
More than 19% of U.S. adults experience an anxiety disorder each year. That’s one in five people you know-friends, coworkers, family members-who wake up with a knot in their stomach, avoid social events, or lie awake at night fearing something terrible is about to happen. Anxiety isn’t just stress. It’s a medical condition with real, measurable symptoms and proven treatments. Yet many suffer in silence, thinking they’re just "overreacting" or "too sensitive." The truth? Anxiety disorders are among the most common mental health conditions-and they’re highly treatable.
What Are the Main Types of Anxiety Disorders?
Anxiety isn’t one thing. It shows up in different forms, each with its own pattern of thoughts, feelings, and behaviors. The DSM-5, the standard guide used by clinicians, recognizes seven primary types:- Generalized Anxiety Disorder (GAD): Constant, excessive worry about everyday things-work, health, bills, even minor decisions. People with GAD often feel on edge, fatigued, and unable to relax, even when there’s no clear reason to be anxious. Symptoms last six months or longer.
- Panic Disorder: Sudden, intense episodes of fear that strike without warning. These panic attacks include racing heart, chest pain, shaking, dizziness, and the terrifying feeling that you’re dying or losing control. After one attack, people often live in fear of the next one.
- Social Anxiety Disorder: Extreme fear of being judged, embarrassed, or humiliated in social situations. This isn’t just shyness. It’s avoiding conversations, meetings, parties, or even eating in public because the fear feels unbearable.
- Specific Phobias: Intense fear of a specific object or situation-heights, spiders, flying, needles, or even vomiting. The fear is out of proportion to the actual danger, and people go to great lengths to avoid it.
- Separation Anxiety Disorder: Often thought of as a childhood issue, but it affects adults too. People with this disorder experience extreme distress when separated from loved ones, even if they’re safe and the separation is temporary.
- Obsessive-Compulsive Disorder (OCD): While now classified separately, OCD shares deep roots with anxiety. It involves intrusive, unwanted thoughts (obsessions) and repetitive behaviors (compulsions) performed to reduce the anxiety they cause-like checking locks 10 times or washing hands until they bleed.
- Selective Mutism: A condition mostly seen in children where they don’t speak in certain settings (like school) even though they speak normally at home. It’s not defiance-it’s anxiety so overwhelming that speaking feels impossible.
These aren’t just "bad days." Each has specific diagnostic criteria, and they often overlap. Someone might have GAD and social anxiety at the same time. That’s common-and treatable.
What Do Anxiety Symptoms Actually Look Like?
Anxiety doesn’t just live in your head. It shows up in your body, too. Here’s what real symptoms look like, backed by clinical data:- Physical: Heart rate spikes to 110-140 beats per minute during panic attacks. Sweating (reported by 92% of panic disorder patients), trembling (87%), shortness of breath (83%), dizziness (76%), nausea (68%), and muscle tension are all common.
- Cognitive: Racing thoughts (82%), difficulty concentrating (89% in GAD), catastrophic thinking ("I’m going to collapse," "Everyone thinks I’m weird"), and constant rumination (91% of people with anxiety replay worries over and over).
- Emotional: Feeling like something terrible is about to happen (95% during panic attacks), excessive worry that doesn’t match reality (100% in GAD), and fear of losing control or going crazy (88%).
These symptoms aren’t imagined. They’re biological. The brain’s threat detection system-usually meant to protect you from danger-is stuck in overdrive. That’s why breathing techniques, grounding exercises, and therapy work: they help reset that system.
What Treatments Actually Work?
The good news? We know what helps. Not guesswork. Not trends. Science-backed, tested, and proven methods.Cognitive Behavioral Therapy (CBT)
CBT is the gold standard. It’s not talking about your childhood. It’s learning practical skills to change how you think and act. A typical CBT program lasts 12 to 20 weekly sessions. By session 12, 60-80% of people report major improvements.Key components:
- Cognitive restructuring: Learning to spot distorted thoughts ("I’ll fail and everyone will laugh") and replacing them with realistic ones ("I’ve prepared. I can handle this.").
- Exposure therapy: Gradually facing feared situations-starting small. For social anxiety, that might mean saying hello to a coworker. For panic disorder, it could mean intentionally letting your heart race in a safe setting. This isn’t about "getting over it." It’s about teaching your brain that the feared outcome won’t happen.
Studies show exposure therapy works for 60-80% of people with phobias and social anxiety. It’s hard. You’ll want to quit. But that’s the point-the discomfort is temporary, and the freedom it brings lasts.
Medication: SSRIs and SNRIs
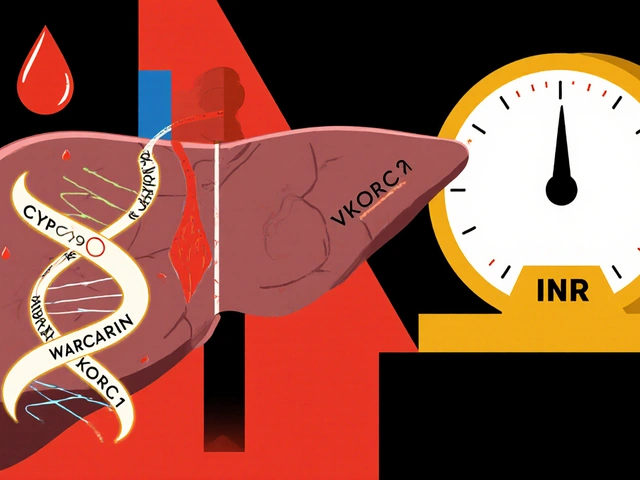
When therapy alone isn’t enough-or when symptoms are severe-medication helps. First-line choices are SSRIs (selective serotonin reuptake inhibitors) like sertraline (Zoloft) and fluoxetine (Prozac), and SNRIs like venlafaxine (Effexor).They don’t work overnight. It takes 6-12 weeks to see full effects. But for many, they reduce physical symptoms-racing heart, sweating, nausea-making therapy easier to stick with.
They’re not addictive. Unlike benzodiazepines (like Xanax or Valium), which offer quick relief but carry high risks of dependence and brain fog with long-term use, SSRIs are safe for months or years. The American Psychiatric Association recommends them as first-line because of their proven safety profile.
Other Effective Options
- Acceptance and Commitment Therapy (ACT): Focuses on accepting anxious thoughts without fighting them, while committing to actions that align with your values. Just as effective as CBT for many.
- Digital tools: FDA-cleared apps like nOCD and Wysa offer guided CBT exercises. Studies show 35-45% symptom reduction in 8 weeks with daily use.
- Newer medications: Zuranolone (Zurzuvae), approved in 2023, is the first oral drug specifically for postpartum anxiety, with a 54% remission rate in trials.
What Gets in the Way of Treatment?
Knowing what works isn’t enough. Many people don’t get help-and here’s why:- Wait times: Average 6-8 weeks to see a specialist. Some rural areas have none.
- Cost and insurance: Many plans limit therapy sessions or require high copays. Medication co-pays can be steep without good coverage.
- Symptom severity: The very symptoms that need treatment-fatigue, avoidance, panic-make it hard to pick up the phone or show up to an appointment.
- Side effects: Some people feel emotionally numb on SSRIs. Others get nausea or insomnia. Adjusting doses or switching meds takes time and patience.
Real stories from Reddit and support groups reflect this struggle: "CBT helped, but exposure made me want to quit." "SSRIs helped my body, but I felt like a zombie." These aren’t failures-they’re part of the process.
What’s New in 2025?
Treatment isn’t standing still. Here’s what’s changing:- Precision medicine: Brain scans (fMRI) are now identifying three distinct "anxiety biotypes" that predict who responds best to CBT vs. medication. This could end the trial-and-error cycle.
- AI-powered prediction: Stanford researchers developed an algorithm that predicts panic attacks 24 hours in advance with 87% accuracy-using voice patterns, movement, and sleep data.
- Ketamine therapy: Early trials show rapid relief for treatment-resistant anxiety. While still experimental, it’s being studied in clinics nationwide.
- Genetic testing: By 2027, experts predict genetic markers will guide medication choices with 70% accuracy, reducing side effects and speeding up recovery.
These aren’t sci-fi. They’re happening now. And they’re making treatment faster, more personal, and more effective.

Where to Start
If you or someone you care about is struggling:- See your primary care doctor. They can rule out medical causes (like thyroid issues) and refer you to a mental health specialist.
- Ask about CBT. Not just "therapy." Specifically ask if they use evidence-based CBT or exposure therapy.
- Try a digital tool like nOCD or Wysa while waiting for an appointment. They’re free or low-cost and proven to help.
- Don’t give up on medication if the first one doesn’t work. It often takes 2-3 tries to find the right fit.
- Join a support group. The Anxiety and Depression Association of America (ADAA) offers 300+ weekly groups. NAMI’s 24/7 helpline answers over 25,000 calls a month.
Anxiety doesn’t have to be your life sentence. It’s a condition-not a character flaw. With the right tools, people recover. They go back to work. They reconnect with family. They travel. They speak up. They live.
You don’t have to wait until you’re "broken" to get help. You don’t have to suffer in silence. Help is here. And it works.
Can anxiety disorders go away on their own?
Sometimes symptoms lessen over time, but they rarely disappear completely without treatment. Left untreated, anxiety often worsens or leads to other problems like depression, substance use, or chronic physical health issues. Early intervention gives you the best chance at full recovery.
Is CBT better than medication for anxiety?
Neither is universally "better." CBT teaches lasting skills and has no side effects, but it takes effort and time. Medication can reduce symptoms quickly, making therapy easier to engage with. Research shows the best results come from combining both-especially for moderate to severe cases. About 58% of people report improvement with combined treatment, compared to 42% with medication alone and 38% with therapy alone.
How long does it take for SSRIs to work?
Most people start noticing small improvements in 2-4 weeks, but full effects usually take 6-12 weeks. It’s common to feel worse before you feel better-especially in the first few weeks. Don’t stop taking it unless your doctor advises. If side effects are unbearable, talk to your provider about adjusting the dose or switching meds.
Can children have anxiety disorders?
Yes. Half of all anxiety disorders begin by age 11. Children may show it as tantrums, refusal to go to school, clinginess, or physical complaints like stomachaches. Early treatment is critical-CBT adapted for kids is highly effective, and it prevents long-term struggles into adulthood.
Are anxiety disorders genetic?
Genetics play a role. If a close family member has an anxiety disorder, your risk is higher-but it’s not destiny. Environment, trauma, stress, and life experiences also shape whether someone develops anxiety. Even with a genetic predisposition, early intervention and healthy coping skills can prevent it from taking hold.
What if I can’t afford therapy?
Many community health centers offer sliding-scale fees based on income. Online platforms like Open Path Collective connect people with therapists charging $30-60 per session. Free or low-cost CBT apps like Woebot and nOCD are clinically validated. Support groups through NAMI and ADAA are free and available nationwide. Help is accessible-even if money is tight.
Can I manage anxiety without medication or therapy?
Mild anxiety can sometimes be managed with lifestyle changes-regular exercise, sleep hygiene, reducing caffeine, and mindfulness. But for moderate to severe anxiety, these alone aren’t enough. Therapy and medication are the only treatments proven to significantly reduce symptoms and restore function. Trying to "power through" without help often leads to burnout and worsening symptoms.
What Comes Next?
Recovery isn’t linear. Some days will be harder than others. That’s normal. The goal isn’t to never feel anxious-it’s to stop letting anxiety control your life. You’ll learn to recognize the early signs. You’ll use your tools. You’ll reach out. You’ll keep going.There’s no shame in needing help. There’s only strength in asking for it. And you’re not alone. Millions are walking this path-and many have already found their way through.







8 Comments
Let me break this down for you. CBT isn't magic-it's behavioral conditioning. You're literally rewiring your amygdala through repeated exposure. The stats are solid, but most people quit at week 3 because they think it's not working. It's not supposed to feel good. It's supposed to make you uncomfortable so your brain learns the threat isn't real. And no, breathing exercises won't fix a chemical imbalance. Stop treating anxiety like a vibe you can meditate away.
I've been on sertraline for 14 months. The first six weeks felt like my emotions were wrapped in plastic. But slowly, the panic attacks stopped hitting like freight trains. What helped most was realizing I didn't have to fight the thoughts-just let them pass like clouds. Therapy gave me tools. Medication gave me the bandwidth to use them. Neither alone was enough. Together? Life changed.
Yo I just wanna say-this post is fire. I was a mess last year, avoided my own family dinners, thought I was losing my mind. Started using nOCD daily. Did one tiny exposure: said hi to my barista. Felt like I was walking through lava. But I did it again. And again. Now I ask for extra sauce without sweating bullets. It's not about being brave. It's about showing up when your brain screams 'RUN'. You're not broken. You're just wired differently. And that's okay.
Of course the pharmaceutical industry loves SSRIs. They make billions. Meanwhile, the real cure is sunlight, magnesium, and quitting social media. They don't want you to know that because it's free. And don't get me started on 'exposure therapy'-sounds like psychological torture wrapped in jargon. They're just trying to make you compliant. Your anxiety? It's not a disorder. It's your soul screaming for authenticity.
Did you know the DSM-5 was written by a committee funded by Big Pharma? The whole 'anxiety disorder' framework is a construct to pathologize normal human emotion. The real cause? Surveillance capitalism. Your anxiety isn't in your brain-it's in the algorithm. They're feeding you fear 24/7 through ads, news, and notifications. They want you dependent. On meds. On apps. On therapists. Wake up. The system is rigged. The panic attacks? They're your body's last protest.
Back home in Afghanistan, we didn’t have CBT or SSRIs. We had tea, silence, and the quiet understanding that pain doesn’t need a label. My uncle had panic attacks after the bombing-he’d sit under the pomegranate tree for hours, not speaking. No diagnosis. No pills. Just presence. Maybe we’re overcomplicating this. Not every wound needs surgery. Sometimes it just needs someone to sit with you in the dark.
Exposure therapy? How quaint. Did you know the American Psychiatric Association is a front for the American Medical Industrial Complex? SSRIs are merely chemical sedatives disguised as solutions. The real cure? Fasting. Cold exposure. And yes-unplugging from the Matrix. Your body is not broken. Your environment is. And they don't want you to know that. Because then you'd stop buying their pills. And their therapy sessions. And their apps. And their conferences. And their journals. And their...
...wait. Did I just spend $180 on a CBT workbook?
CBT works. SSRIs work. But only if you're middle class, insured, and have 20 hours a week to spare. What about the single mom working two jobs? The veteran with no VA access? The kid in rural Mississippi with one therapist for 500 miles? This post reads like a luxury brochure. Real treatment? It's a lottery. And most of us lost before we even bought a ticket.