
If you’ve been living with bloating, cramps, diarrhea, or constipation that won’t quit, you’re not alone. About 1 in 7 people worldwide have irritable bowel syndrome (IBS), and for many, food is the hidden trigger. But not all diets work the same. The FODMAP diet, low-residue diet, and elimination diets are often mixed up - yet they’re wildly different in how they work, who they help, and how long you need to stick with them. This isn’t about cutting out everything you love. It’s about finding out exactly what’s making you sick - and bringing back the foods you can actually tolerate.
What the FODMAP Diet Really Does
The low-FODMAP diet isn’t just another gluten-free or dairy-free trend. It was developed by scientists at Monash University in Australia after years of research into how certain carbohydrates ferment in the gut. These carbs - called FODMAPs - pull water into the intestines and get eaten by gut bacteria, creating gas, bloating, and pain. The diet doesn’t eliminate all carbs. It targets five specific types: fructans, galacto-oligosaccharides (GOS), lactose, excess fructose, and polyols.
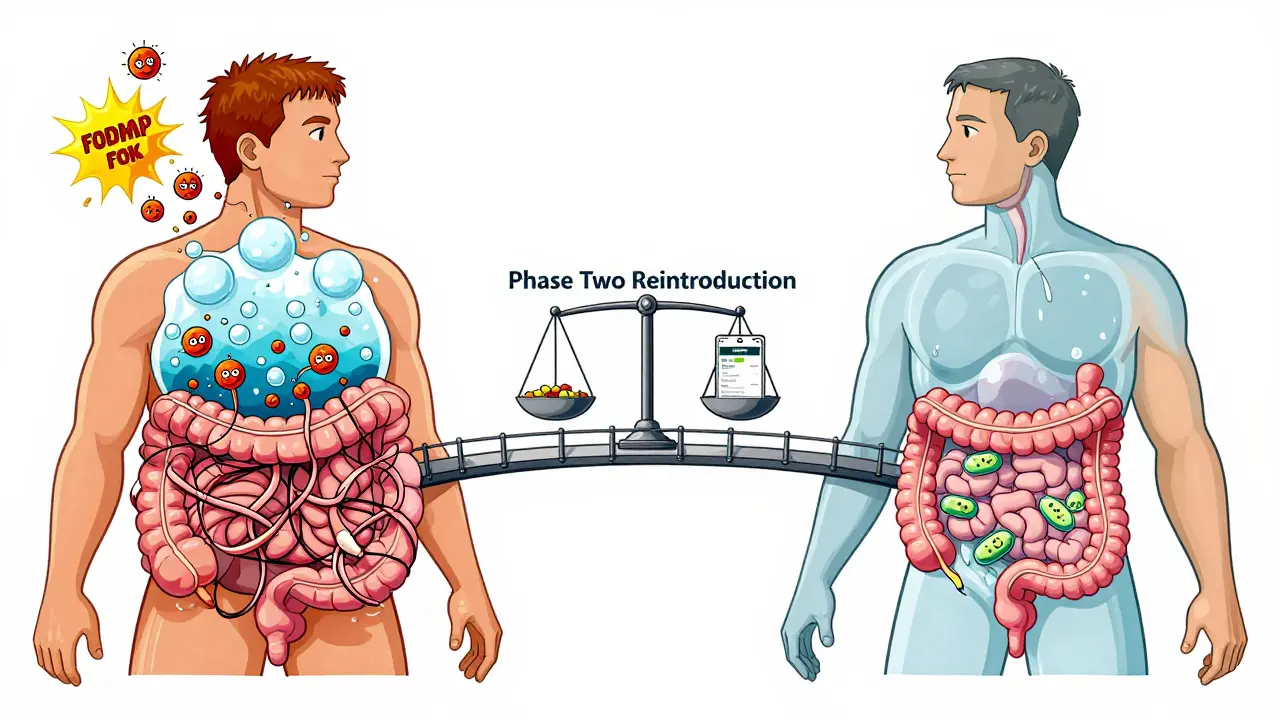
There are three phases. Phase one is strict: you cut out all high-FODMAP foods for 2 to 6 weeks. That means no garlic, onions, wheat, apples, honey, or artificial sweeteners like sorbitol. You eat only foods tested and certified as low-FODMAP - like bananas, carrots, rice, and lactose-free yogurt. Portion size matters. Even a small amount of garlic can trigger symptoms. One teaspoon of minced garlic? High-FODMAP. Half a teaspoon? Usually safe.
Phase two is where the real magic happens. You slowly bring back one FODMAP group at a time, using exact doses: 3 grams of fructans, 5 grams of GOS, 12 grams of lactose, and so on. You track your symptoms for 3 days after each challenge. Most people find they’re only sensitive to one or two groups - not all five. Phase three is personalization. You don’t have to live on plain rice and chicken forever. You rebuild your diet around what you can handle. Studies show 75% to 80% of IBS patients get major relief, especially with bloating and diarrhea.
Low-Residue Diet: When Less Fiber Helps
The low-residue diet is older, simpler, and often misunderstood. It was designed for people with inflammatory bowel disease or before bowel surgery - not for general IBS. The goal? Reduce the amount of undigested food moving through your gut. That means cutting fiber to just 10-15 grams a day (most adults need 25-38 grams). You avoid raw fruits and veggies, nuts, seeds, whole grains, beans, and skins on produce. Even oatmeal and brown rice are off-limits. Dairy is limited to lactose-free versions because many IBS patients also have trouble digesting lactose.
This diet can help if you have diarrhea-predominant IBS and need quick relief. Less fiber means fewer stools and less urgency. But it’s not a long-term fix. After a few weeks, you’ll likely feel sluggish, constipated, or nutrient-deficient. Folate and calcium intake drop significantly. And if you have constipation-predominant IBS? This diet will make it worse. It’s like putting a bandage on a broken bone - it masks the problem, but doesn’t fix it. Most gastroenterologists now recommend it only for short-term use, not as a primary IBS treatment.
Elimination Diets: The Wild Card
General elimination diets are the DIY version of FODMAP. You cut out common triggers - dairy, gluten, caffeine, eggs, soy - for 2 to 4 weeks, then add them back one at a time. Sounds simple, right? It’s not. The problem? No standard rules. You might cut out gluten thinking it’s the culprit, but your real trigger is fructans in wheat. Or you might blame dairy, when it’s actually the lactose in cheese, not the protein. Without knowing which FODMAP group you’re sensitive to, you’re guessing.
Studies show only 30% of people correctly identify their trigger foods without professional help. That’s why many end up eliminating foods they can actually eat. It’s exhausting. You lose variety, social meals, and sometimes even joy in eating. The FODMAP diet, by contrast, uses science-backed challenges. You know exactly what you’re testing and how much. That precision makes all the difference.
Which Diet Works Best - And For Whom?
Here’s how they stack up:
| Feature | Low-FODMAP Diet | Low-Residue Diet | General Elimination Diet |
|---|---|---|---|
| Primary goal | Identify specific carbohydrate triggers | Reduce stool volume | Find food sensitivities |
| Effectiveness for IBS | 75-80% symptom improvement | 45% improvement (best for diarrhea) | 40-50% improvement |
| Duration | 3-6 months (with reintroduction) | 2-4 weeks max | 2-4 weeks |
| Best for | Bloating, gas, IBS-D, mixed IBS | Acute diarrhea, pre-surgery | People without access to FODMAP resources |
| Risks | Reduced gut bacteria diversity, nutritional gaps if prolonged | Nutrient deficiencies, worsens constipation | Over-restriction, misidentification of triggers |
| Professional support needed? | Highly recommended | Optional | Strongly recommended |
The low-FODMAP diet wins for most people with IBS. It’s the only one backed by over 20 randomized trials and endorsed by the American College of Gastroenterology as a first-line treatment. But it’s not for everyone. If you have a history of eating disorders, it can trigger unhealthy behaviors. If you’re constipation-predominant, you might need a different approach - like increasing soluble fiber (psyllium) or trying peppermint oil. And if you’re in a rural area with no access to a dietitian, the low-residue diet might be a temporary bridge - but only until you can get proper guidance.
Real People, Real Results
On Reddit’s r/FODMAP community, over 140,000 people share their journeys. One user, u/IBSWarrior2020, said: “Phase one gave me 80% relief in 10 days. But reintroduction? Brutal. I only react to fructans and polyols. Now I can eat onions again - just not in big chunks.” That’s the power of personalization.
Others aren’t so lucky. A 2023 survey found 65% of people who tried FODMAP without a dietitian got stuck in phase one. They didn’t know how to reintroduce foods. Some gave up entirely. Others ate too much too fast and ended up with worse symptoms than before. The Monash FODMAP app - with its barcode scanner and portion guides - helps. It’s rated 4.8 out of 5 by nearly 30,000 users. But apps can’t replace human guidance.
One woman in her 50s, after 15 years of daily diarrhea, finally got control after working with a certified FODMAP dietitian. “I thought I had to give up everything. Turns out, I just had to stop eating garlic bread and applesauce. That’s it.”

How to Start - Without Getting Overwhelmed
Don’t go cold turkey. Start by tracking your symptoms for two weeks. Note what you eat, when you eat it, and how you feel. Look for patterns. Then, talk to a registered dietitian trained in FODMAPs. You can find certified ones through Monash University’s directory - they’re in 37 countries.
If you can’t find one, use the Monash app. Download it. Learn the low-FODMAP list. Plan your meals ahead. Cook in batches. Keep a symptom journal. Don’t skip phase two. That’s where you reclaim your freedom. Most people end up eating 50-80% of the foods they thought they had to give up forever.
Watch out for hidden FODMAPs. Soy sauce, protein bars, salad dressings, and even some “healthy” snacks are loaded with inulin, honey, or agave. Read labels like a detective. Look for: garlic powder, onion powder, high-fructose corn syrup, inulin, chicory root, sorbitol, mannitol, xylitol.
And don’t stress about perfection. One study found people who followed the diet 85% of the time still saw 70% symptom improvement. You don’t have to be flawless. You just have to be consistent.
What Comes Next?
The future of IBS diets is personalization. Researchers are testing blood and stool biomarkers to predict who will respond to FODMAP. AI tools are being built to suggest meals based on your symptoms. By 2026, your doctor’s electronic health record might automatically flag low-FODMAP options when you’re prescribed medication.
But for now, the best tool you have is knowledge - and patience. This isn’t a quick fix. It’s a journey to understand your body. The goal isn’t to live on a restricted diet forever. It’s to find your own version of freedom - where you can eat a bowl of pasta, a slice of pizza, or a peach without fear.
Can I do the low-FODMAP diet without a dietitian?
Yes, but it’s riskier. Many people skip the reintroduction phase and stay on the strict diet too long, which can harm gut bacteria and lead to nutrient gaps. Using the Monash FODMAP app and tracking symptoms carefully helps. But working with a certified dietitian increases success by 40% and reduces the chance of mistakes.
Is the low-residue diet safe for long-term IBS management?
No. It’s meant for short-term use, like after surgery or during a flare-up. Long-term, it causes low fiber intake, which leads to constipation, poor gut health, and nutrient deficiencies - especially in calcium and folate. It’s not a solution for ongoing IBS symptoms.
Will I ever be able to eat onions or garlic again?
Many people can - but not in large amounts. During reintroduction, you test tolerance. You might find you can handle 1/2 teaspoon of cooked garlic or a small amount of green onion tops. It’s not all or nothing. Most people end up with a flexible diet where they enjoy small portions of previously restricted foods.
Does the FODMAP diet help with constipation?
It helps less than it does for diarrhea. About 40-50% of constipation-predominant IBS patients see improvement. For these cases, adding soluble fiber like psyllium or using peppermint oil capsules often works better. FODMAPs aren’t the main trigger in constipation - gut motility is.
How long does it take to see results on the FODMAP diet?
Most people notice improvement within 2 to 6 weeks during the elimination phase. Some feel better in just a few days. But full results come after reintroduction - when you learn what you can actually tolerate. That takes 8 to 12 weeks. Don’t rush it. The goal is long-term freedom, not just quick relief.
Can I drink alcohol on the low-FODMAP diet?
Some types are okay in small amounts. Vodka, gin, and tequila (pure, no mixers) are low-FODMAP. Wine in moderation (one glass) is usually fine. But beer, cider, and sweet cocktails with high-fructose syrups or honey are not. Always check the Monash app for specific drinks - alcohol can irritate the gut even if it’s low-FODMAP.
What if the FODMAP diet doesn’t work for me?
About 20-25% of people don’t respond. That doesn’t mean you’re broken - it means your triggers might be different. Other options include peppermint oil, gut-directed hypnotherapy, or addressing small intestinal bacterial overgrowth (SIBO). Talk to your doctor. There are other paths. The FODMAP diet is powerful, but it’s not the only one.









14 Comments