
QT Prolongation Risk Calculator
Input Patient Details
Risk Assessment Results
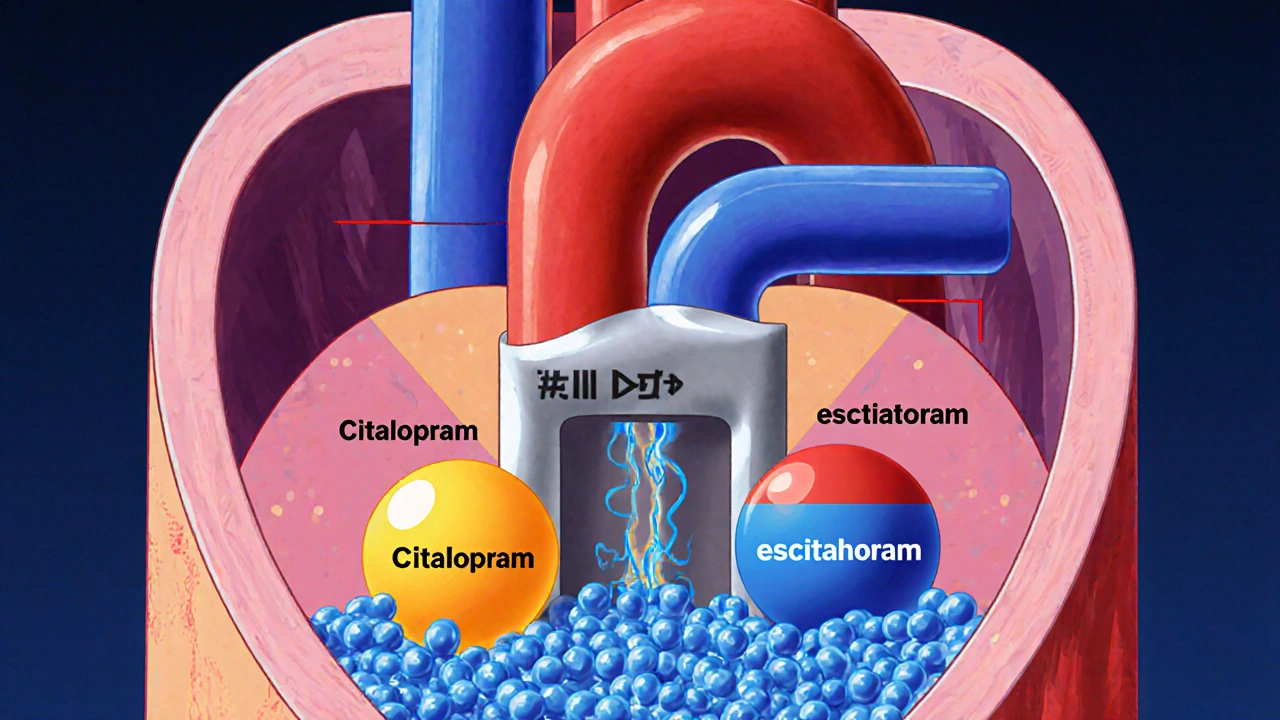
Prescribing an SSRI feels routine, but the reality check comes when the heart’s electrical system gets involved. Both Citalopram is a selective serotonin reuptake inhibitor (SSRI) that contains a mixture of R‑ and S‑enantiomers and Escitalopram is the pure S‑enantiomer of the same molecule have a hidden side‑effect: they can stretch the QT interval on an electrocardiogram. When the QT interval gets too long, the risk of dangerous arrhythmias spikes. This guide walks through the science, the numbers, and the practical limits you need to know before writing a prescription.
Key Takeaways
- Both drugs cause dose‑dependent QT prolongation, but citalopram’s effect is consistently larger.
- Regulators cap daily doses at 20 mg (citalopram) or 10 mg (escitalopram) for patients ≥65 years.
- Monitor any patient with baseline QTc ≥450 ms, electrolyte issues, or concurrent QT‑prolonging meds.
- When cardiac risk is a concern, escitalopram is usually the safer choice despite its higher price.
- Use the table below to compare typical dose‑related QTc changes and recommended maximum doses.
What Are Citalopram and Escitalopram?
Both drugs belong to the SSRI class and are first‑line treatments for major depressive disorder, generalized anxiety, and panic disorder. Citalopram is a racemic mixture of R‑ and S‑enantiomers, while escitalopram isolates the S‑enantiomer, the component most responsible for serotonin reuptake inhibition. Their efficacy is comparable, but the pharmacokinetic nuance - a single enantiomer versus a mixture - influences how they interact with cardiac ion channels.
How Do These SSRIs Touch the Heart?
The heart’s repolarisation phase relies on the rapid outward flow of potassium through hERG channels. Both drugs partially block the hERG potassium channel is a protein that conducts the delayed rectifier potassium current critical for terminating the cardiac action potential. By slowing this current, the ventricles stay depolarised a bit longer, which shows up as a prolonged QT interval on the ECG.
Blockade is modest at therapeutic doses, but it rises with higher plasma concentrations. In vulnerable patients - older adults, those with liver impairment, or anyone taking other QT‑prolonging drugs - even a small extra delay can push the QTc over the safety threshold.
QT Interval Basics and When to Worry
The QT interval measures the time from the start of ventricular depolarisation to the end of repolarisation. Because heart rate influences the raw QT value, clinicians use the corrected QT (QTc), which adjusts for rate. Two cut‑offs guide concern:
- A QTc of 500 ms or longer is generally considered high‑risk for torsade de pointes (TdP).
- An increase of 60 ms or more from a patient’s baseline also signals danger, even if the absolute value stays below 500 ms.
These thresholds come from the analysis by Hasnain, Howland, and Vieweg (2013) and are echoed in FDA and MHRA guidance.
Dose‑Response Data: How Much Does the QT Stretch?
Regulatory studies provide fairly consistent numbers. Below is a snapshot of average QTc changes observed in healthy volunteers:
| Drug | Daily Dose | Mean QTc Increase (ms) |
|---|---|---|
| Citalopram | 20 mg | 8.5 (6.2‑10.8) |
| Citalopram | 40 mg | 12.6 (10.9‑14.3) |
| Citalopram | 60 mg | 18.5 (16.0‑21.0) |
| Escitalopram | 10 mg | 4.5 (2.5‑6.4) |
| Escitalopram | 20 mg | 6.6 (5.3‑7.9) |
| Escitalopram | 30 mg | 10.7 (8.7‑12.7) |
Even the lowest approved doses add a few milliseconds - a change that may feel trivial but can tip over the 60‑ms safety line when combined with other risk factors.
Regulatory Responses Around the World
After the FDA’s August 24 2011 safety communication, most agencies tightened dose limits. The FDA is the US agency that issued the 2011 drug safety communication on citalopram‑related abnormal heart rhythms recommended 40 mg as the maximum for adults under 65 and 20 mg for those 65 and older. MHRA is the UK regulator that released a December 2011 safety update applying the same limits to both citalopram (40 mg/20 mg) and escitalopram (20 mg/10 mg) for the elderly. Health Canada followed suit with comparable caps. New Zealand’s Medsafe issued a March 2012 notice mirroring the UK approach.
Why the slight differences? The UK and European authorities interpreted the dose‑QT data more conservatively, extending lower caps to escitalopram even though its QT effect is smaller. Canada kept the focus on citalopram because of its larger absolute change.
Practical Dose Limits for Different Patient Groups
- Adults < 65 years: Citalopram ≤40 mg/day, Escitalopram ≤20 mg/day.
- Adults ≥65 years: Citalopram ≤20 mg/day, Escitalopram ≤10 mg/day. The reduced metabolism in older adults raises plasma concentrations, so the lower ceiling mitigates extra QT stretch. \n
- Hepatic impairment (moderate): Treat as if the patient were elderly - halve the usual maximum dose.
- Concomitant QT‑prolonging drugs (e.g., certain anti‑psychotics, macrolide antibiotics): Consider dropping to half the standard ceiling and schedule an ECG within 1‑2 weeks of initiation.
- Baseline QTc ≥450 ms: Either avoid these SSRIs or use the minimum effective dose with strict ECG monitoring.
In practice, many clinicians start at the lowest effective dose (10 mg citalopram or 5 mg escitalopram) and titrate only if symptom control is inadequate.

Comparing the Cardiac Risk Profiles
While both drugs can prolong QT, the magnitude and the clinical narrative differ. Below is a concise side‑by‑side view:
| Aspect | Citalopram | Escitalopram |
|---|---|---|
| Enantiomer composition | R + S (racemic) | S‑only |
| Typical QTc rise at max approved dose (adult <65) | ≈12.6 ms at 40 mg | ≈6.6 ms at 20 mg |
| Regulatory max dose (elderly) | 20 mg | 10 mg |
| Cost (US 2024 average) | $0.15 per tablet | $0.25 per tablet |
| Preferred when cardiac risk present | Generally avoided if alternatives exist | Often chosen despite higher price |
The numbers confirm why many prescribers lean toward escitalopram for patients with known QT issues, even though both remain viable with proper safeguards.
Monitoring and Mitigation Strategies
When you decide a patient needs one of these SSRIs, follow a simple checklist:
- Obtain a baseline ECG. Record QTc and look for values ≥450 ms.
- Review current meds for other QT‑prolonging agents (e.g., fluoroquinolones, certain antipsychotics).
- Check electrolytes - low potassium, magnesium, or calcium amplify the risk.
- Start at the lowest recommended dose for the patient’s age and liver function.
- Repeat ECG after 1-2 weeks, especially if you exceeded 10 mg citalopram or 5 mg escitalopram, or if the patient has cardiac comorbidities.
- If QTc climbs >30 ms from baseline or exceeds 500 ms, either reduce the dose, switch to a non‑QT affecting antidepressant (e.g., sertraline), or involve cardiology.
Education matters too. Tell patients to report palpitations, dizziness, or fainting immediately - these can be early signals of dangerous arrhythmias.
Bottom Line for Clinicians
Both citalopram and escitalopram are effective antidepressants, but their cardiac footprints differ enough to shape prescribing decisions. Citalopram’s larger dose‑related QT increase and broader regulatory warnings make it less attractive for patients over 65, those with hepatic impairment, or anyone on a QT‑prolonging cocktail. Escitalopram offers a gentler profile, yet you still need to respect the lower dose caps and monitor high‑risk individuals.
By pairing the dose tables with a clear monitoring plan, you can keep the therapeutic benefits while steering clear of QT‑related complications.
Frequently Asked Questions
Can citalopram cause a heart attack?
Citalopram does not cause myocardial infarction directly. The concern is a prolonged QT interval, which can trigger arrhythmias that, in rare cases, lead to sudden cardiac death.
Is a QTc of 460 ms safe if the patient feels fine?
A QTc of 460 ms is above the typical safety threshold of 450 ms for women and 440 ms for men. Even without symptoms, you should reassess the dose, check electrolytes, and consider an alternative antidepressant.
Do all SSRIs affect the QT interval?
Most SSRIs have minimal QT impact. Fluoxetine, sertraline, and paroxetine generally stay within safe limits, while citalopram and escitalopram are the notable exceptions.
What if a patient is already on a QT‑prolonging antipsychotic?
Avoid stacking two QT‑prolonging agents if possible. If the antipsychotic can’t be changed, choose an antidepressant with the lowest QT effect (e.g., sertraline) and monitor closely.
How often should I repeat ECGs after starting therapy?
A follow‑up ECG at 1-2 weeks is standard for new starts or dose increases. If the initial QTc is near the safety cutoff, consider a repeat at 4 weeks as well.








13 Comments
Thanks for laying out the QT issue so clearly. It's easy to feel uneasy when you realize a common antidepressant can mess with the heart's rhythm. In practice I start everyone at the lowest effective dose and check electrolytes before titrating up. For older patients I usually stick to 10 mg of citalopram or 5 mg of escitalopram and get a baseline ECG. That way we keep the benefits while staying on the safe side.
The whole QT limit hype is just regulators trying to scare us off cheap meds.
When you stare at the numbers in those dose‑response tables, the reality of QT prolongation becomes hard to ignore.
Citalopram, being a racemic mixture, brings both the therapeutic S‑enantiomer and the less‑helpful R‑enantiomer into play, and the latter is a notorious contributor to hERG channel blockade.
Escitalopram, stripped down to the pure S‑form, appears kinder to the heart, yet it still nudges the QTc upward, especially when plasma levels climb.
The data show an average 8.5 ms increase at 20 mg of citalopram, which may seem trivial, but combine that with a potassium deficit and you’re flirting with a 60 ms jump.
A 60 ms jump is the red line that clinicians use to flag torsades risk, regardless of whether the absolute QTc sits at 470 ms or 490 ms.
Older adults often have reduced hepatic clearance, so a standard 40 mg dose can produce plasma concentrations akin to 60 mg in a younger person.
Add a macrolide antibiotic or an antipsychotic that also lingers on hERG, and the additive effect can push the QTc well beyond safe limits.
Regulators responded by slashing the permissible daily dose for patients over 65, but the reality is that even younger patients with comorbidities can hit dangerous thresholds.
In my clinic, I’ve seen a 52‑year‑old with normal labs develop a QTc of 512 ms after a rapid uptitration to 60 mg of citalopram while also being treated for an upper‑respiratory infection.
The patient experienced near‑syncope, and the subsequent ECG forced an immediate switch to sertraline, which has a much cleaner cardiac profile.
That case underscores why electrolyte monitoring-especially magnesium and potassium-is non‑negotiable when you push beyond 20 mg of citalopram.
The same vigilance applies to escitalopram, albeit the dose ceiling is lower and the QTc delta smaller, but the principle remains identical.
If you’re forced to stay on an SSRI for a patient with a baseline QTc of 460 ms, consider a non‑QT‑affecting agent like bupropion or a psychotherapy adjunct.
When you have to choose between the two, escitalopram typically offers the safer margin, but cost and insurance coverage can sway the decision.
Bottom line: dose, patient age, comorbid meds, and baseline ECG all intertwine, and ignoring any one of those variables is a recipe for preventable arrhythmia.
I agree with the cautious start‑low approach; it’s especially important for elders who metabolize slower.
A baseline ECG and electrolyte panel give us a safety net before we nudge the dose up.
Keeping the patient in the loop about potential palpitations also helps catch issues early.
Starting low saves lives. Keep an eye on the heart.
While the regulatory caps may feel restrictive, they’re based on solid signal‑to‑noise data across thousands of patients.
Ignoring them can lead to costly adverse events that outweigh any marginal cost savings.
A balanced view respects both safety and accessibility.
From a pharmacokinetic standpoint the hERG affinity of citalopram is dose‑proportional 📈 the QTc extension correlates with plasma Cmax ☂️ while escitalopram shows a flatter slope due to its enantiomeric purity 🧪 clinicians should therefore prioritize therapeutic drug monitoring when pushing >20 mg 🚦 and consider alternative SSRIs like sertraline with a more favorable cardiac safety profile 🛡️
Nice jargon parade but you’re glossing over the real‑world impact – patients don’t care about Cmax graphs, they care about a dizzy spell at the grocery store.
Your emoji‑filled safety checklist feels like a meme, not a clinical protocol.
We need hard‑nosed electrolyte checks and a real ECG, not just “monitor” buzzwords.
Otherwise the data you love will stay locked in papers while lives get risked.
Ah, the eternal dance between molecules and mortal hearts – as if our prescriptions aren’t already a Shakespearean tragedy waiting for a plot twist.
The regulators act like gatekeepers of the narrative, penning limits as if they could rewrite the very physics of ion channels.
Yet we, the humble prescribers, must navigate this labyrinth with nothing but stethoscopes and hope.
Perhaps the real lesson is that every pill carries a story, and sometimes the quiet ones whisper the loudest warnings.
Indeed, the metaphor works – the QT interval is the line that separates rhythm from chaos.
Practically, that means checking baseline QTc, adjusting dose, and avoiding polypharmacy whenever possible.
A simple protocol can keep the drama off the ECG.
Great reminders – a little vigilance goes a long way.
Keep the conversation open with patients and the outcomes will follow.
Dearest colleagues, whilst I appreciate the earnest optimism expressed, one must not be lulled into complacency by such rose‑tinted assurances – after all, the history of pharmacovigilance is replete with quiet catastrophes concealed beneath benign statistics. In other words, let’s keep our eyes peeled. Your patients deserve both scientific rigor and compassionate vigilance.
Remember, QT safety is a shared responsibility across the care team.
When you prescribe, think of the downstream cascade: pharmacy verification, nursing monitoring, and patient education all intersect at that single ECG readout.
A concise protocol might state “baseline ECG, electrolytes, dose ≤20 mg for ≥65 yo” but the reality of implementation requires dialog, reminders, and sometimes a gentle nudge to a colleague who missed the cue.
Embrace the habit of documenting the rationale in the chart – it not only satisfies regulatory audit trails but also reinforces a culture of transparency.
Finally, celebrate the small wins – a patient who tolerates therapy without arrhythmia is a testament to diligent, collaborative care.
Together we can keep the rhythm of treatment in harmony with cardiac safety.