For decades, proving that a generic drug works the same as the brand-name version meant putting healthy volunteers through blood draws, timed dosing, and weeks of monitoring. Those in vivo bioequivalence studies cost up to $2 million each and took months to complete. But now, a smarter, faster, and cheaper method is taking over-in vitro testing backed by IVIVC.
What Is IVIVC, Really?
IVIVC stands for In Vitro-In Vivo Correlation. It sounds technical, but it’s simple in principle: if you can predict how a drug behaves in the human body just by testing how it dissolves in a lab beaker, you don’t need to give it to people at all. That’s the whole point.The U.S. FDA first laid out the rules in 1996, but it wasn’t until the 2014 update that companies started taking it seriously. IVIVC links a drug’s dissolution rate-how quickly it breaks down in a simulated stomach environment-to its actual absorption in the bloodstream. If the lab test matches what happens in the body, you’ve got a scientifically valid shortcut.
This isn’t theory. It’s been used successfully for extended-release pills like oxycodone, metformin, and diltiazem. Teva saved five full bioequivalence studies after building a solid IVIVC model. That’s over $10 million in avoided costs and 18 months shaved off development time.
The Four Levels of IVIVC: Which One Matters?
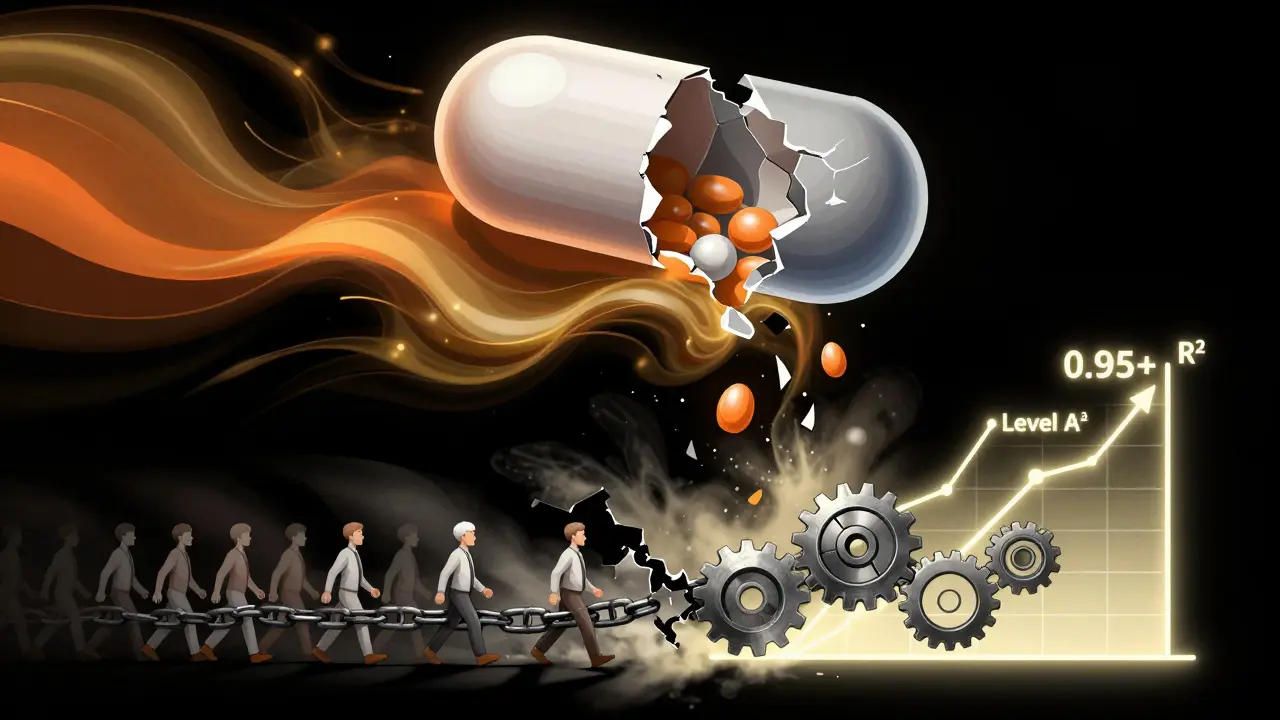
Not all correlations are created equal. The FDA classifies them into four levels, and only one really unlocks a full biowaiver:- Level A: The gold standard. Every point on the dissolution curve matches a point on the blood concentration curve. Think of it like a perfect mirror. If the pill dissolves 40% at 1 hour in the lab, the body absorbs exactly 40% at that same time. This gives you full predictive power. Acceptable models need R² > 0.95, slope near 1.0, and intercept near zero.
- Level B: Uses averages. It tells you the overall speed of release, but not the exact shape of the curve. Useful for some cases, but not enough for a waiver.
- Level C: One number to one number. For example, “dissolution at 1 hour predicts Cmax.” It’s easier to build, but risky. The EMA and FDA warn that this can miss real-world differences in absorption.
- Multiple Level C: Several dissolution points linked to multiple PK parameters. Better than single Level C, but still not as reliable as Level A.
For a regulatory waiver, you need Level A. The FDA requires predictions to be within ±10% for AUC (total exposure) and ±15% for Cmax (peak concentration). If you’re off by more, the model fails.
Why Most IVIVC Submissions Fail
You’d think with all the money at stake, companies would get it right. But here’s the truth: 64% of IVIVC submissions to the FDA in 2023 were rejected. Why?- Wrong dissolution conditions: Testing in plain water won’t cut it. Real stomach fluid has bile salts, enzymes, and pH shifts. Biorelevant media-like FaSSIF (fasted state simulated intestinal fluid)-is now mandatory for complex products. Companies using old compendial methods (USP Apparatus 2 in pH 1.2) are getting rejected.
- Not enough formulation variation: To build a model, you need at least 3-5 different versions of the drug: fast-releasing, slow-releasing, and everything in between. Most companies test only two formulations. That’s not enough to see the full pattern.
- Insufficient PK data: You need dense blood sampling-12+ time points per subject. Many studies sample every 2 hours, missing critical peaks and troughs.
- Validation done wrong: A model that fits your data doesn’t mean it predicts new data. True validation requires testing it on a completely new formulation, not just the ones you used to build it.
According to a 2022 survey of 47 generic manufacturers, 76% of failed IVIVC attempts were due to poor formulation characterization. That’s not a technical glitch-it’s a planning failure.
When IVIVC Works Best (and When It Doesn’t)
IVIVC isn’t a magic bullet. It shines in one area: modified-release oral products. Extended-release tablets, capsules, and pellets that release drug slowly over 8-24 hours are perfect candidates. That’s because their absorption is controlled by dissolution rate, not gut permeability.For immediate-release drugs, the Biopharmaceutics Classification System (BCS) is simpler. If the drug is highly soluble and highly permeable (BCS Class I), you can get a biowaiver just by showing dissolution in 15 minutes. No IVIVC needed.
But IVIVC fails in these cases:
- Narrow therapeutic index drugs: Warfarin, digoxin, lithium. Even tiny differences in absorption can be dangerous. Regulators still demand in vivo studies.
- Non-linear pharmacokinetics: When higher doses don’t lead to proportional blood levels, the math breaks down.
- Complex delivery systems: Ophthalmic gels, injectables, implants. These don’t dissolve the same way oral pills do. The FDA is exploring IVIVC for these, but no approvals yet.
- Food effects: If a drug absorbs differently when taken with food, your lab model must account for it. Many IVIVC models ignore this-and get caught when real patients eat breakfast.
Who’s Doing It Right?
The companies succeeding with IVIVC aren’t small players. Teva, Sandoz, Mylan, Sun Pharma, and Lupin have dedicated teams. They hire PhDs in pharmaceutics, not just formulation scientists. They partner with CROs like Alturas Analytics and Pion, who have success rates of 60-70% on Level A models-nearly double the industry average.One company spent $1.2 million over 18 months on a modified-release product, only to have their model collapse when real food-effect data came in. They scrapped it. Another spent 14 months and three formulation tries before the FDA accepted their oxycodone IVIVC. But once approved, they avoided five full bioequivalence studies. That’s a net savings of $8 million.
Smaller companies? Most give up. The expertise, time, and cost are too high. That’s why only 5 of the top 10 generic manufacturers have full IVIVC capabilities. The rest still rely on costly in vivo studies.
The Future: AI, Biorelevance, and Global Harmonization
The field is changing fast. In 2024, the FDA and EMA held a joint workshop on machine learning for IVIVC. Instead of linear regression, companies are now using neural networks to predict absorption from dissolution profiles. Early results show better accuracy, especially for complex release patterns.Biorelevant media is becoming standard. By 2025, the American Association of Pharmaceutical Scientists predicts 75% of new IVIVC submissions will use FaSSIF or FeSSIF (fed state media). The old “water and pH 6.8” tests are dead for anything beyond immediate-release.
The FDA’s GDUFA III plan (2023-2027) includes $15 million for IVIVC research. The EMA’s 2021 reflection paper shows 23% of scientific advice requests now involve IVIVC. This isn’t a trend-it’s a shift.
By 2027, McKinsey projects IVIVC-supported waivers will cover 35-40% of all modified-release generic approvals, up from 22% today. That’s a huge change. It means fewer volunteers in clinical trials, faster access to affordable drugs, and less waste.
What This Means for Patients and Providers
You won’t see IVIVC on a drug label. But you’ll feel its impact.Generic drugs are cheaper because companies aren’t spending millions on human studies. That savings gets passed on. More generics reach the market faster. Patients get access to life-saving medications sooner. For chronic conditions like hypertension or diabetes, that’s not just convenience-it’s health equity.
And for clinicians? Less uncertainty. When a generic has an approved IVIVC, regulators have already confirmed it behaves the same as the brand. No more guessing whether the cheaper version will work.
IVIVC isn’t perfect. It’s hard. It’s expensive to build. But when done right, it’s the most powerful tool we have to make generic drugs faster, safer, and more affordable.
What is the main advantage of using IVIVC over in vivo bioequivalence studies?
The main advantage is cost and time savings. A single in vivo bioequivalence study can cost $500,000 to $2 million and take 6-12 months. IVIVC allows companies to replace these studies with lab-based dissolution testing, cutting development time by 6-12 months and saving up to $2 million per study avoided. It also reduces the need to enroll healthy volunteers, making drug development more ethical and scalable.
Can IVIVC be used for all types of drugs?
No. IVIVC works best for modified-release oral products where drug absorption is controlled by dissolution rate-like extended-release tablets. It’s not suitable for drugs with narrow therapeutic indices (like warfarin), non-linear pharmacokinetics, or complex delivery systems like injectables or implants. For immediate-release drugs, the BCS classification system is simpler and more commonly used.
Why do most IVIVC submissions get rejected by the FDA?
Most rejections happen because the dissolution test doesn’t reflect real human physiology. Using plain water or simple pH buffers instead of biorelevant media like FaSSIF is the top reason. Other common failures include insufficient formulation variation, sparse blood sampling in pharmacokinetic studies, and poor model validation. The FDA requires models to predict new data-not just fit existing data.
What is the difference between Level A and Level C IVIVC?
Level A is a point-to-point correlation-every dissolution value matches a blood concentration value at the same time. It gives full predictive power and is required for full biowaivers. Level C only links one dissolution point (like % dissolved at 1 hour) to one pharmacokinetic parameter (like Cmax). It’s easier to build but less reliable, and regulators only accept it with strong supporting evidence.
Is biorelevant dissolution testing mandatory for IVIVC?
For complex modified-release products, yes. The FDA and EMA now expect dissolution testing to mimic real gastrointestinal conditions using biorelevant media like FaSSIF or FeSSIF. Traditional methods using water or simple buffers are no longer sufficient for regulatory approval. By 2025, biorelevant testing is expected to be standard for 75% of new IVIVC submissions.
Which companies are leading in IVIVC adoption?
The leaders are large generic manufacturers with dedicated R&D teams: Teva, Sandoz, Mylan, Sun Pharma, and Lupin. These companies invest in specialized staff, advanced dissolution equipment, and partnerships with CROs like Alturas Analytics and Pion. Smaller companies often lack the resources and expertise, so they still rely on traditional in vivo studies.
Final Thought: It’s Not About Replacing Humans-It’s About Replacing Unnecessary Testing
IVIVC doesn’t eliminate science. It makes it smarter. Instead of testing drugs on hundreds of people, we’re using better science to predict outcomes. The goal isn’t to cut corners-it’s to cut waste. When a drug’s behavior can be accurately predicted in a lab, why put people through blood draws? That’s not just efficient. It’s responsible.The future of generic drug approval isn’t more trials. It’s better models. And IVIVC is leading the way.






9 Comments
So... we're just replacing people with beakers now? I mean, I get it-less blood draws, less money, less waiting-but it still feels like we're trusting a machine to guess what our bodies do... like, what if the pill dissolves perfect in the lab but my stomach's just... weird? I've had drugs that work on my friend but make me feel like a zombie. Not all bodies are the same, you know? I'm not against progress, but... *sigh* I just hope they're not cutting corners under the guise of science.
This is actually one of the most thoughtful pieces I've read on generic drug regulation. The distinction between Level A and Level C IVIVC is crucial-and something I didn't realize was so finely tuned. It's impressive how much rigor is required just to get a waiver. The fact that 64% of submissions fail tells me the FDA isn't just rubber-stamping this. That’s reassuring. I wonder if this model could ever be applied to biologics? Maybe not yet, but the direction feels right.
My cousin takes metformin and just got a new generic. She didn't even notice a difference. Honestly? If the science says it's the same and the price is lower, I'm all for it. Less money for pharma, more money for groceries. Win-win.
OMG YES. This is the future. Imagine not having to drag yourself to a clinic for blood draws every two hours for weeks just to prove a pill works. We’re talking about real people here-students, parents, elderly folks-who just need their meds. This isn’t cold science-it’s compassion with data. Let’s fund this, scale this, and make it the norm. No more unnecessary suffering. Just... better science. I’m here for it.
Just to clarify: biorelevant media like FaSSIF isn’t optional anymore for anything beyond immediate-release. If you’re testing an extended-release tablet in plain water, you’re not just doing it wrong-you’re wasting everyone’s time. The FDA has been clear since 2018. And yes, you need at least three formulations-not two. One fast, one slow, one in between. And your PK sampling? 12+ time points, minimum. No exceptions. I’ve reviewed 47 submissions this year. 39 failed because they skipped the basics. It’s not the tech-it’s the hustle.
Thank you for this comprehensive and meticulously detailed exposition. The ethical implications of reducing human subject involvement through scientifically validated in vitro models are profound. It is both pragmatic and humane to replace resource-intensive in vivo studies with robust IVIVC frameworks, provided that the requisite statistical rigor and biorelevant conditions are strictly adhered to. The regulatory alignment between the FDA and EMA represents a significant stride toward global harmonization in pharmaceutical science.
Back home in Nigeria, we still get generics that cost half what they do here-but sometimes they don’t work the same. I wonder if this IVIVC thing will ever reach places like ours? Or will it just make the rich countries faster and leave the rest behind? I hope not. Medicine shouldn’t be a luxury of good labs.
It is important to note that the validation of IVIVC models must include prospective testing on formulations not used in model development. This is a critical distinction often overlooked. A model that fits historical data is not necessarily predictive. Regulatory acceptance requires independent verification. This standard ensures patient safety and scientific integrity. The industry must prioritize this step above expediency.
Wait wait wait-so if I’m on warfarin, I still gotta do the blood draws? Good. I don’t trust any algorithm to tell me if my blood’s gonna clot or not. I’ve seen what happens when things are ‘close enough.’ Not cool. This whole thing? Amazing for metformin. But for life-or-death meds? Let’s keep the humans in the loop. Just a little. Please.