
When standard asthma treatments like inhalers and steroids stop working, many patients face a brutal reality: constant flare-ups, emergency room visits, and reliance on oral steroids that wreck their bones, blood sugar, and mood. For these people, biologics aren’t just another option-they’re a lifeline. Two of the most impactful classes are anti-IgE and anti-IL-5 therapies, which target the root causes of severe asthma instead of just masking symptoms.
What Exactly Are Biologics?
Biologics are not pills or generic drugs. They’re made from living cells-usually from mice or bacteria-that are engineered in labs to act like precision missiles. Unlike traditional asthma meds that calm inflammation broadly, biologics zero in on one specific molecule in the immune system that’s driving the problem. Think of it like using a key to unlock a single door instead of smashing down the whole wall.
They’re given as injections under the skin, usually once every few weeks. Some, like reslizumab, require an IV infusion. Most patients learn to self-administer after a few training sessions. The big advantage? They work for people who just don’t respond to anything else.
Anti-IgE: Targeting the Allergy Pathway
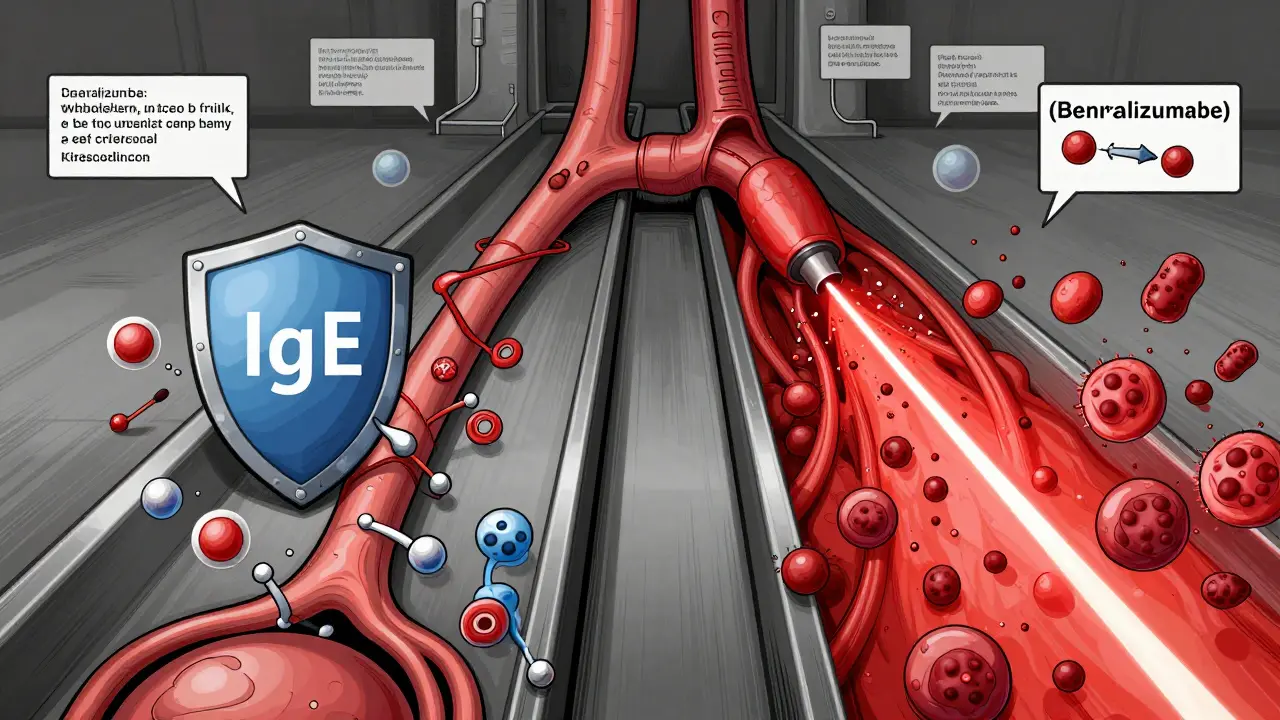
Omalizumab (brand name Xolair) was the first biologic approved for asthma back in 2003. It blocks immunoglobulin E, or IgE-the antibody that triggers allergic reactions. When you’re allergic to dust mites, pollen, or pet dander, your body overproduces IgE. This binds to mast cells and basophils, which then explode with histamine and other inflammatory chemicals. That’s what causes wheezing, coughing, and tightening in the chest.
Omalizumab sticks to IgE before it can bind, stopping the chain reaction. It’s only effective for people with allergic asthma, confirmed by a positive skin test or blood test showing elevated allergen-specific IgE. Blood total IgE levels must be between 30 and 1500 IU/mL. If you don’t have allergies, omalizumab won’t help.
Studies show it cuts asthma exacerbations by about 50%. In the landmark INNOVATE trial, patients on omalizumab had far fewer ER visits and hospital stays. Many also reduced or stopped oral steroids entirely. But it takes time. Some feel better in 4 weeks. Others need 12 to 16 weeks before they notice a real difference.
Anti-IL-5: Going After Eosinophils
While anti-IgE targets allergies, anti-IL-5 drugs tackle a different problem: too many eosinophils. These are white blood cells that swarm the airways in certain types of severe asthma, causing chronic swelling and mucus buildup. This is called eosinophilic asthma.
Three drugs fall into this category: mepolizumab (Nucala), reslizumab (Cinqair), and benralizumab (Fasenra). All block IL-5, a signaling protein that tells eosinophils to multiply and stick around. But they work differently.
Mepolizumab and reslizumab bind directly to IL-5, so it can’t reach its target. Benralizumab is sneakier-it latches onto the IL-5 receptor on eosinophils themselves. This triggers the immune system to kill those cells on the spot. That’s why benralizumab can wipe out nearly all circulating eosinophils within 24 hours. Mepolizumab takes weeks.
Patients need a blood test showing at least 150 eosinophils per microliter (or 300 in the past year) to qualify. In the MENSA and ZONDA trials, these drugs cut exacerbations by over 50%. Like omalizumab, they also reduce steroid use. One patient on Reddit said, “After six months on mepolizumab, I went from 3-4 ER trips a year to zero.”
How Do They Compare?
Choosing between anti-IgE and anti-IL-5 isn’t about which is “better.” It’s about matching the drug to the patient’s biology.
| Feature | Anti-IgE (Omalizumab) | Anti-IL-5 (Mepolizumab, Benralizumab) |
|---|---|---|
| Target | Immunoglobulin E (IgE) | Interleukin-5 (IL-5) or its receptor |
| Best for | Allergic asthma with elevated IgE | Eosinophilic asthma with high blood eosinophils |
| Typical dose frequency | Every 2-4 weeks | Every 4 weeks (mepolizumab/reslizumab); every 8 weeks after initial doses (benralizumab) |
| Administration | Subcutaneous injection | Subcutaneous (mepolizumab, benralizumab); IV infusion (reslizumab) |
| Time to effect | 4-16 weeks | 4-12 weeks (benralizumab acts faster on eosinophils) |
| Reduction in exacerbations | ~50% | 51-52% |
| Biomarker required | Serum IgE level (30-1500 IU/mL) | Blood eosinophils ≥150-300 cells/μL |
One key difference: anti-IgE doesn’t work during an active flare. It’s preventive. Anti-IL-5 drugs, especially benralizumab, can reduce inflammation even if eosinophils are already high. That’s why some doctors prefer them for patients with frequent, unpredictable attacks.
Real-World Challenges
These drugs aren’t magic. They come with hurdles.
- Cost: Annual treatment runs $25,000-$40,000 USD. Insurance often requires prior authorization, which can take 2-3 weeks.
- Side effects: Most are mild-headaches, sore throat, or pain at the injection site. About 1 in 10 people experience these. Severe allergic reactions (anaphylaxis) are rare-about 1 in 1,000 doses-but more likely if you’ve had serious allergies before.
- Not everyone responds: Real-world data shows 30-40% of patients don’t improve meaningfully. That’s why biomarkers are non-negotiable. If your IgE is low or your eosinophils are normal, these drugs won’t help.
- It’s add-on therapy: Biologics only work if you’re already taking your inhalers correctly and consistently. Skipping doses or using the wrong technique will make biologics look like they failed.
One patient on Reddit shared, “Benralizumab gave me great control, but the joint pain after the third shot was unbearable. I had to stop.” That’s why tracking side effects matters. What works for one person might not work for another.
Who Gets These Drugs?
Guidelines from the European Respiratory Society and GINA are clear: biologics are only for patients with severe asthma who’ve tried everything else. That means:
- Using high-dose inhaled corticosteroids and long-acting beta agonists daily
- Having good inhaler technique (confirmed by a nurse or specialist)
- Proving poor adherence isn’t the problem
- Having documented exacerbations (at least 2 in the past year)
- Having a biomarker that matches the drug: IgE for omalizumab, eosinophils for anti-IL-5
It’s not a first-line option. It’s the last step before a patient’s life gets taken over by asthma.
What’s Next?
The field is moving fast. Tezepelumab (Tezspire), approved in 2021, targets TSLP-an upstream protein that triggers multiple pathways, even in non-eosinophilic asthma. It’s the first biologic that works regardless of biomarker levels. That’s huge.
Researchers are testing twice-yearly injections. One trial is looking at combining biologics. And in June 2024, the FDA approved ensifentrine, the first oral biologic-like drug for asthma, though it works differently.
Right now, only 1-2% of eligible patients get biologics. The main reasons? Cost, access, and lack of awareness. But as more generics arrive and testing gets easier, that number should climb.
Final Thoughts
For someone stuck in a cycle of steroid dependence, ER visits, and missed work, biologics can mean the difference between surviving and living. Anti-IgE and anti-IL-5 therapies don’t cure asthma-but they give control back. When used right, with proper testing and support, they’re not just effective. They’re transformative.
But they’re not for everyone. And they’re not a replacement for good asthma management. They’re the final tool in a toolkit-when everything else has been tried.
Are biologics a cure for severe asthma?
No, biologics are not a cure. They don’t eliminate asthma. Instead, they reduce inflammation caused by specific immune pathways, leading to fewer flare-ups, hospital visits, and steroid use. Patients still need to take their regular inhalers and avoid triggers. Biologics are a long-term management tool, not a one-time fix.
How long does it take to see results from anti-IgE or anti-IL-5 therapy?
Most patients start noticing improvements within 4 to 12 weeks. Some feel better sooner, especially with benralizumab’s rapid effect on eosinophils. But full benefits-like fewer hospitalizations or reduced steroid use-often take 12 to 16 weeks. Patience is key. Stopping too early means missing the real benefit.
Can I stop my inhalers if I start a biologic?
Absolutely not. Biologics are add-on therapies. You must keep using your inhaled corticosteroids and long-acting bronchodilators as prescribed. Stopping them can trigger a dangerous flare-up. Biologics work best when combined with optimized standard care. They’re designed to reduce the damage caused by inflammation, not replace the foundation of asthma control.
Why do I need blood tests before starting a biologic?
Because these drugs only work if your asthma matches their target. Omalizumab needs high IgE levels and evidence of allergies. Anti-IL-5 drugs need elevated eosinophils. Giving them to someone without those biomarkers is like using a key that doesn’t fit the lock. Testing prevents wasted time, money, and false hope. It’s how doctors pick the right tool for your body.
Is it worth the cost?
For many, yes. While annual costs range from $25,000 to $40,000, studies show patients on biologics save money long-term by avoiding ER visits, hospital stays, and oral steroid side effects. One study found that for every $1 spent on biologics, $2-$3 was saved in other healthcare costs. If you’re having 3-4 hospitalizations a year, the math often adds up. Insurance coverage and patient assistance programs can also cut costs significantly.





10 Comments
Let me get this straight-you’re telling me we’re spending $40k a year to block a single protein like it’s some kind of sci-fi sniper rifle? Meanwhile, people in developing countries are still using nebulizers powered by bicycle pumps. This isn’t medicine, it’s luxury healthcare performance art. And don’t even get me started on the ‘biomarker required’ nonsense. You mean to tell me if your eosinophils are 149 instead of 150, you’re just screwed? That’s not science, that’s a spreadsheet with delusions of grandeur.
When we speak of biologics we speak not merely of molecules but of the metaphysical rupture between the body as machine and the body as sacred text
The IgE is not merely an antibody but a mirror of the soul’s allergic response to a world that has forgotten silence
IL-5 is not a cytokine but a cry from the lungs begging to be heard beyond the noise of pharmaceutical capitalism
Perhaps the real biologic is the patient who dares to believe in healing when the system says no
And yet we measure in microliters and dollars and forget that healing cannot be quantified by a lab report
The body does not care for your biomarkers it only asks for breath
And breath is not patented
It is not insured
It is not regulated
It simply is
And in that simplicity lies the true biologic
For anyone feeling overwhelmed by the jargon-this stuff is actually way simpler than it looks.
Think of your asthma like a faulty alarm system. Traditional inhalers are like turning the volume down on the siren. Biologics? They’re rewiring the alarm so it doesn’t go off at all.
Omalizumab doesn’t just ‘block IgE’-it removes the trigger that tells your body to panic over harmless stuff like cat hair or pollen. That’s why allergic asthma patients feel like they’ve been given back their lives.
And anti-IL-5? It’s not just reducing eosinophils-it’s telling those overzealous immune cells to go home and take a nap. Benralizumab doesn’t just calm them down-it deletes them. Like a clean sweep.
Yes, they’re expensive. But if you’re avoiding one ER visit a year, you’ve already paid for it. And yes, you still need your inhalers. Biologics aren’t magic. They’re precision tools.
And if you’re not getting results after 12 weeks? Talk to your doc. Maybe you’re on the wrong one. But don’t give up. These drugs change lives.
Why do Western countries treat asthma like a luxury problem? In India, we have children breathing through cloth masks because there’s no clean air. We don’t have biologics-we have hope. And hope doesn’t come with a $40,000 price tag. This is not progress. This is exclusion dressed up as innovation. You call it medicine. I call it colonial medicine-only for those who can afford to be sick properly.
Meanwhile, our doctors use nebulizers made from bicycle pumps and pray. But we still breathe. We still live. And we still outlive your expensive little antibodies.
I’ve been on benralizumab for a year now and I can’t believe I waited this long. I used to wake up gasping every other week. Now? I went on a hike last weekend. Without my inhaler. Just me, the trail, and the wind. I didn’t even think about asthma. That’s wild.
It took 10 weeks to feel it. First, the nighttime cough stopped. Then the wheeze. Then the fear. I’m not saying it’s perfect-my arm still stings after the shot-but it’s like someone turned down the volume on my lungs. And I didn’t even know how loud it was until it got quiet.
If you’re on the fence? Do the blood test. Talk to your allergist. Don’t let cost scare you off-ask about patient programs. This isn’t a miracle. It’s a second chance. And you deserve it.
Biologics? More like biologic-bullshit. Every single one of these drugs was developed by a pharma company that spent 12 years patenting a molecule and 13 years marketing it as ‘revolutionary.’ Meanwhile, the real solution? Clean air. Less pollution. Better housing. But no, let’s just inject people with lab-grown proteins and call it a day.
And the biomarkers? Total nonsense. I’ve seen three patients with identical eosinophil counts-one responded, two didn’t. So what’s the science? Guesswork with a lab coat.
Also, why is no one talking about the fact that these drugs make you more susceptible to parasitic infections? Because it’s not in the ads. They don’t want you thinking about worms. They want you thinking about your inhaler.
Just wanted to say thank you for this post. I’ve been on omalizumab for 18 months and honestly? I didn’t think I’d ever feel normal again. I used to cancel plans because I was scared I’d have an attack. Now I’m back at work full-time, hiking on weekends, and even adopted a cat (yes, I’m allergic but I’m not having a meltdown anymore). It’s not magic, but it’s the closest thing I’ve had to a reset button. Keep going, folks. It takes time, but it’s worth it.
I read this whole thing and just cried. Not because I’m sad, but because I finally feel seen. I’ve been told for years that my asthma was ‘just bad luck.’ But the truth? My body was screaming and no one was listening. When they tested my eosinophils and said I qualified for mepolizumab, I thought it was a joke. But now, after 8 months, I haven’t been to the ER. I sleep through the night. I can walk up stairs without stopping. This isn’t just medicine. It’s dignity.
As someone who’s been on both anti-IgE and anti-IL-5, I’ll say this: the biggest difference isn’t the science-it’s the waiting. Omalizumab took 4 months to feel anything. Benralizumab? I felt it by week 6. The difference in quality of life was night and day. I wish I’d known that sooner.
Also, the injection site pain? Totally worth it. I used to have to carry my inhaler like a security blanket. Now I just carry a small cooler for my meds. Small price for breathing without fear.
And yes, the cost sucks. But if your insurance denies it, keep pushing. I had to appeal three times. Now I’m on a patient assistance program. Don’t give up.
OMG I’m so glad someone finally said this. I’ve been on benralizumab for 2 years and my joint pain is TERRIBLE. Like, I can’t open jars anymore. But my doctor says it’s ‘just a side effect’ and ‘not serious.’ 😂 Like, I’m 32 and I can’t carry groceries? What’s the point of breathing better if I can’t hold a spoon? And don’t even get me started on the fact that I have to go to a clinic every 8 weeks to get a shot that costs more than my rent. I’m not rich. I’m not a guinea pig. I’m just trying to live. 🤦♀️