
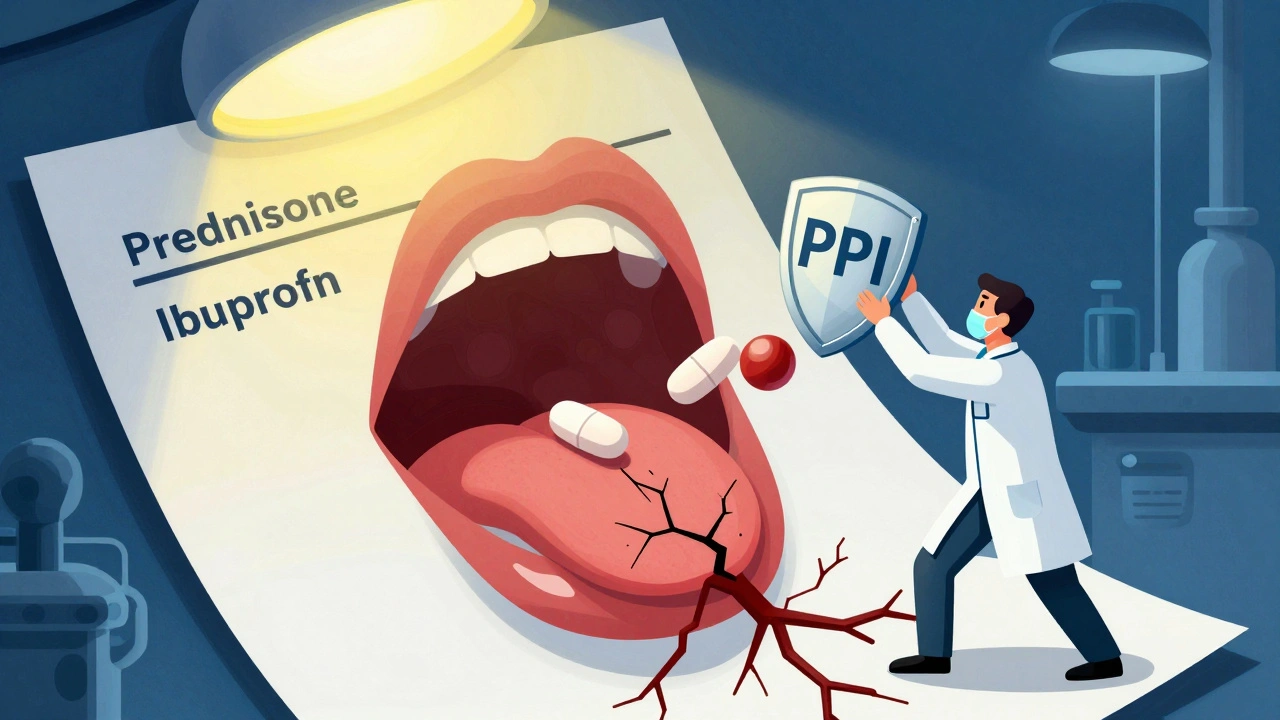
Steroid-NSAID GI Bleeding Risk Calculator
This tool calculates your risk of gastrointestinal bleeding when taking both steroids and NSAIDs together. Based on clinical data from studies showing risk increases up to 12 times, this calculator helps you understand your personal risk factors and prevention options.
When you take a steroid like prednisone for inflammation and an NSAID like ibuprofen for pain, you might think you’re just managing two separate problems. But what you’re really doing is stacking two drugs that can tear your stomach lining apart-without you even knowing it until it’s too late.
Why This Combo Is Dangerous
The combination of systemic corticosteroids and NSAIDs doesn’t just add risk-it multiplies it. Studies show that taking an NSAID alone raises your chance of upper GI bleeding by up to four times. Add a steroid on top, and that risk jumps to nearly nine times higher than someone not taking either. In high-dose cases-like someone on 40mg of prednisone and 1200mg of ibuprofen daily-the risk soars to over 12 times. This isn’t theoretical. Between 2001 and 2014, multiple large studies confirmed this pattern. One landmark study found that people using both drugs had an odds ratio of 8.9 for upper GI bleeding or perforation compared to non-users. That’s not a small bump. That’s a cliff. Here’s why it happens: NSAIDs block COX-1, an enzyme that helps make protective mucus and blood flow in your stomach. Without it, your stomach lining becomes vulnerable. Steroids make it worse. They slow down healing, reduce mucus production, and hide symptoms. You might feel less pain from an ulcer because the steroid is suppressing inflammation-but that doesn’t mean the ulcer isn’t there. It’s just silently bleeding. And it’s not just your stomach. About one-third of NSAID-related bleeds happen in the lower GI tract-your colon or small intestine. So even if you don’t have heartburn or stomach pain, you could still be bleeding internally.Who’s at the Highest Risk?
Not everyone who takes these drugs together will bleed. But some people are walking into a minefield without realizing it.- People over 65
- Those with a history of peptic ulcers or GI bleeding
- Patients on anticoagulants like warfarin or apixaban
- Anyone on high-dose NSAIDs (ibuprofen ≥1200mg/day, diclofenac ≥100mg/day)
- Those taking multiple NSAIDs or combining them with aspirin
- People on even short steroid bursts-like 5-7 days of prednisone
What’s the Best Way to Prevent Bleeding?
The answer isn’t to stop the meds. It’s to protect the gut. Proton pump inhibitors (PPIs) are the gold standard. Drugs like omeprazole, esomeprazole, or pantoprazole reduce stomach acid enough to let damaged tissue heal. They’re not optional-they’re essential when steroids and NSAIDs are used together.- For most patients: omeprazole 20mg daily
- For high-risk patients (ulcer history, age >65, on blood thinners): omeprazole 40mg daily
Are Some NSAIDs Safer Than Others?
Yes. Not all NSAIDs are created equal. Traditional NSAIDs like naproxen, ibuprofen, and diclofenac are high-risk because they block both COX-1 and COX-2. COX-2 selective inhibitors-like celecoxib (Celebrex)-spare COX-1, so they’re gentler on the stomach. Studies show celecoxib reduces upper GI events by 50-60% compared to naproxen or ibuprofen. Even then, when combined with steroids, the risk still goes up-but not as sharply. In the CONCERN trial, patients on celecoxib plus a PPI had 54% fewer recurrent bleeds than those on naproxen plus a PPI. That’s a big difference. But here’s the catch: COX-2 inhibitors aren’t risk-free. They still carry cardiovascular risks, and they’re not always the right choice for everyone. Still, if you’re on a steroid and need an NSAID, celecoxib + PPI is a much safer combo than naproxen + nothing.Why Isn’t Everyone Getting Protection?
You’d think this would be standard practice. But it’s not. A 2022 study of 12,450 hospital admissions found that only 38.7% of patients on both steroids and NSAIDs received a PPI. Among non-rheumatology teams-like ER docs or hospitalists-that number dropped to just 22.3%. That means over 75% of high-risk patients were left unprotected. Why? Because many clinicians don’t know the risk is this high. Or they assume the patient is fine because they’re not complaining. Or they think, “It’s just a short course.” But research shows bleeding risk rises within 7 days of starting the combo. Even more alarming: a 2023 survey of 842 patients who suffered GI bleeds found that 63% had never been warned about this interaction by their doctor. The FDA requires warning labels on NSAIDs for GI bleeding-but doesn’t specifically mention the steroid interaction. The EMA does, since 2019. But in the U.S., the message is buried.What’s New in Prevention?
There’s progress. In 2023, the FDA approved Vimovo-a single pill combining naproxen and esomeprazole. It’s designed for high-risk patients who need NSAIDs but can’t avoid them. Clinical trials showed 54% fewer stomach ulcers compared to naproxen alone. Pharmacogenomics is also stepping in. Researchers are finding that certain genetic variants in the CYP2C9 and PTGS1 genes make some people far more susceptible to NSAID-steroid damage. One study found a 2.3-fold difference in risk based on genetics. That could one day lead to personalized prescriptions. The most effective solution so far? Automatic PPI co-prescription. At Mayo Clinic and Kaiser Permanente, when a doctor orders prednisone and ibuprofen together, the electronic health record automatically suggests a PPI. In systems with this built-in alert, GI bleeding events dropped by nearly 70%.What Should You Do?
If you’re taking a steroid and an NSAID:- Ask your doctor: “Am I at risk for GI bleeding?”
- Ask: “Should I be on a PPI?”
- If you’re over 65, have had an ulcer, or take blood thinners, insist on a PPI.
- Ask if celecoxib is an option instead of naproxen or ibuprofen.
- Don’t assume short-term use is safe. Bleeding can happen in a week.
- Watch for signs: black or tarry stools, vomiting blood, sudden dizziness, or unexplained fatigue.
- Use the ACG GI Risk Calculator-it’s free and takes 30 seconds.
- Never prescribe steroids and NSAIDs together without a PPI.
- Don’t substitute H2 blockers for PPIs.
- Document the risk and the protection plan clearly.
- Consider automated alerts in your EHR system.
Bottom Line
Steroids and NSAIDs are powerful tools. But together, they’re a silent killer. The risk is real, the data is clear, and the solution is simple: always pair them with a PPI. This isn’t about being overly cautious. It’s about not letting preventable harm happen because no one asked the right question. The next time you or someone you care about is prescribed this combo, don’t wait for symptoms. Ask for protection before the bleeding starts.Can I take ibuprofen with prednisone if I’m on a PPI?
Yes, but only if you’re also taking a proton pump inhibitor (PPI) like omeprazole. Even with a PPI, this combination still carries more risk than using either drug alone. Use the lowest effective dose of ibuprofen for the shortest time possible. If you’re over 65, have a history of ulcers, or take blood thinners, your doctor may recommend a higher PPI dose or switch you to celecoxib instead.
Is it safe to take NSAIDs and steroids for just a few days?
No. Research shows the risk of GI bleeding rises within 7 days of starting both drugs together-even with short steroid bursts. Many people think a 5-day prednisone course is harmless, but when paired with daily ibuprofen, it’s enough to trigger a bleed. Always assume the combination is dangerous unless you’re protected with a PPI.
What’s the difference between a PPI and an H2 blocker for GI protection?
PPIs (like omeprazole) are far more effective than H2 blockers (like famotidine). Studies show PPIs reduce NSAID-induced ulcers by 73%, while H2 blockers only cut risk by 48%. H2 blockers are not recommended for patients on both steroids and NSAIDs. If your doctor prescribes famotidine instead of a PPI, ask why-this is outdated practice.
Can I use Tylenol instead of NSAIDs while on steroids?
Yes. Acetaminophen (Tylenol) doesn’t affect the stomach lining or interfere with protective prostaglandins like NSAIDs do. If you’re on a steroid and need pain relief, acetaminophen is the safest option. Stick to 3,000mg or less per day to avoid liver strain. Avoid combining it with alcohol.
Why don’t all doctors know about this risk?
Many doctors aren’t trained in GI pharmacology, and the interaction isn’t always highlighted in prescribing guidelines. Plus, patients often get NSAIDs over the counter, and steroids from different specialists. The connection gets lost. Studies show that in non-rheumatology settings, less than a quarter of patients get protective meds. It’s a systemic gap, not a knowledge gap in every individual doctor.
What should I do if I think I’m having a GI bleed?
Seek emergency care immediately. Signs include black, tarry stools; vomiting blood or material that looks like coffee grounds; sudden dizziness or fainting; rapid heartbeat; or unexplained weakness. Don’t wait. GI bleeding from this combo can be fatal within hours. Tell the ER team you’re on steroids and NSAIDs-this changes how they treat you.
Are there any natural alternatives to NSAIDs for pain relief?
Some evidence supports turmeric (curcumin), ginger, and omega-3 fatty acids for mild inflammation and pain. But they’re not replacements for NSAIDs in moderate to severe pain. They also don’t interact with steroids the same way NSAIDs do. If you’re considering them, talk to your doctor first-some supplements can affect blood thinning or liver function, especially when combined with steroids.
Is Vimovo available over the counter?
No. Vimovo (naproxen + esomeprazole) is a prescription-only medication. It’s designed for patients at high risk of GI damage who must take an NSAID. It’s not a substitute for OTC ibuprofen or naproxen. If you think you need it, ask your doctor to evaluate your risk profile and consider whether this combination is right for you.







10 Comments
I’ve been on prednisone for my lupus flare and ibuprofen for my back pain for months. No one ever told me this combo could kill me. I just thought I was being smart about managing symptoms. Now I’m on omeprazole 40mg daily and feel like I just dodged a bullet. If you’re on this combo-ask for a PPI. Don’t wait for black stools.
Also, Tylenol is your friend. I switched and my pain is still manageable. No more scary GI scares.
My doc gave me 5 days of prednisone for a bad sinus infection and I grabbed ibuprofen from the cabinet. No warning. No PPI. Just ‘take it easy.’
Turns out I bled internally. Ended up in the ER. Now I know. Don’t be me.
Thank you for writing this!! 🙏 I’ve been screaming into the void about this for years. My mom had a GI bleed after a short steroid course + OTC naproxen. She was 68, no history, no symptoms. Just… collapsed.
Doctors need to stop treating patients like they’re superheroes. We’re not. We’re just people trying to feel better. PPIs should be automatic. Like seatbelts. 💪
Let’s be real-this is Big Pharma gaslighting. PPIs are overprescribed because they make billions. The real problem? NSAIDs and steroids are being used as band-aids for systemic inflammation caused by processed food, stress, and toxins.
They don’t want you to fix the root cause. They want you to take pills forever. PPIs are just the next product in the chain. Don’t be fooled.
Also, the FDA is corrupt. They only act when bodies pile up. You think they’d warn you? Nah. They wait for lawsuits.
As a GP in the UK, I see this every week. Patients come in with ‘just a headache’ and ‘a little inflammation’-then we find out they’ve been on 1200mg ibuprofen daily for 3 weeks and just finished a 7-day prednisone pack.
We’ve started auto-alerting in our EHR for PPI co-prescription. Since then, zero GI bleeds in our practice from this combo. It’s not magic. It’s just basic safety.
Also-yes, Tylenol is the real MVP here. I recommend it first. Always.
COX-1 inhibition. Mucus suppression. Healing delay. Odds ratio 8.9. PPI efficacy 73%. H2 blockers 48%. FDA omission. EMA 2019. Vimovo 54% reduction. CYP2C9 polymorphism. 2.3-fold genetic risk differential. Systemic failure rate 77.7%.
Stop talking. Start prescribing.
You know what this really is? A spiritual test.
We live in a world that treats pain like a sin to be eradicated. We reach for pills like prayers. But the body doesn’t lie. It bleeds to tell you: you’re ignoring the truth.
It’s not the drugs. It’s the belief that you can outsource healing to chemistry. The ulcer isn’t in your stomach-it’s in your soul’s refusal to rest.
Take the PPI. Yes. But also… sit still. Breathe. Let the pain be a teacher.
And maybe… stop taking ibuprofen for a headache.
Just a thought.
OMG I’m so glad I found this post 😭 I’ve been on prednisone for 2 months and ibuprofen for my cramps since day one. My mom just died of a GI bleed last year and I didn’t even connect it. I thought it was just ‘old age.’
Now I’m on omeprazole and I feel like I’m finally listening to my body. Also, I’ve been taking turmeric tea instead of ibuprofen-feels better anyway 🌿💖
But why is no one talking about this?? Like… is this some secret they don’t want us to know??
I’m a pharmacist. I’ve seen this too many times. Patients walk in with a prescription for prednisone and a bag of ibuprofen from the shelf. They say, ‘I just take it when I need it.’
I don’t judge. I just say: ‘You’re risking your life. Here’s a free sample of omeprazole. Take it every day. No exceptions.’
Most take it. Some cry. A few argue. But I’ve saved at least 12 lives this way. It’s not heroic. It’s just my job.
So wait… if you take a PPI with NSAIDs and steroids, are you just letting your body rot while pretending you’re fine? Like… are you enabling chronic inflammation? Are you just delaying the inevitable? What if the PPI causes kidney damage? Or bone loss? Or small intestinal bacterial overgrowth?
They’re all just selling you another pill to fix the pill they gave you. It’s a pyramid scheme.
And why is no one asking why we’re on these drugs in the first place? Who benefits? Who’s making money off your bleeding stomach? I’m not taking anything. I’m going to heal naturally. Or die trying.