That’s not a problem for most people with healthy kidneys. But if your kidneys aren’t working at full speed - which happens often with age, diabetes, or chronic kidney disease - that extra potassium builds up. And when serum potassium climbs above 5.0 mmol/L, you’re in danger of hyperkalemia. At levels above 6.0 mmol/L, it can trigger dangerous heart rhythms or even cardiac arrest. Studies show that in people with normal kidney function, the annual risk of hyperkalemia from ACE inhibitors is around 1.2%. But for someone with stage 3 or 4 chronic kidney disease, that risk jumps to nearly 13%. And if you’re diabetic? Your risk is more than three times higher than someone without diabetes.Which Foods Are the Biggest Culprits?
You don’t need to give up fruits and veggies - but you do need to know which ones pack the most potassium. A single banana has about 326 mg. A medium baked potato? Around 926 mg. One cup of cooked spinach? 839 mg. And if you’re drinking coconut water - popular as a "natural energy drink" - you’re getting over 1,500 mg of potassium in just one serving. Here’s a quick look at common high-potassium foods and their approximate potassium content per typical serving:- Avocado (½ medium): 485 mg
- Orange (1 medium): 237 mg
- Tomato (1 cup, raw): 427 mg
- White potato (1 medium, baked): 926 mg
- Sweet potato (1 medium, baked): 700 mg
- Dried apricots (½ cup): 1,100 mg
- Coconut water (1 cup): 1,500 mg
- Salt substitute (1.25 g): 525 mg
It’s Not Just Food - It’s What You Combine
The real danger isn’t just one banana. It’s the combo. Many people on ACE inhibitors are also prescribed spironolactone, a potassium-sparing diuretic. When you mix these two, your risk of hyperkalemia triples. That’s not a small increase - it’s a red flag. In fact, some studies show the risk is 300-400% higher than taking an ACE inhibitor alone. Even over-the-counter supplements can be risky. Potassium chloride tablets, herbal teas like dandelion root, or even salt substitutes labeled "low sodium" often contain potassium chloride. People assume they’re healthier - but for someone on an ACE inhibitor, they’re a hidden hazard. And timing matters. Research shows that eating high-potassium foods two hours before or after taking your ACE inhibitor reduces the peak potassium spike by about 25%. That’s a simple, practical way to lower your risk without cutting out foods entirely.
Who’s Most at Risk?
Not everyone needs to worry. But some groups should be extra careful:- People over 65 - kidney function naturally declines with age
- Those with diabetes - even early-stage kidney damage increases risk
- Patients with chronic kidney disease (CKD) stages 3-4
- People taking multiple medications that affect potassium
- Those who’ve had a previous episode of high potassium
What Do Experts Really Say?
There’s disagreement among doctors - and that’s confusing for patients. Some, like Dr. Alan H. Gradman, argue that dietary potassium rarely causes serious hyperkalemia in people with normal kidneys. He says fewer than 0.5% of patients on ACE inhibitors develop dangerous levels from food alone. But others, like Dr. Suzanne Oparil, warn that older adults often don’t feel symptoms until it’s too late. Muscle weakness, nausea, or an irregular heartbeat might seem like "just getting older" - until it’s a heart attack. The American Society of Hypertension recommends blood tests every 3-6 months for people with normal kidney function. But if you have diabetes or CKD, they want you tested every month - especially when starting the drug or changing the dose. And here’s something surprising: a 2016 study in the Journal of the American College of Cardiology found that people with normal kidneys who ate 3,400-4,700 mg of potassium daily - the amount recommended for heart health - didn’t develop hyperkalemia while on ACE inhibitors or ARBs. That challenges the old idea that everyone on these drugs must avoid potassium-rich foods.What Should You Do?
Here’s what works in real life:- Get tested. Ask your doctor for a baseline potassium test before starting an ACE inhibitor. Then get checked again after 1-2 weeks, and every 3-6 months if you’re stable.
- Know your numbers. Normal potassium is 3.5-5.0 mmol/L. Anything above 5.0 is a warning. Above 6.0? That’s an emergency.
- Track your intake. Use a free app like MyFitnessPal to log your meals for a week. You might be shocked at how much potassium you’re getting.
- Be smart with salt substitutes. If you’re using them to cut sodium, ask your doctor for a potassium-free alternative. Many contain potassium chloride - which is dangerous with ACE inhibitors.
- Don’t panic about fruits. You don’t need to avoid bananas or avocados entirely. But if you’re eating them daily and have kidney issues, talk to your doctor or a dietitian. One banana a day is usually fine. Two? Maybe not.
- Space out your meals. Try to eat high-potassium foods at least two hours before or after taking your ACE inhibitor. It’s a small change with a measurable effect.
What About Alternatives?
If you’re worried about potassium, ask your doctor about angiotensin II receptor blockers (ARBs), like losartan or valsartan. They work similarly to ACE inhibitors but carry about 60% of the hyperkalemia risk. Calcium channel blockers or thiazide diuretics are even safer for potassium levels - though they might not work as well for kidney protection in diabetics. And if you’ve already had a high potassium episode, there’s a newer option: patiromer (Veltassa). This medication binds potassium in your gut so your body doesn’t absorb it. Clinical trials show 89% of patients who took it could safely stay on their ACE inhibitor without needing to switch drugs.Bottom Line
You don’t have to live on a low-potassium diet just because you’re on an ACE inhibitor. But you do need to be informed. For most people with healthy kidneys, a banana or two a day won’t hurt. But if you’re over 65, diabetic, or have kidney disease - you need to be cautious. The real risk isn’t the food. It’s the silence. Too many people don’t know about this interaction until they’re in the ER with a dangerously high potassium level. Don’t be one of them. Ask your doctor for a blood test. Talk to a dietitian. Track your intake. Small steps can prevent a big crisis.Can I still eat bananas if I’m on an ACE inhibitor?
Yes - but it depends. If you have healthy kidneys and no other risk factors, one banana a day is generally safe. If you have diabetes, chronic kidney disease, or are taking other medications like spironolactone, even one banana daily could raise your potassium to dangerous levels. Always get your blood potassium tested before assuming it’s fine.
How do I know if my potassium is too high?
You won’t always feel it. Early signs include muscle weakness, fatigue, nausea, or an irregular heartbeat. But many people have no symptoms until their potassium is dangerously high - over 6.0 mmol/L. The only reliable way to know is through a blood test. Don’t wait for symptoms. Get tested regularly if you’re on an ACE inhibitor.
Is coconut water safe with ACE inhibitors?
No - not if you’re at risk. One cup of coconut water contains about 1,500 mg of potassium, which is more than half the daily recommended limit for someone on an ACE inhibitor with kidney issues. There are documented cases of patients being hospitalized after drinking coconut water daily while on lisinopril. Avoid it unless your doctor says it’s safe.
Should I stop eating potatoes and tomatoes?
Not necessarily. A medium baked potato has nearly 900 mg of potassium - that’s a lot. But if you eat it once a week and your potassium levels are normal, it’s probably fine. The key is balance and monitoring. If you’re eating potatoes, tomatoes, avocados, and bananas every day, you’re likely overloading. Cut back gradually and get tested.
Can I take potassium supplements with ACE inhibitors?
Never without your doctor’s approval. Potassium supplements can push your levels into the danger zone, especially if you’re also taking a diuretic or have kidney problems. Most people get enough potassium from food. Supplements are rarely needed - and often dangerous - when you’re on an ACE inhibitor.
Are there any ACE inhibitors that are safer for potassium?
Lisinopril appears to carry a slightly lower risk of hyperkalemia than enalapril or captopril, based on head-to-head studies. But the difference is small. The bigger factor is your kidney function and other medications - not which ACE inhibitor you’re on. Always focus on monitoring and lifestyle, not just the drug name.
What should I do if I miss a potassium test?
Don’t wait. Call your doctor and ask for a blood test. If you’ve been on an ACE inhibitor for more than 3 months without a check-up, you’re overdue. Most guidelines say testing every 3-6 months is standard. If you have kidney disease or diabetes, you should be tested monthly. Skipping tests is one of the most common reasons people end up in the hospital with hyperkalemia.






14 Comments
Been on lisinopril for 5 years and still eat bananas like it’s a sport. Got my labs done last month - potassium was 4.8. No drama. If your kidneys are good, don’t stress. Your body’s not a bomb. It’s a machine that knows how to balance stuff.
I’m 72 with type 2 diabetes and CKD stage 3. My nephrologist told me to avoid coconut water like it’s poison. I used to drink it daily thinking it was healthy. Now I stick to apple juice and water. Small changes save lives.
It is imperative to recognize that the pharmacodynamic interaction between angiotensin-converting enzyme inhibitors and dietary potassium intake is mediated through the renin-angiotensin-aldosterone system. Aldosterone suppression leads to decreased distal tubular potassium excretion, thereby increasing serum concentration. This is not a trivial matter in patients with impaired renal function.
wait so i can still eat sweet potatoes?? i thought i had to give up everything. my wife makes these crazy roasted sweet potato wedges and i eat them like 3x a week. if i just space them out from my pill time, im cool? i feel like a genius
So many people panic about food when the real issue is lack of monitoring. Get your blood tested. Talk to your doctor. Don’t let fear make you miss out on good food. You’re not broken, you’re just managing.
The human body evolved in an environment where potassium was abundant and sodium scarce. Modern diets have inverted this balance, yet we treat potassium as if it were a toxin. Perhaps the issue is not the food, but the confluence of aging, polypharmacy, and medicalized fear. We have forgotten that physiology is not a spreadsheet.
So let me get this straight… I can’t have a baked potato because of a pill, but I can drink 3 energy drinks with 200mg caffeine each? Cool. I’ll just swap my potatoes for Red Bulls. Thanks, medicine.
Big Pharma doesn’t want you to know this, but potassium is actually a natural blood pressure reducer - they’re scared people will stop taking their drugs and just eat bananas. That’s why they scare you with ‘hyperkalemia.’ It’s a profit play. Your kidneys are fine. Trust your body.
From a pharmacokinetic standpoint, the CYP3A4-mediated metabolism of ACE inhibitors is not significantly impacted by dietary potassium, but the renal excretion threshold is critically dependent on GFR. In CKD stages 3-4, tubular secretion capacity is compromised, leading to non-linear accumulation kinetics. Hence, the 13% incidence rate isn't anecdotal - it's biologically deterministic.
they put potassium in salt substitutes on purpose so you get hooked on the pill then they sell you veltassa for 2k a month. its all a scheme. i stopped taking my med and now i eat 5 bananas a day. my bp is better and my heart feels lighter. they dont want you to know this.
People who don’t track their potassium intake are just being irresponsible. It’s not rocket science - use MyFitnessPal, stop eating avocado toast, and maybe don’t drink coconut water like it’s Gatorade. If you’re too lazy to read labels, don’t be surprised when you end up in the ER.
So… I’m supposed to be scared of potatoes but not scared of my 12 pills a day? This is why I hate doctors. They make you feel guilty for eating food while ignoring that your meds are literally a chemical bomb.
i just checked my last blood test… potassium was 5.1… should i be worried?? i eat one banana a day and a cup of tomato sauce… is that too much?? i dont know what to do anymore
My grandma’s on lisinopril and eats sweet potatoes every Sunday. She’s 81, no hospital visits, walks 3 miles a day. If she’s fine, maybe we’re overcomplicating this. Listen to your body - not just the numbers.