Have you ever looked at your prescription label and wondered why it says take on an empty stomach-or take with food? It’s not just a suggestion. Getting this wrong can mean your medicine doesn’t work, or worse, it makes you sick. For millions of people taking multiple medications every day, this simple detail can make a huge difference in how they feel, how well their treatment works, and whether they stay out of the hospital.
Let’s cut through the confusion. This isn’t about diet trends or fancy nutrition. It’s about chemistry, biology, and real-world science that’s been studied for decades. Here’s what actually happens when you take your pills with or without food-and why it matters.
Why Food Changes How Medicine Works
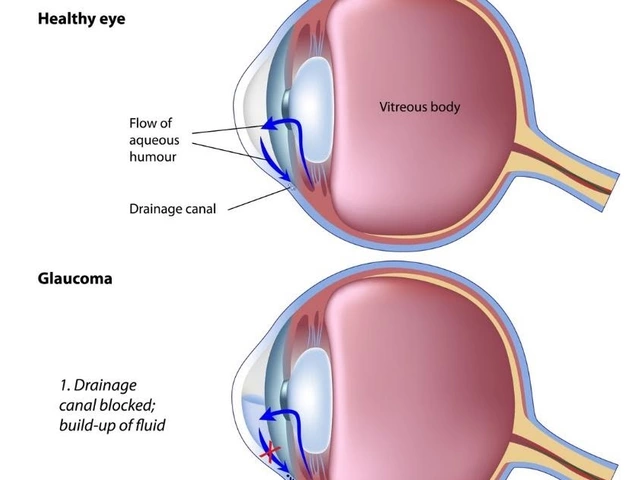
Your stomach isn’t just a bag that digests food. It’s a chemical factory. When you eat, your body releases acid, bile, enzymes, and hormones that change the environment inside your gut. These changes can either help or hurt how well your medicine gets absorbed into your bloodstream.
Some drugs need acid to dissolve properly. If you take them after a big meal, your stomach acid gets diluted, and the medicine might not break down at all. Other drugs are too harsh on an empty stomach-they can irritate your lining and cause nausea, ulcers, or bleeding. Food acts like a buffer.
And it’s not just about the stomach. Food slows down how fast your stomach empties. That means some medicines spend more time in the upper gut, where they’re absorbed best. For others, food binds to them like glue, locking them up so they can’t be absorbed at all.
According to the U.S. Food and Drug Administration, about 40% of all prescription medications have specific food instructions built into their labeling. That’s not a small number. It’s a major part of how these drugs are designed to work.
Medicines That MUST Be Taken with Food
Some drugs simply don’t work well-or are too harsh-unless you eat first. Here are the most common ones:
- NSAIDs (ibuprofen, naproxen, aspirin): These can cause stomach irritation, bleeding, or ulcers when taken on an empty stomach. The UK NHS and German medical guidelines both recommend taking them after eating. A 2021 study found that taking ibuprofen with food cuts nausea by 20%.
- Antibiotics like Augmentin (amoxicillin/clavulanate): Food reduces side effects like nausea and diarrhea. One study showed that patients who took Augmentin with food had fewer stomach issues than those who didn’t.
- Antiretrovirals (ritonavir, zidovudine): These HIV drugs are notorious for causing nausea. Taking them with a small meal or snack reduces nausea by nearly half, according to patient reports from HIV Clinic Canada.
- Nitrofurantoin and rifabutin: These antibiotics are easier on your stomach when taken with food. The NHS says this can extend their effectiveness from under an hour to up to two hours.
- Some cholesterol and HIV meds (like saquinavir): High-fat meals can boost absorption by up to 40%. That’s not a coincidence-it’s how the drug was designed to work.
And here’s a practical tip: if your doctor says take it with food, you don’t need a full meal. A banana, a handful of nuts, or even a slice of toast can be enough. One Reddit user reported that taking NSAIDs with a banana reduced stomach upset in 63% of cases.
Medicines That MUST Be Taken on an Empty Stomach
Some drugs are ruined by food. If you take them with a meal, you might as well throw them away.
- Tetracycline and doxycycline: Calcium in dairy, iron in supplements, and even magnesium in antacids bind to these antibiotics and block absorption. Studies show this can cut effectiveness by up to 50%.
- Levothyroxine (for thyroid): This one’s critical. Food can reduce absorption by 20% to 55%. The standard advice? Take it 30 to 60 minutes before breakfast. Mayo Clinic says even coffee can interfere-so wait at least an hour after taking it before drinking.
- Didanosine (an older HIV drug): Stomach acid destroys it. It must be taken on an empty stomach, with no food for at least 30 minutes before and after.
- Bisphosphonates (like alendronate for osteoporosis): These need to be taken with a full glass of water, 30 to 60 minutes before eating. Food or drink too soon can cause serious esophageal irritation.
Timing matters here. The Mayo Clinic recommends either taking these drugs 1 hour before a meal or 2 hours after. For some, like bisphosphonates, the buffer is even longer. Skipping this window can mean your bone medication doesn’t work-and you’re at risk for fractures.

What About Grapefruit Juice? And Other Surprises
Food isn’t just about meals. Some drinks and snacks can have dangerous effects.
Grapefruit juice is the classic example. It blocks an enzyme in your gut (CYP3A4) that normally breaks down certain drugs. That means more of the drug gets into your blood-sometimes too much. This can be deadly with medications like some statins, blood pressure drugs, or immunosuppressants.
Even if your label doesn’t mention grapefruit, it’s safer to avoid it entirely if you’re on chronic meds. The same goes for Seville oranges, pomelos, and some herbal teas.
And don’t forget about milk. It’s not just a problem for tetracycline. Some antifungals like ketoconazole lose effectiveness when taken with dairy because milk raises stomach pH.
Why Do Guidelines Sometimes Conflict?
You might have heard that NSAIDs should be taken on an empty stomach for faster pain relief. A 2015 review in Inflammopharmacology argued exactly that-saying there’s no strong proof that food protects the stomach. But here’s the catch: those studies were mostly on healthy young adults. The real risk isn’t for them. It’s for older people, diabetics, or those on blood thinners.
Doctors in the UK and Germany recommend food for NSAIDs in older patients because their stomachs are more fragile. The trade-off? Slower pain relief versus avoiding a hospital trip for a bleeding ulcer. For most people, safety wins.
That’s why the FDA now requires drug makers to test food effects in real patients-not just lab animals. In 2023, 78% of new drugs had food-effect data included in their approval. That’s up from 62% in 2018. The science is getting better. But it’s still not one-size-fits-all.
How to Get It Right Every Time
Managing multiple meds with different rules is hard. A 2023 GoodRx survey found that 42% of people taking five or more medications admitted to mixing up the food rules at least once.
Here’s how to avoid mistakes:
- Read every label. Don’t assume all pills work the same. Even two different brands of the same drug can have different instructions.
- Ask your pharmacist. They’re trained for this. A 2024 Express Scripts report showed patients who got clear food instructions from pharmacists had 27% better adherence.
- Use color-coded reminders. Some pharmacies now use red stickers for “empty stomach,” green for “with food,” and yellow for “with high-fat meal.” One pilot study saw adherence jump by 31%.
- Set phone alarms. “Take levothyroxine at 7 a.m.” “Take Augmentin after lunch.” Even a simple reminder cuts errors.
- Keep a log. Write down what you took, when, and with what. If you feel off, you’ll know if food might be the cause.
And if you’re confused? Don’t guess. Call your doctor or pharmacy. It’s better to ask than to risk your health.
The Future: Personalized Medicine and Your Gut
Science is moving beyond “take with food” to “take with this specific meal.” Researchers at UCSF developed a machine learning model in early 2024 that predicts how your gut microbiome affects drug absorption-with 87% accuracy in early tests.
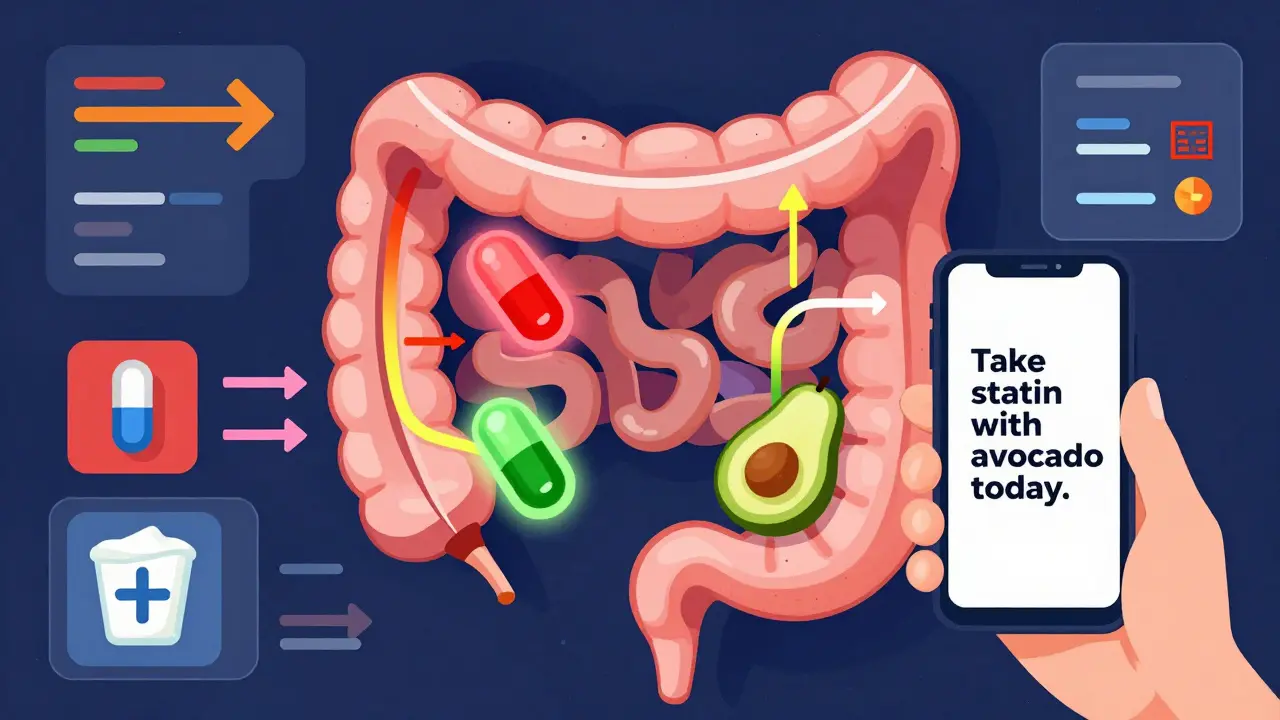
Imagine a future where your phone tells you: “Today, your gut is slow. Take your statin with a small avocado instead of toast.” That’s not sci-fi. It’s coming.
The NIH just funded $15.7 million in research to study how individual diets affect drug metabolism. The European Medicines Agency now requires food-effect studies for all new cancer drugs starting in 2025.
This isn’t just about pills anymore. It’s about matching your body, your food, and your medicine.
Final Rule: When in Doubt, Ask
There’s no universal rule. What works for one person might hurt another. Your body, your meds, your diet-they’re all unique.
So don’t rely on memory. Don’t follow a friend’s advice. Don’t assume “it’s probably fine.”
Check the label. Talk to your pharmacist. Use a reminder app. Write it down.
Because when it comes to prescription medicine, timing isn’t just important-it’s life-changing.