
P2Y12 Inhibitor Decision Tool
| Drug | Efficacy Score | Bleeding Risk Score | Overall Recommendation |
|---|---|---|---|
| Prasugrel | |||
| Ticagrelor | |||
| Clopidogrel |
When doctors need to stop a blood clot after a heart attack or a stent placement, they turn to a class of drugs called P2Y12 inhibitors. Prasugrel vs alternatives is a hot topic because the right choice can mean fewer repeat heart attacks and fewer bleeding complications.
What is Prasugrel?
Prasugrel is a second‑generation thienopyridine that irreversibly blocks the P2Y12 platelet receptor. By preventing ADP‑mediated platelet aggregation, it reduces the risk of a new clot forming after an acute coronary syndrome (ACS) event. Prasugrel was approved in the U.S. in 2009 and has been incorporated into European and Australian guidelines for patients undergoing percutaneous coronary intervention (PCI).
How does Prasugrel differ from other P2Y12 inhibitors?
Three drugs dominate the P2Y12 market: Clopidogrel, Ticagrelor and Prasugrel. All three prevent platelets from sticking together, but they vary in how fast they work, how consistent the effect is, and how they are metabolized.
Mechanism of Action and Pharmacokinetics
- Prasugrel: A pro‑drug converted by CYP2C19 and CYP3A4 into an active metabolite that binds irreversibly to the P2Y12 receptor. Onset within 30 minutes, peak inhibition at 2 hours, half‑life of the active metabolite ~7 hours.
- Clopidogrel: Also a pro‑drug, but relies heavily on CYP2C19. Variable activation leads to a slower and less predictable platelet inhibition (onset 2-6 hours, peak 3-7 days).
- Ticagrelor: A direct‑acting reversible inhibitor, not a pro‑drug. Rapid onset (30 minutes), peak at 1.5 hours, half‑life ~12 hours.
Evidence from Major Trials
Three landmark studies shape current practice:
- TRITON‑TIMI 38 (Prasugrel vs Clopidogrel in 13,000 ACS patients). Prasugrel cut the composite of cardiovascular death, MI, or stroke by 16% but raised major bleeding by 32%.
- PLATO (Ticagrelor vs Clopidogrel in 18,000 ACS patients). Ticagrelor lowered the primary endpoint by 16% with a modest increase in non‑fatal bleeding, but not in fatal bleeding.
- CAPRICORN (head‑to‑head comparison of Prasugrel vs Ticagrelor). No statistically significant difference in efficacy, but prasugrel showed slightly higher bleeding in patients over 75 kg.
Safety Profile: Bleeding Risks
Bleeding is the main downside of potent P2Y12 inhibitors. The risk hierarchy, based on pooled data, looks like this:
- Highest: Prasugrel - especially in patients >75 years, weight <60 kg, or with a history of stroke/TIA.
- Intermediate: Ticagrelor - reversible binding means the effect wanes faster after discontinuation.
- Lowest: Clopidogrel - less potent, but also less effective at preventing ischemic events.
Clinicians often mitigate risk by using a lower maintenance dose (5 mg) for high‑risk patients or switching to clopidogrel after a short course of the newer agents.
Indications and Contra‑indications
All three drugs are approved for ACS and PCI, but nuances matter:
| Drug | Primary Indication | Major Contra‑indication |
|---|---|---|
| Prasugrel | ACS patients undergoing PCI | History of stroke/TIA, age >75 yr, weight <60 kg |
| Clopidogrel | ACS, stroke secondary prevention | Active pathological bleeding |
| Ticagrelor | ACS (including non‑ST‑elevation) and long‑term secondary prevention | History of intracranial hemorrhage, severe hepatic impairment |
Dosing Regimens
- Prasugrel: 60 mg loading, then 10 mg daily (5 mg if age > 75 yr or weight < 60 kg).
- Clopidogrel: 300-600 mg loading, then 75 mg daily.
- Ticagrelor: 180 mg loading, then 90 mg twice daily.
Because prasugrel and ticagrelor require higher pill burden, adherence can be an issue for some patients.
Cost Considerations in Australia (2025)
| Drug | Monthly Cost (AU$) | Generic Availability |
|---|---|---|
| Prasugrel | 180 | No (brand‑only) |
| Clopidogrel | 45 | Yes (multiple generics) |
| Ticagrelor | 220 | No (brand‑only) |
For patients without private insurance, clopidogrel is often the default purely for cost reasons, even when a more potent agent might be clinically preferable.
Guideline Recommendations (2024 ESC, 2025 Australian Cardiology Society)
- Prefer Prasugrel or Ticagrelor over Clopidogrel for all ACS patients undergoing PCI, unless contraindicated.
- Use Prasugrel for patients without prior stroke/TIA, age ≤75 yr, weight ≥60 kg, and who can tolerate a once‑daily pill.
- Choose Ticagrelor for patients who need rapid reversibility (e.g., potential need for urgent surgery) or who are at higher bleeding risk but still require potent platelet inhibition.
- Reserve Clopidogrel for patients with contraindications to the newer agents, high cost sensitivity, or for long‑term secondary prevention after the initial 12‑month intensive phase.
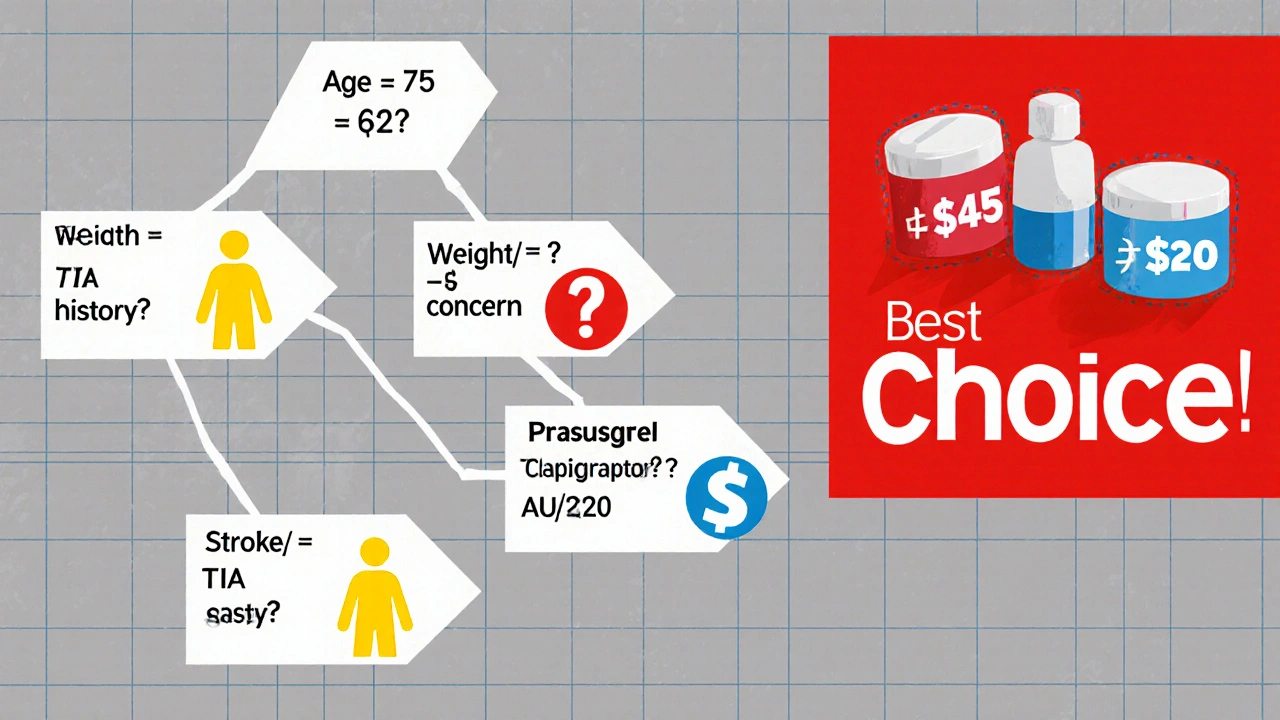
Practical Decision Tree
- Is the patient >75 yr or <60 kg?
Yes → Avoid Prasugrel; consider Ticagrelor or Clopidogrel. - History of stroke/TIA?
Yes → Avoid Prasugrel; Ticagrelor is acceptable if no intracranial bleed risk. - Need for rapid offset (e.g., upcoming surgery)?
Yes → Ticagrelor (reversible) preferred. - Cost‑conscious patient with good renal function?
Yes → Clopidogrel may be chosen, acknowledging lower efficacy. - Otherwise, high‑risk ACS with PCI → Prasugrel offers strongest evidence of outcome benefit.
Key Takeaways for Patients
- Discuss any history of bleeding, stroke, or low body weight with your cardiologist.
- Ask about the cost and whether your insurance covers the newer agents.
- If you’re scheduled for surgery, let your doctor know; a reversible drug like Ticagrelor may simplify timing.
Frequently Asked Questions
Can I switch from clopidogrel to prasugrel after a heart attack?
Yes, many clinicians start patients on clopidogrel and switch to prasugrel once the risk of early bleeding subsides, typically after 5-7 days, provided there are no contraindications.
Why does ticagrelor need to be taken twice daily?
Ticagrelor’s reversible binding means its platelet inhibition drops faster than irreversible agents. Twice‑daily dosing maintains a steady therapeutic level.
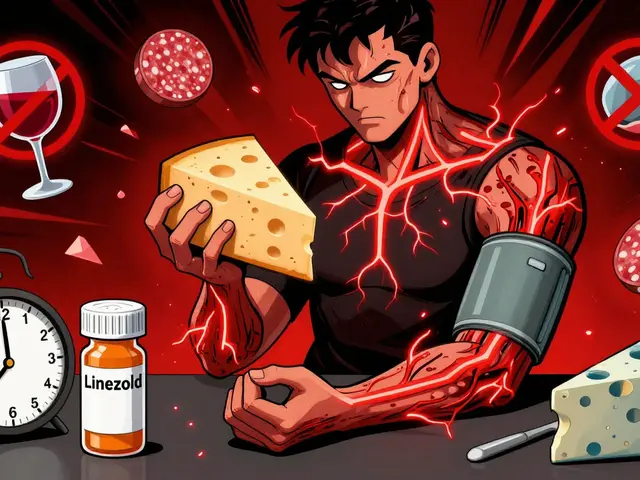
Is prasugrel safe for patients on aspirin?
Standard practice pairs any P2Y12 inhibitor with low‑dose aspirin (75‑100 mg). The combination improves efficacy but also raises bleeding risk, so monitoring is essential.
How long should I stay on prasugrel after stent placement?
Guidelines recommend at least 12 months of dual antiplatelet therapy (DAPT) after a drug‑eluting stent. Some patients continue beyond that period if they remain at high ischemic risk and low bleeding risk.
What lab test checks if prasugrel is working?
Platelet function tests such as VerifyNow P2Y12 assay can quantify inhibition. However, routine testing isn’t recommended unless there’s a clinical concern about drug resistance or bleeding.
Bottom Line
Prasugrel delivers the most robust protection against repeat heart attacks in younger, heavier patients without a prior stroke, but it carries a higher bleeding price tag. Ticagrelor offers similar efficacy with the benefit of reversibility, while clopidogrel remains a cost‑effective, lower‑risk option for those who can’t tolerate the newer drugs. The best choice hinges on age, weight, bleeding history, surgery plans, and, of course, the pocket.



9 Comments
Prasugrel works fast, but watch the bleeding risk in older patients.
The 2024 ESC guidelines really push Prasugrel and Ticagrelor front‑and‑center for ACS patients undergoing PCI. If a patient is under 75, weighs over 60 kg and has no prior stroke, Prasugrel is often the best pick. For those who might need quick reversal, Ticagrelor has the edge. Still, the cost gap is huge, especially in public hospitals.
Honestly, the whole "potent drug" hype feels like a cash‑grab. You’re paying over $180 a month for Prasugrel when a cheap generic does the job for most folks. And the bleeding risk? Nobody wants another hospital stay because of a prescription. So why not stick with clopidogrel unless you’re in a trial?
Let me set the stage: a bright, early morning in the cath lab, the hum of monitors, the scent of antiseptic – a symphony of life‑saving technology. The cardiologist, eyes narrowed like a hawk, reaches for the P2Y12 box, contemplating the ancient rivalry between Prasugrel, Clopidogrel, and the ever‑daring Ticagrelor. In his mind, the TRITON‑TIMI 38 trial looms like a mythic saga, promising reduced composite events at the cost of a bleeding dragon to be slain. He recalls the CAPRICORN head‑to‑head showdown, where the warriors clashed, yet no clear victor emerged, only whispers of higher bleeding in the heavier Prasugrel knight. Each drug, a character in this drama, carries its own backstory: Prasugrel, the swift assassin, irreversibly binding the P2Y12 receptor, delivering a half‑life of seven hours, but leaving a scar of 32 % more major bleeding. Clopidogrel, the old‑guard, slow to rise, its activation shackled by CYP2C19, sometimes stumbling in patients who are poor metabolizers. Ticagrelor, the rebellious non‑pro‑drug, reversible, dancing in and out of the receptor with a twelve‑hour half‑life, promising flexibility for urgent surgeries. The decision tree unfurls like a tangled vine: age, weight, prior stroke, cost – each node a fork in the road. The cardiologist ponders the Australian formulary, staring at AU$180 for Prasugrel, AU$45 for Clopidogrel, AU$220 for Ticagrelor – numbers that could devastate a patient’s wallet. He imagines the patient’s perspective: a monthly bill that rivals a mortgage, the anxiety of adhering to a twice‑daily regimen. He wonders about the future, the looming generic versions, the potential for cost‑parity, the promise of personalized medicine guided by genetic testing. In the end, the choice is not merely pharmacologic; it is a moral calculus, balancing efficacy, safety, economics, and patient autonomy. And as the cath lab lights flicker, the decision is made, a single prescription sliding across the sterile tray, sealing the fate of a heart that just survived the storm.
Prasugrel's pharmacodynamics are robust its irreversible binding ensures sustained inhibition but cost remains prohibitive
Oh great, another pricey drug to add to the list.
For most patients clopidogrel stays the budget‑friendly go‑to.
In Australia we see the same dilemma – the health system can’t afford all the brand‑only options so doctors often default to clopidogrel unless the patient meets strict criteria for a stronger agent. It’s a pragmatic approach, not a lack of care.
Thats not how u compare cost w/ generics. Clopidogrel may be cheap but it doesnt always work well for every body.