
Heartburn Risk Calculator
Calculate your personalized heartburn risk based on medications you're taking and spicy food consumption. This tool helps you identify potential triggers and make informed decisions about your diet and medication timing.
Your Medication Factors
Select medications that apply to you. Some medications can significantly increase heartburn risk.
Your Spicy Food Consumption
How much spicy food do you eat? Different people have different sensitivities.
Additional Factors
These factors can also affect your heartburn risk.
Heartburn isn’t just a nuisance after a spicy taco night-it’s a signal that something deeper is going on in your digestive system. If you’re taking medications like aspirin, beta blockers, or even common antacids, and you love your hot sauce, you might be setting yourself up for a cycle of discomfort that’s harder to break than you think. The truth? Not everyone reacts the same way to spicy food or medications, but the risks are real-and avoidable.
Why Spicy Food Makes Heartburn Worse
The heat in chili peppers comes from capsaicin, and while it’s great for flavor, it’s not great for your lower esophageal sphincter (LES). This muscle is supposed to act like a one-way door, keeping stomach acid where it belongs. But capsaicin relaxes it, sometimes by 30-40% in sensitive people. That means acid can creep up into your esophagus, causing that burning feeling that climbs from your chest to your throat.
It’s not just about how much spice you eat-it’s about your body’s sensitivity. Some people can handle a full-on vindaloo with no issues. Others get heartburn from a single jalapeño. Research from the NIH in 2023 found no universal rule: spicy food doesn’t trigger reflux in everyone. But in clinical practice, 65-75% of people with GERD report clear worsening of symptoms after eating spicy meals, according to Dr. Kyle Staller of Massachusetts General Hospital.
And here’s the catch: that sensitivity can change. One day, you eat your favorite hot wings and feel fine. The next day, same meal, same sauce, and you’re doubled over. That’s because factors like stress, sleep, meal timing, and even gut bacteria can shift how your body responds. There’s no one-size-fits-all trigger list.
Medications That Make Heartburn Worse
You might not realize that some of the pills you take daily are making your heartburn worse. Common over-the-counter and prescription drugs can relax your LES or irritate your esophagus directly.
- Aspirin and NSAIDs like ibuprofen and naproxen can cause erosive esophagitis in 15-30% of regular users, according to the FDA. They don’t just hurt your stomach-they damage the lining of your esophagus.
- Beta blockers, often prescribed for high blood pressure, increase GERD risk by 22%, based on the Framingham Heart Study update from early 2023.
- Anticholinergics (used for motion sickness, overactive bladder, or Parkinson’s) reduce LES pressure by 25% in two-thirds of users, per a 2021 University of Michigan study.
- Nitrates for chest pain and theophylline for asthma both relax the LES by 35% or more.
- Bisphosphonates for osteoporosis can literally burn your esophagus if not taken with a full glass of water and you lie down too soon after.
These aren’t rare side effects-they’re well-documented. If you’re on any of these meds and get heartburn after meals, it’s not just coincidence. It’s pharmacology.
How Spicy Food Affects Your Medications
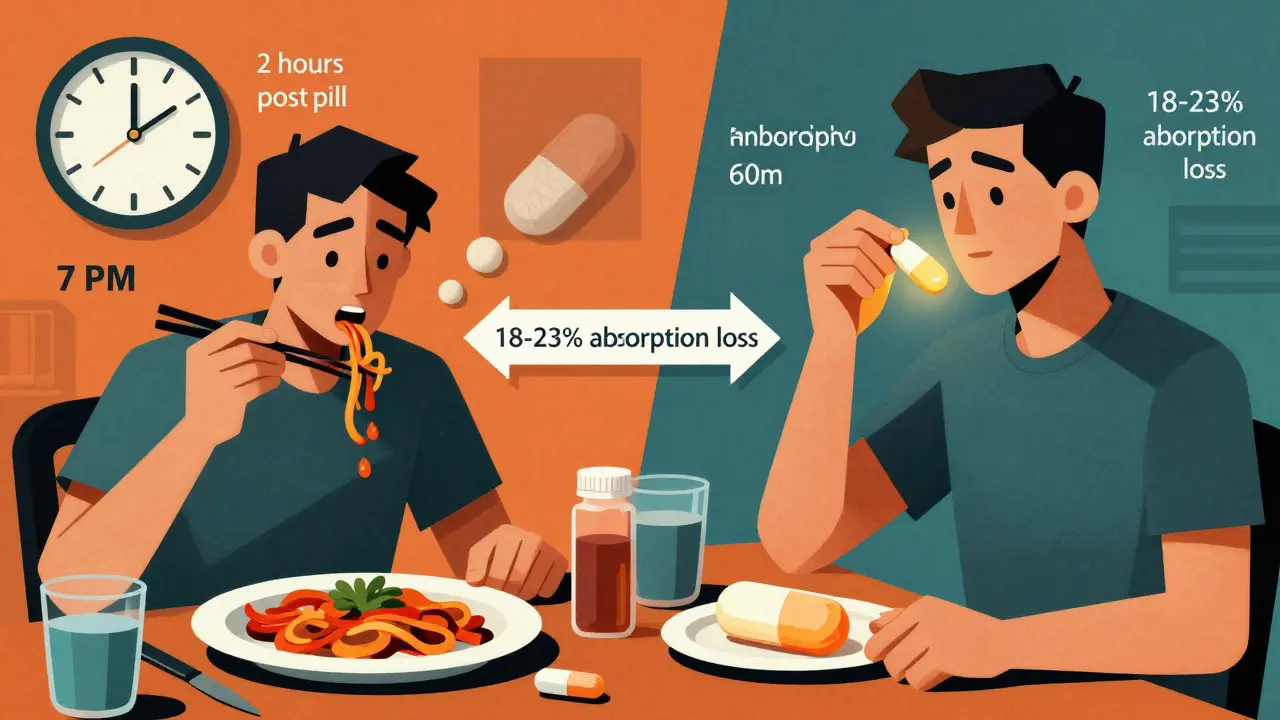
It’s not just that spicy food triggers heartburn-it can also make your heartburn meds work less effectively. Take pantoprazole, one of the most common proton pump inhibitors (PPIs). It’s designed to shut down stomach acid production. But if you take it within two hours of eating spicy, fatty, acidic, or caffeinated foods, its absorption drops by 18-23%, according to a 2022 study in the Journal of Clinical Gastroenterology.
That means you’re taking your pill on time, following the instructions, but still getting heartburn. Why? Because the food you ate is blocking the drug from working properly. The same goes for antacids like Tums or Rolaids. They give quick relief, but if you’re eating spicy food regularly, you’re just treating symptoms-not fixing the problem.
And here’s another hidden issue: antacids can interfere with other medications. Aluminum-based antacids reduce absorption of antibiotics like tetracycline by 50% and fluoroquinolones by up to 90%. If you’re on antibiotics for an infection, taking an antacid right after your meal could make your treatment fail.
What Actually Works: A Realistic Plan
Forget the idea that you have to give up spicy food forever. The goal isn’t total restriction-it’s smart management. Here’s how to do it.
- Track your triggers. Keep a simple food and symptom diary for two weeks. Note what you ate, what meds you took, when you ate them, and when heartburn hit. Be specific: “spicy chicken stir-fry with 2 tsp chili paste at 7 PM” is better than “ate spicy food.” After 10-14 days, patterns will show up.
- Try a 3-7 day elimination. Cut out all known triggers: spicy foods, caffeine, alcohol, chocolate, citrus, and fatty meals. Then slowly reintroduce them one at a time. If heartburn returns after adding back chili peppers, you’ve found your trigger. If not, you can keep eating them.
- Time your meds right. Take PPIs like pantoprazole 30-60 minutes before your first meal of the day. Never take them right after a spicy meal. Take antacids at least one hour after meals or at bedtime, and wait four hours before taking other medications.
- Don’t lie down after eating. Gravity helps. Wait at least three hours after your last meal before lying down. Elevate the head of your bed by 6-8 inches if nighttime reflux is a problem.
- Space out your meals. Eating every 3 hours gives your stomach time to empty, reducing pressure that causes reflux. Three small meals are better than two big ones.
Patients who follow this personalized approach see symptom improvement in 2-4 weeks. One Reddit user, u/SpicyFoodLover89, eliminated spicy food for three weeks while staying on pantoprazole. Symptoms vanished. Then, they slowly added back mild spices with antacids on standby. They now enjoy spicy food without daily heartburn.
When to Worry: Red Flags
Heartburn that comes and goes is annoying. Heartburn that’s getting worse, lasting longer, or changing in character? That’s a red flag.
- Difficulty swallowing
- Unintentional weight loss
- Vomiting blood or black, tarry stools
- Heartburn that wakes you up at night
- Relief from antacids that lasts less than 2 hours
These could point to something more serious: a hiatal hernia, Barrett’s esophagus, or even esophageal cancer. Antacids mask symptoms-they don’t stop disease progression. If you’re relying on them more than twice a week, talk to your doctor. The American Gastroenterological Association warns against long-term antacid use due to risks like electrolyte imbalances.

The Bigger Picture: A Shift in Treatment
The $12.5 billion GERD medication market is changing. Doctors are moving away from “take a pill and eat whatever you want” to “find your triggers and adjust.” The FDA’s 2023 guidelines now support “precision nutrition”-tailoring advice to your body, not a one-size-fits-all list.
New drugs like Vonoprazan (Voquezna), approved in August 2023, are more effective than older PPIs and work regardless of how your body metabolizes drugs. But even these won’t fix your heartburn if you keep pairing them with spicy meals and late-night snacks.
Meanwhile, research into capsaicin desensitization is promising. In a 2023 Johns Hopkins trial, 65% of participants slowly built up their spice tolerance over 12 weeks without worsening symptoms. This isn’t about becoming a chili-eating champion-it’s about regaining control.
The future of heartburn management isn’t just pills. It’s awareness, timing, and personalization. You don’t have to give up flavor. You just need to understand how your body reacts-and when to pause.
Can I still eat spicy food if I have GERD?
Yes, but not always. Many people with GERD find that spicy food worsens their symptoms, but not everyone reacts the same. The best approach is to eliminate spicy foods for 3-7 days, then reintroduce them slowly to see if they trigger heartburn. If they do, you can still enjoy them occasionally with antacids on hand-but don’t rely on them daily.
Does pantoprazole stop working if I eat spicy food?
It doesn’t stop working entirely, but its absorption drops by 18-23% when taken within two hours of spicy, fatty, or acidic foods. To get the full benefit, take pantoprazole 30-60 minutes before your first meal of the day, and avoid trigger foods close to that time.
Which medications make heartburn worse?
Common culprits include aspirin and other NSAIDs (ibuprofen, naproxen), beta blockers for blood pressure, anticholinergics (for bladder or motion sickness), nitrates for chest pain, theophylline for asthma, and bisphosphonates for osteoporosis. These either relax the muscle that blocks acid or irritate the esophagus directly.
Are antacids safe to use every day?
No. Using antacids more than 2-3 times a week can lead to electrolyte imbalances and interfere with other medications. Aluminum-based antacids can reduce absorption of antibiotics like tetracycline by up to 50%. They’re good for quick relief, but not a long-term solution.
How long does it take to see improvement after changing my diet?
Most people notice better symptom control within 2-4 weeks of making consistent changes: timing meals, avoiding triggers, and taking meds correctly. Tracking your food and symptoms for at least two weeks helps identify what’s really causing your heartburn.
Can I stop taking my GERD meds if I change my diet?
Don’t stop your medication without talking to your doctor. Some people can reduce or stop meds after successfully managing triggers, but others still need them. Stopping PPIs suddenly can cause rebound acid production, making symptoms worse. Work with your doctor to create a safe plan.
What to Do Next
Start simple: grab a notebook or use your phone’s notes app. For the next 14 days, write down everything you eat and drink, the time you took any medication, and whether you had heartburn-and how bad it was. Look for patterns. Did heartburn happen every time you had chili after taking ibuprofen? Did it disappear when you ate your spicy curry earlier in the day?
Then, talk to your doctor or a registered dietitian. Bring your notes. Ask about your medications. Ask if any could be contributing. Ask if you’re a candidate for a trial elimination diet. You don’t have to live with daily heartburn. With the right approach, you can eat what you love-without the burn.







11 Comments