Drug Interaction Checker
Note: This tool is for educational purposes only. Always consult with your doctor or pharmacist for medical advice.
Every year, tens of thousands of people end up in the hospital because of drug interactions-some preventable, many never checked. You might be taking a statin for cholesterol, a blood thinner for heart health, or an antidepressant for mood, but if you add a new pill without checking what it does with what you’re already on, you could be risking serious harm. It’s not about being paranoid. It’s about being smart.
Why Drug Interactions Are More Dangerous Than You Think
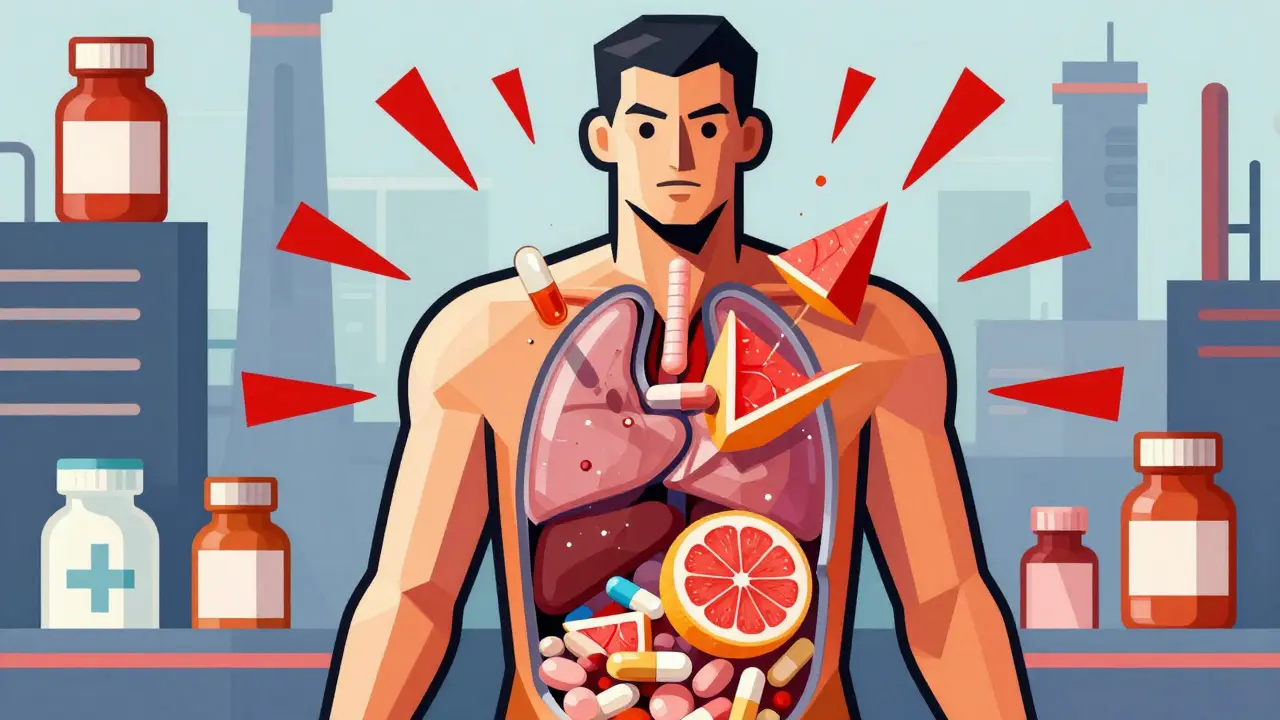
Drug interactions happen when two or more substances-medications, supplements, even foods-change how your body handles a drug. This can make a medicine too strong, too weak, or cause side effects you didn’t sign up for. Grapefruit juice, for example, can make cholesterol-lowering statins like simvastatin dangerously potent. One study found that combining simvastatin over 20 mg with the heart rhythm drug amiodarone increases the risk of muscle breakdown (rhabdomyolysis) by 15 times. That can lead to kidney failure or death. The FDA says about 7,000 deaths each year in the U.S. come from preventable drug reactions. Half of those are caused by interactions that could have been caught with a simple check. And it’s not just prescription drugs. Over-the-counter painkillers like ibuprofen can thin your blood too much if you’re already on warfarin. Herbal supplements like St. John’s Wort can make antidepressants less effective-or trigger serotonin syndrome, a life-threatening condition.The Four Questions You Must Ask Before Taking Anything New
Don’t assume your doctor or pharmacist knows everything you’re taking. Many patients see multiple providers, use different pharmacies, and forget to mention supplements. Before you start any new medication, ask these four questions out loud:- Can I take this with my other medications?
- Should I avoid certain foods, drinks, or alcohol?
- What are the warning signs of a bad reaction I should watch for?
- How will this drug work in my body, and what might interfere with it?
Build and Maintain a Complete Medication List
The most powerful tool you have is a real, up-to-date list of everything you take. Not just prescriptions. Include:- All prescription drugs (name, dose, frequency)
- All over-the-counter meds (pain relievers, antacids, sleep aids)
- All vitamins, minerals, and supplements (even if you think they’re harmless)
- Herbal products (turmeric, ginkgo, echinacea, etc.)
- Any topical creams or patches

Use Free Online Checkers-But Don’t Rely on Them Alone
There are good, free tools out there. The Drugs.com Drug Interactions Checker is one of the most trusted. It checks over 24,000 prescription drugs, 7,000 supplements, and 4,000 foods. It’s updated daily and used by over a million people monthly. In a 2021 study, it caught 92.4% of clinically significant interactions-better than WebMD’s tool. The University of Liverpool’s HIV Drug Interaction Checker is even more precise, especially for complex regimens. It uses a color-coded system: red = dangerous, yellow = use caution, green = safe. It’s so reliable that 78% of HIV specialists use it. But here’s the catch: no online tool knows your body. It doesn’t know if you have kidney disease, are over 65, or have a genetic variation that slows how you process drugs. The FDA warns these tools can’t replace professional advice. They’re helpers-not replacements.Know the Top 7 High-Risk Drug Combinations
Some interactions are so dangerous they’re well-documented. These seven combinations account for 63% of serious hospitalizations from drug interactions:- Warfarin + NSAIDs (like ibuprofen or naproxen) → bleeding risk
- SSRIs (like sertraline) + MAOIs (like phenelzine) → serotonin syndrome
- Digoxin + clarithromycin → heart rhythm problems
- Statins + fibrates (like fenofibrate) → muscle damage
- Calcium channel blockers + protease inhibitors → dangerously low blood pressure
- Sildenafil (Viagra) + nitrates (like nitroglycerin) → sudden drop in blood pressure
- Theophylline + fluvoxamine → toxic levels of theophylline
Use One Pharmacy. Always.
This is one of the simplest, most effective steps you can take. Using a single pharmacy means all your meds are in one system. That pharmacy’s software can scan every new prescription against everything else you take. A 2021 study of 22,000 Medicare patients found that using just one pharmacy reduced serious drug interactions by 31%. Yet only 38% of Americans do it. Why? Cost. Convenience. Insurance restrictions. But here’s the truth: saving $5 on a prescription isn’t worth risking a hospital stay. If your insurance lets you switch, do it. If you’re paying cash, find a local pharmacy that offers low-cost generics. Your safety is worth more than a few dollars.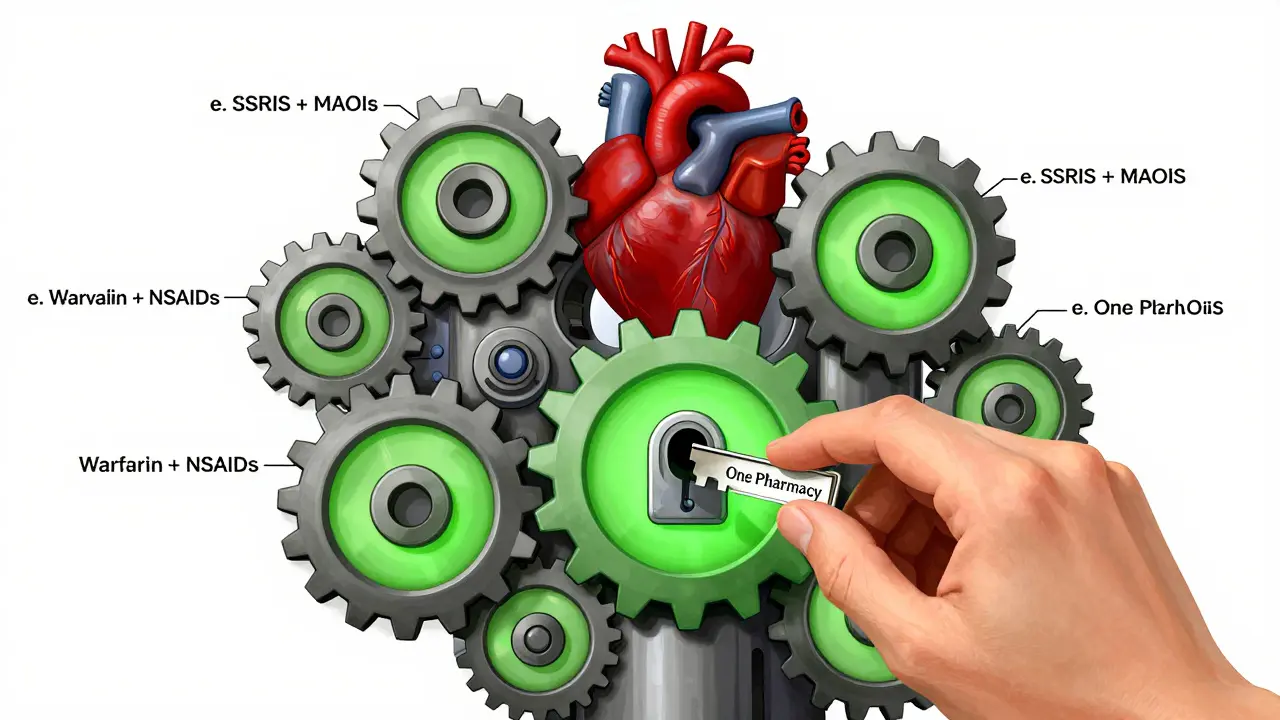
Don’t Ignore the ‘Alert Fatigue’ Problem
Doctors and pharmacists get flooded with interaction warnings. Some are real. Many are false alarms. One Reddit user reported 12 alerts for a five-medication regimen-most were trivial. That’s called alert fatigue. When warnings never stop, people start ignoring them. That’s dangerous. In one case, a patient missed a critical interaction between sertraline and linezolid (an antibiotic) because their doctor had seen so many false alerts they skimmed past the real one. The patient caught it themselves using Drugs.com and called their pharmacist before taking the antibiotic. The fix? Don’t let technology make you lazy. If you see a warning-even if you’ve seen it before-stop. Ask. Verify.What’s Next? Personalized Medicine Is Coming
The future of drug safety is personal. Researchers are now testing systems that use your genetic data to predict how you’ll react to drugs. The NIH found that adding CYP450 enzyme gene test results improved interaction prediction accuracy by 37% for 22 common medications. By 2024, all certified electronic health record systems in the U.S. will be required to show interaction alerts with severity ratings and patient-specific risk factors. That means your doctor’s system will soon say: “This combination is high risk for patients over 70 with reduced kidney function.” But until then, you’re still your own best safety net.Final Checklist: Your Action Plan
Here’s what to do today:- Write down every medication, supplement, and OTC drug you take-right now.
- Bring the actual bottles to your next doctor’s visit.
- Ask your doctor: “Can this interact with anything else I’m taking?”
- Use Drugs.com or the University of Liverpool’s checker to verify before starting anything new.
- Choose one pharmacy and stick with it.
- Read the label. Even if you’ve taken it before-doses change.
- Tell every provider-even the dentist or physical therapist-what you’re on.
Can I check for drug interactions myself without a doctor?
Yes, you can use free tools like Drugs.com or the University of Liverpool’s HIV Drug Interaction Checker to screen for potential interactions. These tools are reliable for spotting major risks. But they can’t replace professional advice. Your doctor or pharmacist knows your full health history-like kidney function, age, genetics, and other conditions-that these tools don’t. Always confirm findings with a healthcare provider before making changes.
Are herbal supplements safe to take with prescription drugs?
No, not necessarily. Many people assume herbal supplements are harmless because they’re “natural,” but that’s false. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and blood thinners. Garlic and ginkgo can increase bleeding risk when taken with warfarin. Turmeric can interfere with blood sugar medications. Always disclose every supplement you take-no matter how small or common it seems.
Why do I get so many drug interaction alerts from my pharmacy?
Pharmacy systems are programmed to flag even low-risk interactions to avoid liability. Many alerts are false positives-like warning about grapefruit juice with a drug that doesn’t interact with it. This causes “alert fatigue,” where people start ignoring all warnings. That’s dangerous. Always review alerts carefully. If something seems wrong or excessive, ask your pharmacist to explain why it’s flagged. Don’t dismiss it just because you’ve seen it before.
What should I do if I accidentally take a drug that interacts with another?
Stop taking the new medication immediately. Call your pharmacist or doctor. If you experience symptoms like dizziness, rapid heartbeat, confusion, muscle pain, bleeding, or trouble breathing, go to the emergency room. Don’t wait. Some interactions, like serotonin syndrome or rhabdomyolysis, can escalate quickly. Keep a list of all your meds handy to show medical staff.
Do drug interactions happen immediately after taking a new medication?
Sometimes, yes. For example, combining certain antibiotics with statins can cause muscle damage within 24-48 hours. Other interactions build up over days or weeks. Some, like grapefruit juice with statins, can have effects even if taken hours apart. That’s why it’s critical to check interactions before you start any new medication-not after you’ve already taken it.
Can I trust my pharmacist to catch all interactions?
Pharmacists are trained to catch interactions, and most use software that scans your full profile. But if you use multiple pharmacies, your records aren’t complete. A 2021 study found that 62% of interaction errors happened when patients used more than one pharmacy. Even with perfect software, if your doctor prescribed something new and your pharmacist doesn’t know about it, they can’t warn you. That’s why you need to keep your own list and bring it to every appointment.
Is it safe to skip a dose if I’m worried about an interaction?
No. Skipping doses without medical advice can be just as dangerous as taking a bad combination. For example, stopping blood thinners suddenly can cause clots. Stopping antidepressants abruptly can trigger withdrawal symptoms. If you’re worried about an interaction, contact your doctor or pharmacist before making any changes. Never adjust your meds on your own.
What’s the best way to keep my medication list updated?
Use a digital app like Medisafe or MyTherapy, or keep a simple printed list in your wallet. Update it every time you get a new prescription, stop a medication, or start a supplement. Bring it to every appointment-even if you think nothing changed. Many patients forget they started a new vitamin or painkiller. A “medication passport” updated after every visit reduces errors by over 50%, according to the Cleveland Clinic.








15 Comments
My pharmacist flagged my ibuprofen and warfarin combo. I ignored it. Two weeks later, I was in the ER with a hematoma the size of a grapefruit. Don't be me.
I used to think supplements were harmless ‘natural’ stuff. Then my mom went into serotonin syndrome after mixing St. John’s Wort with her SSRI. She’s fine now, but it took three days in ICU. Always ask. Always check. It’s not paranoia-it’s love.
Drugs.com is my bible. I plug in every new pill-even over-the-counter ones-before I swallow. I’ve caught three bad combos already. One was a melatonin that interacted with my blood pressure med. My pharmacist said I saved myself a trip to the hospital. Worth five minutes of my time.
Look, I’m from India, where we treat pharmacies like convenience stores. You walk in, say ‘I need something for pain,’ and they hand you a box of NSAIDs without asking if you’re on warfarin. I once saw a man take diclofenac with rivaroxaban-he didn’t even know what either drug did. It’s not just Western medicine that’s broken. It’s the culture of ‘just take it.’ If you’re on anything that affects your liver or kidneys, you owe it to yourself to know what’s in your body. Not just what the label says, but what it *does*. And yes, that means Googling. And yes, that means calling your pharmacist at 8 PM. You’re not being dramatic. You’re being alive.
They say ‘use one pharmacy’ like it’s a magic bullet. But have you seen the data? Big Pharma owns the pharmacy software. Those ‘interaction alerts’? Half of them are designed to scare you into buying their branded versions. I’ve had the same script flagged for ‘interaction’ with grapefruit juice for three years-when my med doesn’t even metabolize that way. They want you dependent. Don’t trust the system. Trust your own research. And always, always check the FDA’s MedWatch database.
PLEASE PLEASE PLEASE bring your actual bottles to your doctor!!! I thought I knew what I was taking-until I opened my cabinet and found three different versions of the same pill with different dosages!!! My doctor nearly fainted!!! I thought I was being careful!!! Turns out I was just confused!!!
Let us not pretend this is about patient safety. This is about liability avoidance disguised as public health. The FDA’s 7,000 death statistic is cherry-picked from a dataset that includes unreported suicides and accidental overdoses. The real issue? The pharmaceutical-industrial complex has created a dependency economy where patients are incentivized to take more pills, not fewer. The ‘four questions’ are performative. The real solution is de-prescribing. But that doesn’t sell profit margins.
I’ve been using the University of Liverpool’s tool for years-especially since I started my HIV regimen. It’s the only one that actually explains *why* something is dangerous, not just that it is. I print the results and bring them to my appointments. My doctor now says I’m his most prepared patient. It’s not hard. It’s just consistent.
Just started a new vitamin D3 and didn’t check. My blood sugar went nuts. I didn’t even know it could do that. I’m so sorry I didn’t read the whole article before. I’m updating my list tonight. Thank you for this. I’m gonna print it and tape it to my fridge. 💪
My grandma takes 17 pills a day. I made her a color-coded chart with pictures. She calls it her ‘medication rainbow.’ Now she knows what’s blue (heart), what’s red (blood thinner), and what’s green (vitamins). We even added little smiley faces for ‘safe with food.’ She laughs about it. But she’s alive. And she’s not in the hospital. Sometimes, simple wins.
Of course you’re supposed to check interactions-but who’s really doing it? The rich? The educated? Meanwhile, my cousin in rural Alabama gets her meds from Walmart’s $4 list and takes them with grapefruit juice because ‘it’s cheaper than water.’ They don’t have time to Google. They don’t have access to one pharmacy. And you’re telling them to ‘be smart’? That’s not advice-that’s classism dressed up as healthcare.
It is imperative to underscore that the utilization of standardized, evidence-based interaction-checking protocols remains an indispensable component of pharmacovigilance. The data presented herein, while compelling, necessitates corroboration via peer-reviewed literature and institutional guidelines, particularly those promulgated by the American College of Clinical Pharmacy. One must not conflate accessibility with efficacy.
Why are we even talking about this? In America, you take what the doctor gives you. Period. If you’re too lazy to read the label, that’s your problem. Stop blaming the system. Take responsibility.
They say ‘use one pharmacy’ like it’s a miracle. But what if your pharmacy’s system is outdated? What if they’re using software from 2015? What if they’re understaffed and miss things? I’ve had meds filled at the same place for 10 years-and still got a dangerous interaction. You can’t outsource your safety to a computer. You have to be the gatekeeper. Always.
You know who’s really responsible for these deaths? The doctors who prescribe without asking about supplements. The pharmacists who don’t follow up. The FDA that lets companies market drugs without full interaction testing. And you? You’re just the victim. Don’t feel guilty for not being a medical expert. Demand better systems. Because no amount of ‘checking’ should be required to stay alive.