
What Exactly is Osteoporosis?
Over 10 million Americans have osteoporosis, and another 44 million are at risk. This silent disease weakens bones, making them prone to fractures from minor falls or even everyday activities. Unlike common myths, it's not just an 'old person's problem'-bone loss starts decades earlier. But there's hope. Bisphosphonate Therapy is one of the most effective ways to slow bone loss and prevent fractures. Let's break it down.
Osteoporosis is defined by low bone mineral density (BMD) caused by deteriorating bone structure. It's not a normal part of aging-it's a medical condition where bone breakdown outpaces rebuilding. The World Health Organization established diagnostic criteria in 1994 based on BMD measurements, which we measure using a DXA Scan (dual-energy X-ray absorptiometry).
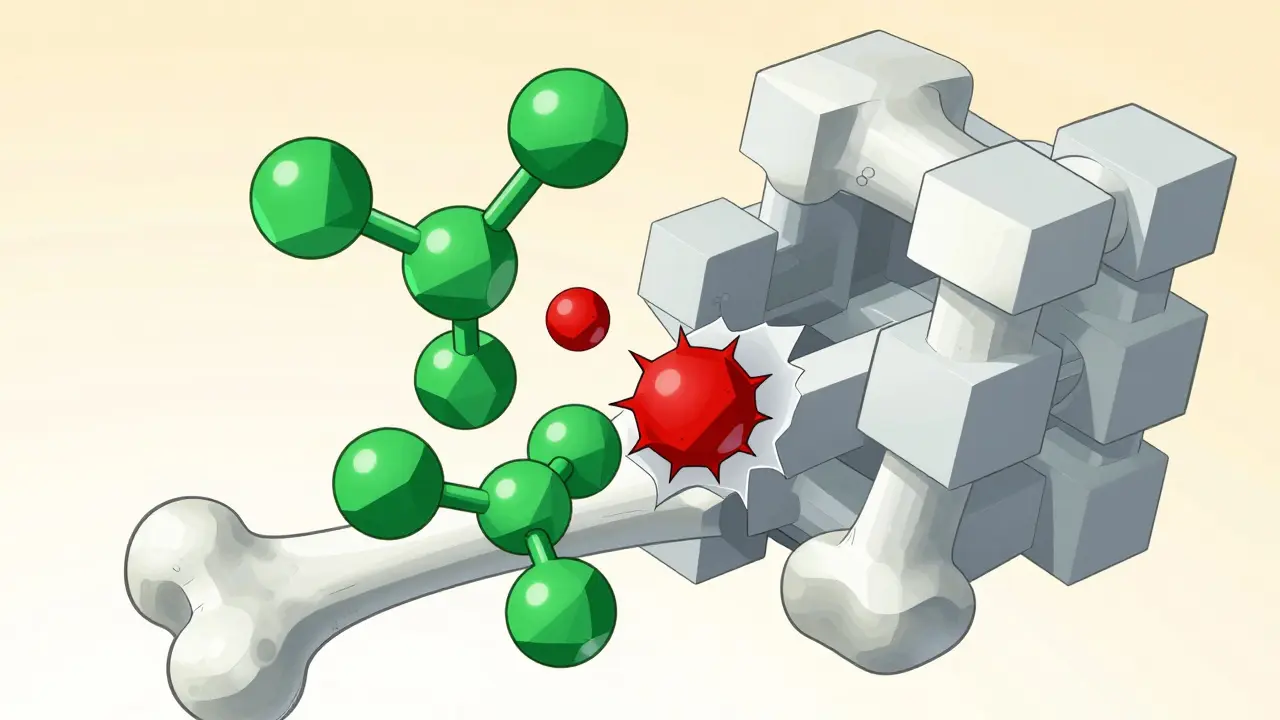
How Bisphosphonates Fight Bone Loss
Bisphosphonates are the most common treatment for osteoporosis. These drugs stick to bone surfaces and block cells called osteoclasts that break down bone. Think of them as "bone guardians" slowing down the destruction process. By doing this, they help maintain bone density and reduce fracture risk. The first bisphosphonate, etidronate, was used in the 1980s. Today, nitrogen-containing bisphosphonates like alendronate and zoledronic acid are first-line treatments because they're more effective.
Bisphosphonate Therapy works by inhibiting the enzyme farnesyl pyrophosphate synthase in osteoclasts. This stops bone resorption and can even trigger osteoclast death. The result? Slower bone loss and stronger bones over time. Clinical trials show alendronate reduces spine fractures by 48% and hip fractures by 51% over three years. Zoledronic acid cuts hip fracture risk by 41% in seniors.
Oral vs. IV: Choosing Your Bisphosphonate
Not all bisphosphonates are the same. Oral options like alendronate (Fosamax) and risedronate (Actonel) are taken weekly or monthly. You have to take them on an empty stomach with a full glass of water, then stay upright for 30-60 minutes. This is crucial-lying down too soon can cause stomach irritation. IV versions like zoledronic acid (Reclast) are given once a year in a doctor's office. They bypass the stomach, so they're great for people with digestive issues. But IV treatments require a clinic visit and can cause flu-like symptoms for a few days.
Alendronate is the most prescribed oral bisphosphonate. It's affordable-often under $40 a month as a generic. Risedronate is similar but may cause fewer stomach issues. For those who can't tolerate oral meds, Zoledronic Acid (Reclast) is a yearly IV infusion that's highly effective. However, it's not for people with severe kidney problems.
Benefits and Risks: What You Need to Know
Bisphosphonates aren't perfect. They work well for most people-reducing fractures by up to 50% in high-risk patients. But side effects happen. About 10-15% of oral bisphosphonate users get stomach pain or heartburn. Rare but serious risks include atypical femur fractures (3-5 cases per 10,000 patient-years) and osteonecrosis of the jaw (0.01-0.04% of patients). These risks are higher with long-term use, which is why doctors often recommend a "drug holiday" after 3-5 years for low-risk patients.
Osteonecrosis of the Jaw is a rare condition where jawbone tissue dies. It's linked to high-dose bisphosphonates used in cancer treatment, but it can occur in osteoporosis patients too. Dentists often recommend a dental checkup before starting bisphosphonates to reduce this risk. Atypical Femur Fractures are unusual breaks in the thigh bone. They're rare but can happen after years of bisphosphonate use. Doctors monitor patients closely for these signs.
Alternatives to Bisphosphonates
Not everyone can take bisphosphonates. For those who can't, there are alternatives. Denosumab (Prolia) is a monthly injection that blocks a protein involved in bone breakdown. It's as effective as bisphosphonates but requires consistent dosing-stopping it suddenly can cause rapid bone loss. Teriparatide (Forteo) is a daily injection that actually builds new bone. It's used for severe osteoporosis but costs over $1,800 a month and is limited to two years of use. Newer options like romosozumab (Evenity) boost bone formation while slowing breakdown, but it carries heart risks and is only used for one year.
Denosumab (Prolia) is popular for patients who can't tolerate oral bisphosphonates. It lowers fracture risk by 68% for spine fractures but needs lifelong use. Teriparatide (Forteo) is unique-it's an anabolic drug that stimulates bone growth. It increases bone density by 9-13% in 18-24 months, but it's expensive and short-term. Romosozumab (Evenity) offers dual action but has a black box warning for heart attack risk.

Practical Tips for Treatment Success
Taking bisphosphonates correctly matters. For oral pills, take them first thing in the morning with a full glass of water. Stay upright for 30-60 minutes-no lying down or eating. Skip them if you have kidney problems (creatinine clearance below 30-35 mL/min). Your doctor will check your bone density every 1-2 years with a DXA scan. If you're on a drug holiday, keep up calcium and vitamin D intake. Exercise like walking or weight training also strengthens bones. And never stop taking bisphosphonates without talking to your doctor-sudden discontinuation can increase fracture risk.
FRAX Score is a tool doctors use to estimate your 10-year fracture risk. Treatment usually starts if your score is above 20% for major osteoporotic fractures or 3% for hip fractures. DXA Scan is the gold standard for measuring bone density. It's a quick, painless X-ray that helps track your bone health over time.
Frequently Asked Questions
How long does it take for bisphosphonates to work?
Bisphosphonates start working immediately to slow bone loss, but it takes about 1-2 years to see measurable improvements in bone density. Doctors usually check bone density with a DXA scan after 1-2 years to assess progress. However, the main goal is preventing fractures, which can happen even before density numbers change significantly.
Can I stop taking bisphosphonates after a few years?
Yes, but only under doctor supervision. For low-risk patients, a "drug holiday" after 3-5 years may be recommended to reduce rare side effects. However, stopping without guidance can lead to rapid bone loss and increased fracture risk. Your doctor will monitor your bone density and fracture risk before deciding.
What's the difference between oral and IV bisphosphonates?
Oral bisphosphonates (like alendronate) are taken by mouth weekly or monthly. They require careful dosing-on an empty stomach, upright for 30-60 minutes. IV bisphosphonates (like zoledronic acid) are given once a year in a clinic. They bypass the stomach, so they're better for people with digestive issues, but may cause flu-like symptoms after infusion.
Are there side effects I should watch for?
Common side effects include stomach pain or heartburn for oral bisphosphonates. Rare but serious risks include atypical femur fractures (thigh bone breaks) and osteonecrosis of the jaw (jawbone damage). If you experience severe thigh or groin pain, jaw pain, or numbness, contact your doctor immediately. Most side effects are manageable with proper monitoring.
Why do doctors recommend calcium and vitamin D with bisphosphonates?
Bisphosphonates work best when your body has enough calcium and vitamin D to build new bone. Without these nutrients, the drugs can't do their job effectively. Most doctors recommend 1,200 mg of calcium and 800-1,000 IU of vitamin D daily. Food sources like dairy, fortified cereals, and sunlight exposure help, but supplements are often needed.









12 Comments
Bisphosphonates are a critical tool in managing osteoporosis, but understanding how they work is key. These medications target osteoclasts, the cells responsible for breaking down bone, thereby slowing down bone loss. For example, alendronate has been shown to reduce spine fractures by up to 48% and hip fractures by 51% over three years in clinical trials. However, long-term use requires careful monitoring for rare side effects like atypical femur fractures or osteonecrosis of the jaw. It's important to note that these side effects are extremely rare-about 3-5 cases per 10,000 patient-years for femur fractures and 0.01-0.04% for jaw issues. Many patients also need to take calcium and vitamin D supplements to support bone health while on bisphosphonates. Regular weight-bearing exercises like walking or strength training can further enhance bone strength. Additionally, your doctor might recommend a 'drug holiday' after 3-5 years for low-risk patients to reduce side effect risks. It's crucial to have regular DXA scans to monitor bone density and adjust treatment as needed. Remember, osteoporosis isn't just about taking medication-it's a comprehensive approach involving lifestyle changes and consistent medical care. Always consult your healthcare provider before making any changes to your treatment plan. The key is staying informed and proactive about your bone health. Small steps make a big difference in preventing fractures and maintaining mobility as you age. Proper adherence to dosing instructions, like taking oral bisphosphonates on an empty stomach and staying upright for 30-60 minutes, is also essential for effectiveness and avoiding side effects. Bone health is a lifelong journey, and working closely with your doctor ensures the best outcomes.
Osteoporosis is often misunderstood as solely an aging issue, but bone loss begins decades before symptoms appear. The DXA scan is the gold standard for diagnosis, measuring bone mineral density. Bisphosphonate therapy is effective, but alternatives like denosumab exist for those who cannot tolerate oral medications. It's important to have regular check-ups to assess bone density and adjust treatment accordingly.
Take it with water and stay upright for 30 minutes-no exceptions.
Bisphosphonates are a scam by Big Pharma they cause more harm than good the real problem is poor diet and lack of exercise doctors push these drugs to make money no one talks about natural alternatives
You're absolutely right about taking it properly! Consistency is key. I've seen so many people skip the upright part and wonder why they have stomach issues. Staying upright for 30-60 minutes isn't just a suggestion-it's critical. Also, don't forget to get outside for sunlight and maybe a walk. Your bones will thank you!
Ah yes, another 'miracle drug' from the pharmaceutical industry. Because nothing says 'healthcare' like a pill that causes jawbone rot and thigh fractures. But hey, at least it's covered by insurance, right? Let's all take our bisphosphonates and hope for the best!
I think u r being a bit harsh. Bisphosphonates have helped many people. Sure, there are risks, but theyre rare. Maybe instead of blaming pharma, we should focus on proper usage and monitoring. Like taking calcium and vitamin D. Also, regular checkups. Its not perfect, but its better than nothing.
American healthcare is the best in the world. Why are we even talking about alternatives? Bisphosphonates are the standard for a reason. If you can't afford it, get a better job. We don't need foreign alternatives-American medicine is superior.
Exactly. American healthcare leads the world. Those who criticize it just don't appreciate the quality care available. If you're not taking bisphosphonates, you're endangering your health. It's irresponsible to suggest alternatives without evidence.
You think it's about health? It's about control. The government and pharma are in cahoots to keep us dependent on drugs. They don't want us to know about natural bone-building methods. They're hiding the truth. Wake up people!
Hey everyone, let's keep it positive. Bisphosphonates are great-American science at its best. If you're having issues, talk to your doctor. We're all in this together. Stay strong and take care of your bones!
Toxic positivity. You're just repeating what the pharma reps told you. Real talk-bisphosphonates have serious risks. Your 'stay strong' nonsense ignores people who actually have side effects. It's not about being positive; it's about being honest.