
When someone is having a severe allergic reaction, every second counts. Anaphylaxis can turn a mild itch into a life-threatening emergency in under five minutes. If you or someone you care about has a history of serious allergies, knowing how to use an epinephrine auto-injector isn’t just helpful-it’s essential. This guide breaks down exactly how to use it, what to expect, and what most people get wrong-so you’re ready when it matters.
What Is an Epinephrine Auto-Injector?
An epinephrine auto-injector is a small, pen-like device that delivers a single, pre-measured dose of epinephrine (also called adrenaline) into the muscle. It’s designed for emergency use during anaphylaxis-a sudden, dangerous allergic reaction that can cause trouble breathing, a drop in blood pressure, swelling of the throat, or loss of consciousness.
Epinephrine works fast. It tightens blood vessels to raise blood pressure, opens airways to help breathing, and reduces swelling. Without it, anaphylaxis can be fatal. The American Academy of Allergy, Asthma & Immunology says giving epinephrine within 5 to 15 minutes of symptoms starting cuts the risk of death by 75%.
The most common brands are EpiPen, Auvi-Q, Adrenaclick, and the newer Neffy nasal spray. EpiPen is the most widely used, making up over 85% of the U.S. market. But each has differences in how they work, cost, and ease of use. For example, Auvi-Q gives voice instructions, which helps when you’re panicking. Neffy doesn’t use a needle, which matters to people afraid of injections.
When Should You Use It?
You don’t wait for symptoms to get worse. Use the auto-injector at the first sign of a severe reaction. That includes:
- Hives, swelling of the lips, tongue, or throat
- Wheezing, shortness of breath, or feeling like your airway is closing
- Dizziness, fainting, or sudden weakness
- Rapid heartbeat, nausea, vomiting, or a sense of doom
Some people think antihistamines like Benadryl are enough. They’re not. Delaying epinephrine to give an antihistamine first increases the chance of a second, even more dangerous reaction by 300%. Epinephrine is the only treatment that can stop anaphylaxis from killing someone.
Even if symptoms seem mild at first, don’t wait. Reactions can spike quickly. If you’re unsure, use it. Better safe than sorry.
How to Use an Epinephrine Auto-Injector (Step by Step)
Here’s how to use a standard auto-injector like the EpiPen. Other brands work similarly, but check the instructions that come with your device.
- Remove the safety cap. Most auto-injectors have a blue safety cap on the end. Pull it straight off. Don’t squeeze the sides or press the tip-this could trigger it accidentally.
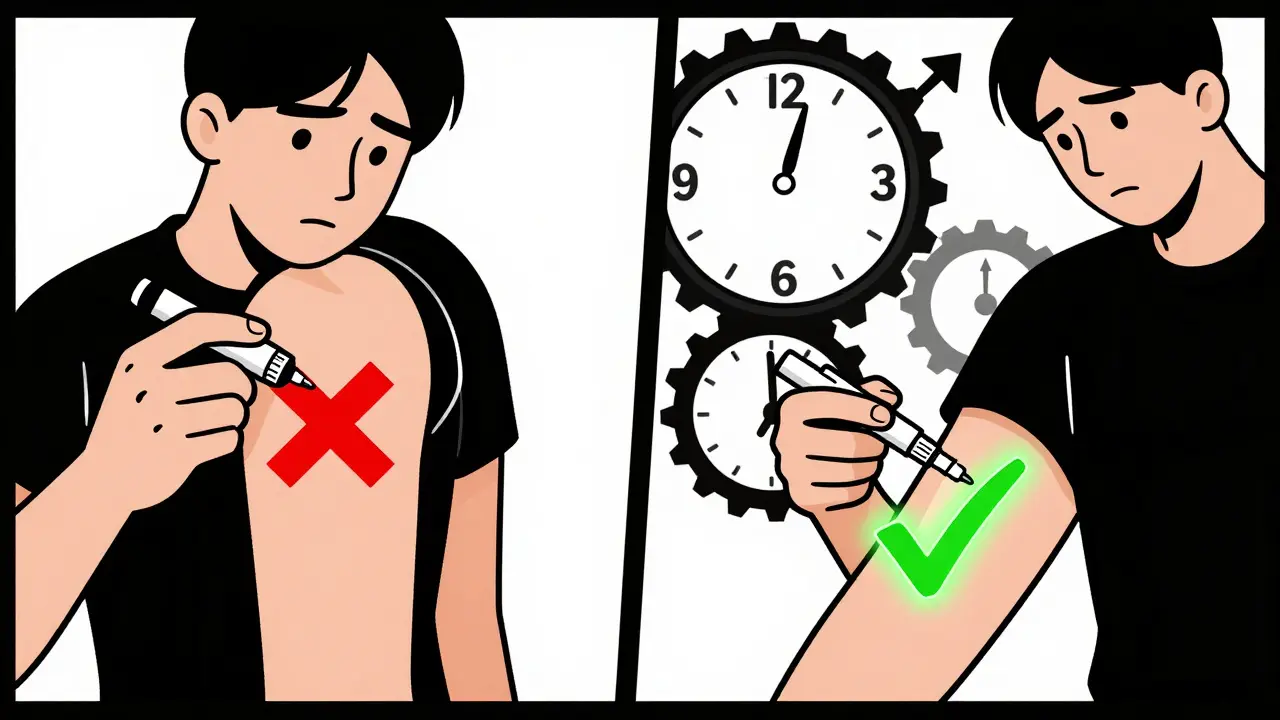
- Place it against the outer thigh. You can inject through clothing if needed. The best spot is the middle of the outer thigh, halfway between the hip and knee. Don’t inject into the buttocks, arms, or abdomen.
- Push hard until you hear a click. Press the injector firmly against the thigh until you hear a click. That means the needle has fired. Hold it there for 3 full seconds. Don’t pull away early.
- Remove the device. After 3 seconds, pull it straight out. You’ll see the needle retract automatically in most models.
- Massage the area for 10 seconds. Gently rub the injection site to help the medicine absorb faster.
- Call 911 or get emergency help immediately. Even if you feel better, you still need to go to the hospital. Anaphylaxis can come back hours later.
For children, hold their leg steady while injecting. If they’re small, you can place them on the floor or a table and inject from above. Never let them stand or walk during the reaction.
Common Mistakes People Make
Studies show only about 42% of people use the auto-injector correctly during a real emergency. Here are the biggest errors:
- Not holding it long enough. Most people pull it away after 1 or 2 seconds. You need 3 full seconds for the full dose to deliver.
- Missing the thigh. Injecting into the arm, belly, or buttocks means the medicine won’t absorb fast enough.
- Forgetting to call 911. Epinephrine buys time, but it’s not a cure. Hospital care is still needed.
- Delaying use. Waiting to see if symptoms get worse is the most dangerous mistake. Don’t wait.
- Accidental activation. The orange tip on EpiPens can trigger if squeezed too hard. Always keep it in its case and avoid touching the tip.
One study found that 37% of people using EpiPens for the first time made at least one critical error. That’s why practice matters.
Practice with a Trainer Device
Most pharmacies give you a trainer device that looks and feels like the real one-but doesn’t have a needle or medicine. Use it every few months. Practice on a pillow, a friend’s thigh, or even a banana.
Studies show you need about 3 to 4 practice sessions to get it right. Schools, workplaces, and even some pharmacies offer free training. Ask for it. If you’re a parent, make sure babysitters, teachers, and coaches know how to use it too.
Auvi-Q’s voice guidance helped 89% of users get it right in tests. If you’re nervous about remembering steps, it’s worth considering.
Storage and Expiration
Epinephrine breaks down over time. Check the expiration date every time you get a refill. Most devices last 12 to 18 months.
Store them at room temperature-between 59°F and 86°F. Don’t leave them in a hot car, a freezing glove compartment, or a bathroom where humidity can ruin them. Keep them in their original case to protect from light.
If the liquid inside looks cloudy, discolored, or has particles, replace it. Even if it hasn’t expired, a damaged device won’t work.
What About the New Nasal Spray?
Neffy, approved in 2023, is the first needle-free option. It’s a spray you put into one nostril. It works fast and avoids the fear of needles.
But it’s not perfect. In testing, 32% of people didn’t use it correctly during simulated emergencies. You need to press the nozzle firmly and breathe normally while spraying. It won’t work if you’re sneezing, sniffling, or holding your nose.
Neffy is a good option for needle-averse people, but it’s not yet as widely available as EpiPen. It also costs more and isn’t covered by all insurance plans.

Cost and Accessibility
Cost is a big barrier. EpiPen costs around $679 without insurance. Adrenaclick is cheaper at $195 but requires two steps to activate. Auvi-Q is over $4,200 but offers financial help for most users.
Many insurance plans cover auto-injectors, but copays can still be over $300. GoodRx coupons can help. Some manufacturers offer free or low-cost programs for people without insurance.
In schools, 47 U.S. states require epinephrine to be available, but only 28 require staff to be trained. If your child has allergies, ask if the school has a plan-and if the staff know how to use it.
After You Use It
Even if symptoms disappear, go to the emergency room. About 20% of people have a second wave of symptoms hours later. This is called a biphasic reaction.
At the hospital, they’ll monitor your breathing, blood pressure, and heart. You may get additional treatments like oxygen, IV fluids, or steroids to prevent a rebound reaction.
Afterward, replace your auto-injector. You can’t reuse it. Talk to your allergist about updating your emergency plan. Maybe you need a second device for school or work.
Final Reminder
Anaphylaxis doesn’t wait. Epinephrine saves lives. The difference between using it right and waiting too long is often the difference between life and death.
Know your device. Practice regularly. Tell the people around you how to use it. Don’t wait for the perfect moment. If you think it’s anaphylaxis-use it. Then call for help.
It’s not just about carrying a device. It’s about being ready to act when it matters most.








9 Comments
Look, I get it - epinephrine saves lives, but let’s be real: 85% of the market is EpiPen because Big Pharma bought the FDA’s lunch. Auvi-Q’s voice instructions? Cute. Neffy’s nasal spray? A marketing gimmick for people who cry at needles. The real issue is cost. $700 for a plastic pen that expires in 18 months? That’s not healthcare - that’s extortion. And don’t get me started on insurance loopholes. If you’re not rich, you’re just gambling with your kid’s life. #PharmaIsTheProblem
Thank you for this. I’m a mom of a 6-year-old with peanut allergies, and I’ve been terrified of using the EpiPen until now. I practiced with the trainer on a banana last weekend - yes, really. It felt weird, but now I’m not shaking every time we leave the house. I told my daughter’s teacher, her babysitter, and even the guy at the ice cream shop. Knowledge is power, and sharing it saves lives. You’re not alone. We’ve got this.
Incorrect. Epinephrine doesn’t ‘tighten blood vessels’ - it’s a non-selective alpha and beta-adrenergic agonist that induces vasoconstriction via alpha-1 receptor activation, bronchodilation via beta-2 stimulation, and inhibits mast cell degranulation. The mechanism is pharmacologically nuanced. Also, ‘safety cap’ is a misnomer - it’s a safety release mechanism requiring deliberate axial force. And Neffy’s bioavailability? Only 50% of EpiPen’s IM delivery. The 32% misuse rate isn’t user error - it’s poor ergonomics and lack of standardized training protocols. You’re oversimplifying a complex pharmacological intervention.
So let me get this straight: you’re telling me I need to stab my thigh with a pen… then call 911… then pray?!!! And I’m supposed to do this while my kid’s face is turning into a balloon??!?!?!? I’m not a doctor, I’m a barista who just wants to make it to Tuesday without someone dying in my coffee shop. I need a freaking robot. Or a wizard. Or a really loud voice that says ‘PUSH HARDER, YOU GOT THIS!’ - oh wait, Auvi-Q does that. I’m switching. Also, why does this cost more than my rent?!
As someone who’s traveled to over 40 countries and seen emergency response systems from rural Nigeria to Tokyo, I can tell you that the U.S. approach to epinephrine access is uniquely fragmented. In Japan, schools have mandatory training and devices are subsidized. In Germany, pharmacists conduct free quarterly demos. Here? We rely on parents who are terrified and underinsured to carry life-saving devices that cost more than a monthly Netflix subscription. The cultural disconnect is staggering. We treat anaphylaxis like a personal responsibility rather than a public health imperative. It’s not just about the injector - it’s about how we value human life in crisis.
It is a moral failing - a profound and indefensible one - that the American healthcare apparatus has commodified the very substance that prevents death in the most vulnerable among us. Epinephrine, a naturally occurring catecholamine synthesized in the adrenal medulla, has been transformed into a profit-driven commodity, priced beyond the reach of the working class. One cannot claim to uphold the sanctity of life while simultaneously pricing its preservation out of reach. This is not healthcare. This is a moral abomination dressed in pharmaceutical branding.
In Nigeria, we don’t have EpiPens. We have mothers. We have neighbors. We have hands that hold, voices that shout, and feet that run to the clinic - sometimes five miles away. If you have a device, you are lucky. But don’t mistake access for wisdom. In Lagos, we teach children to recognize swelling before it’s visible - a tingling tongue, a whisper in the chest. We don’t wait for the click. We act on instinct. The pen is a tool, but courage? That’s the real medicine. Don’t just carry it - be ready to be the reason someone breathes.
It is imperative to note that the assertion that epinephrine reduces mortality by 75% is statistically misleading. The cited figure originates from observational cohort studies with significant confounding variables, including prehospital response time, comorbidities, and concomitant administration of antihistamines. No randomized controlled trial has established causality. Furthermore, the recommendation to administer epinephrine at the ‘first sign’ of reaction lacks evidence-based specificity. Premature administration may lead to iatrogenic tachycardia, hypertension, and myocardial ischemia. Caution, not urgency, must guide clinical decision-making.
Okay, I’m the guy who used his EpiPen on his own kid last year. Didn’t know how. Panicked. Missed the thigh. Hit the butt. Felt like a failure. But I called 911. We got to the ER. Kid’s fine. Now I carry two. I trained my wife. I taught my kid’s soccer coach. I even made a stupid little video on TikTok (don’t judge). If you’re reading this and you’re scared? You’re not alone. The device doesn’t make you brave. Using it does. So go practice. Now. Your future self will thank you. 😅💉