
ACE Inhibitor & ARB Combination Checker
Check Your Medication Combination
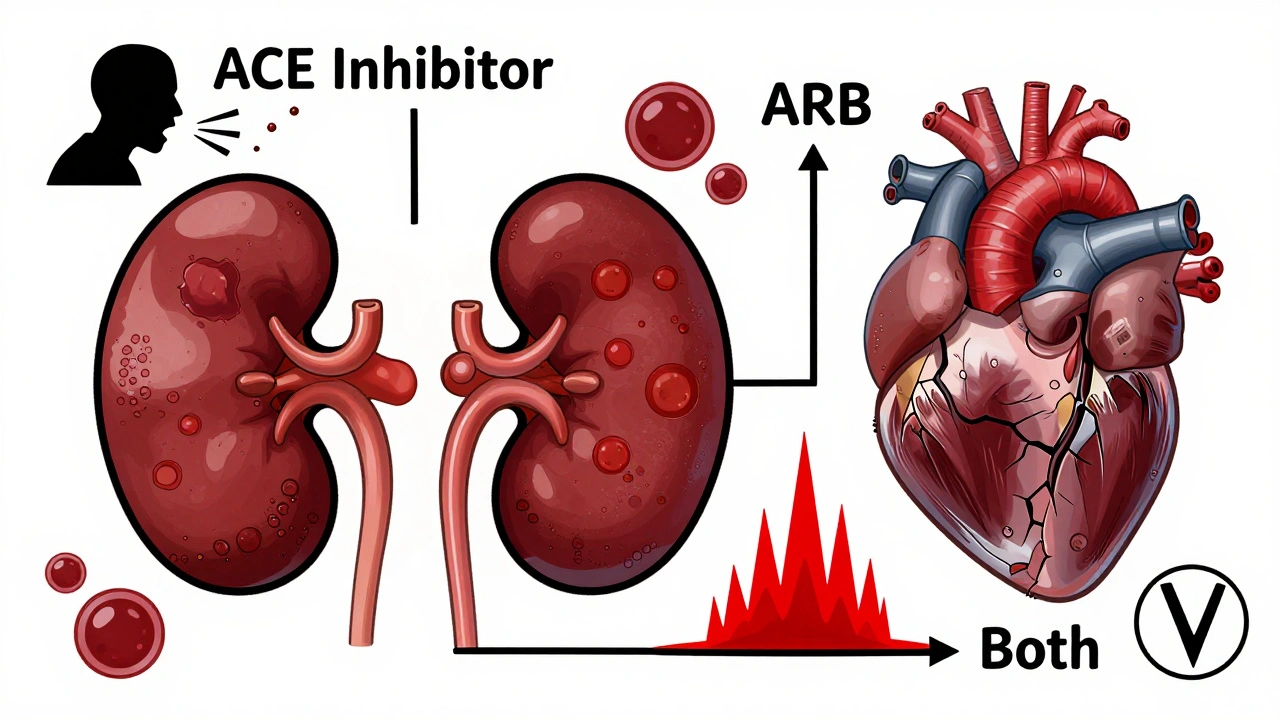
When you're taking medication for high blood pressure, heart failure, or kidney disease, you expect it to help-not hurt. But when it comes to ACE inhibitors and ARBs, mixing them can be dangerous, even if it seems logical. Both drugs target the same system in your body, the renin-angiotensin system, to lower blood pressure and protect your organs. But that doesn’t mean they work the same way-and combining them doesn’t make them better. In fact, it often makes things worse.
How ACE Inhibitors and ARBs Work (And Why It Matters)
ACE inhibitors like lisinopril, enalapril, and ramipril stop your body from making angiotensin II, a hormone that tightens blood vessels and raises blood pressure. They do this by blocking the enzyme that turns angiotensin I into angiotensin II. ARBs, such as losartan, valsartan, and irbesartan, take a different approach. Instead of stopping the production of angiotensin II, they block its receptors so the hormone can’t do its job.
At first glance, they sound like two paths to the same destination. But here’s the catch: ACE inhibitors cause bradykinin to build up in your body. That’s why about 1 in 10 people on these drugs get a dry, annoying cough. ARBs don’t do that. That’s why if you can’t tolerate an ACE inhibitor, your doctor will likely switch you to an ARB-not add one.
Another key difference? ACE inhibitors reduce angiotensin II everywhere, including at AT2 receptors, which may have protective effects on the heart and kidneys. ARBs only block AT1 receptors. That means angiotensin II can still act on AT2 receptors, which some researchers believe might be helpful long-term. But that doesn’t mean combining both drugs gives you the best of both worlds.
The Real Risk: Combining ACE Inhibitors and ARBs
It’s tempting to think that if one drug lowers blood pressure, two must lower it more. But that’s not how it works with these two classes. Multiple large studies-including the ONTARGET trial in 2008 and the VA NEPHRON-D trial in 2018-showed that using an ACE inhibitor and an ARB together doesn’t improve survival, reduce heart attacks, or protect the kidneys any better than using one alone.
What it does do? Double your risk of dangerous side effects.
- Hyperkalemia (high potassium): Risk jumps from 5% to over 10%. Severe cases can cause irregular heart rhythms-and even cardiac arrest.
- Acute kidney injury: Your kidneys may suddenly struggle to filter waste. This is especially risky if you’re older, have diabetes, or already have reduced kidney function.
- Dialysis-requiring kidney failure: In the ONTARGET trial, patients on both drugs were more than twice as likely to need dialysis compared to those on just an ACE inhibitor.
The FDA and major medical groups-including the American Heart Association, the American College of Cardiology, and the European Society of Cardiology-all say: Don’t combine them. Outside of rare, tightly monitored research settings, there’s no safe or proven benefit.
Why Do Some Doctors Still Try It?
Despite the clear warnings, a small number of doctors still consider combining ACE inhibitors and ARBs in specific cases. For example, in patients with non-diabetic kidney disease-like focal segmental glomerulosclerosis-who have proteinuria (excess protein in urine) above 1 gram per day, and who haven’t responded to maximum doses of an ACE inhibitor alone, some nephrologists might add an ARB.
But even then, it’s not done lightly. These patients need weekly blood tests for potassium and kidney function. They’re watched like hawks. And most doctors avoid it entirely. A 2023 survey of 317 primary care doctors found that 89% had stopped using this combination after the 2018 VA NEPHRON-D trial results came out. Only 11% still used it in rare cases-with monthly lab checks.
One Reddit thread from March 2024 had 142 medical residents sharing their experiences. Seventy-eight percent said they’d seen a patient hospitalized for hyperkalemia or kidney failure after being put on both drugs. That’s not an anomaly-it’s the rule.
Switching Between ACE Inhibitors and ARBs
If you’re switching from an ACE inhibitor to an ARB (or vice versa), don’t just swap them out. You need a washout period.
The Cleveland Clinic and other guidelines recommend waiting at least four weeks between stopping one and starting the other. Why? Because both drugs linger in your system, and overlapping them-even briefly-can spike your potassium or crash your kidney function. In real-world practice, though, only about 42% of prescribers follow this rule, according to a 2022 JAMA Internal Medicine study. That’s risky.
And if you’re switching because of a cough? That’s fine. But if you’re switching because your blood pressure isn’t controlled, don’t reach for the other drug. Talk about adding a diuretic, a calcium channel blocker, or a low-dose mineralocorticoid receptor antagonist like spironolactone. Those options are safer and proven to work.
Who Should Avoid These Drugs Altogether?
Not everyone can take ACE inhibitors or ARBs. Here’s who needs to be extra careful:
- Pregnant women: Both classes can cause severe birth defects. If you’re planning a pregnancy or think you might be pregnant, stop these drugs immediately and talk to your doctor.
- People with a history of angioedema: ACE inhibitors can trigger life-threatening swelling of the face, lips, or throat. If you’ve had this before-even once-you should never take an ACE inhibitor again. ARBs are safer, but still carry a small risk.
- Those with bilateral renal artery stenosis: Narrowed arteries to both kidneys can make these drugs dangerously reduce kidney function.
- Patients on aliskiren: This is a direct renin inhibitor. Combining it with ACE inhibitors or ARBs is officially contraindicated by the FDA after the ALTITUDE trial showed increased strokes and kidney failure.

Monitoring Is Non-Negotiable
If you’re on either an ACE inhibitor or an ARB, you need regular blood tests. Not just once. Not just when you feel off. Regularly.
Here’s what your doctor should check:
- Serum potassium: Aim to keep it between 3.5 and 5.0 mmol/L. Above 5.5 is dangerous.
- Serum creatinine: A rise of more than 30% from baseline in the first few weeks may mean your kidneys are struggling.
- eGFR: This estimates how well your kidneys are filtering. A drop of more than 15% in a month needs attention.
These tests should happen 1-2 weeks after starting the drug or changing the dose. After that, every 3 months if you’re stable. If you’re older, diabetic, or have kidney disease, check every 1-2 months.
What’s the Future Looking Like?
While ACE inhibitors and ARBs are still widely used, the focus is shifting. The market is growing, but not because of combinations. In 2023, ACE inhibitors accounted for 58% of new RAS blocker prescriptions in the U.S., and ARBs made up 42%. Lisinopril and losartan are the top two-simple, cheap, and effective.
Newer drugs are stealing the spotlight. Angiotensin receptor-neprilysin inhibitors (ARNIs), like sacubitril/valsartan (Entresto), are now first-line for heart failure with reduced ejection fraction. They’ve shown better survival rates than ACE inhibitors alone.
And there’s a new trial underway: the FINE-REWIND trial (2024-2028). It’s testing whether very low doses of both an ACE inhibitor and an ARB might be safe and helpful for diabetic kidney disease. But this is experimental. Don’t expect this to change guidelines anytime soon.
Bottom Line: Stick to One, Monitor Closely
ACE inhibitors and ARBs are powerful tools. But they’re not interchangeable, and they’re not meant to be combined. If you’re on one and it’s working, stay on it. If you’re having side effects like a cough or swelling, talk to your doctor about switching-not adding.
The goal isn’t to crush your blood pressure with two drugs. It’s to protect your heart and kidneys without putting your life at risk. That means choosing the right drug, taking it as prescribed, and getting your labs checked regularly.
Don’t let the idea of "more is better" lead you down a dangerous path. In this case, less is safer-and just as effective.
Can I take an ACE inhibitor and an ARB together for better blood pressure control?
No. Combining an ACE inhibitor with an ARB does not improve survival, heart attack prevention, or kidney protection. It doubles your risk of dangerous side effects like high potassium, acute kidney injury, and even dialysis-requiring kidney failure. Major guidelines from the AHA, ACC, and ESC strongly advise against this combination outside of rare research settings.
Why do ACE inhibitors cause a cough but ARBs don’t?
ACE inhibitors block the enzyme that breaks down bradykinin, a substance that can irritate the airways and cause a dry, persistent cough. ARBs don’t affect bradykinin levels, so they rarely cause this side effect. About 10-15% of people on ACE inhibitors get the cough; only 3-5% on ARBs do.
What should I do if I need stronger blood pressure control while on an ARB or ACE inhibitor?
Don’t add the other class. Instead, talk to your doctor about adding a diuretic (like hydrochlorothiazide), a calcium channel blocker (like amlodipine), or a low-dose mineralocorticoid receptor antagonist like spironolactone. These are safer, well-studied options that work well with RAS blockers without increasing kidney or potassium risks.
How often should I get blood tests if I’m on an ACE inhibitor or ARB?
Get your potassium and creatinine checked 1-2 weeks after starting the drug or changing the dose. If everything’s stable, check every 3 months. If you’re older, diabetic, or have kidney disease, check every 1-2 months. Skipping these tests can lead to undetected high potassium or kidney damage.
Are ARBs safer than ACE inhibitors overall?
ARBs have a better side effect profile-they cause less cough and slightly less angioedema. But they’re not safer in every way. Both can raise potassium and harm kidney function, especially in high-risk patients. ACE inhibitors have stronger evidence for reducing death in heart failure. The choice depends on your condition, side effects, and medical history-not just which one is "safer."
I was switched from an ACE inhibitor to an ARB because of a cough. How long should I wait before starting the new drug?
Wait at least four weeks after stopping the ACE inhibitor before starting the ARB. This reduces the risk of overlapping effects that can spike potassium or damage your kidneys. Many doctors skip this step, but following it is safer-especially if you have diabetes or kidney disease.








8 Comments
Really glad someone laid this out so clearly. I’ve seen too many patients get mixed up on this-especially when they’re googling ‘better BP control’ and end up on both meds. One guy ended up in the ER with potassium at 6.8. Scary stuff. Stick to one, monitor, and don’t overcomplicate it.
⚠️ WARNING: Combining ACEi + ARB is NOT ‘off-label’-it’s a CLASS III CONTRAINDICATION per ACC/AHA/ESC guidelines. 📉 2.1x higher risk of dialysis. 📈 10.4% hyperkalemia vs 4.8% monotherapy. 📊 VA NEPHRON-D: p<0.001. Don’t be the doctor who ‘thinks they know better.’
i just wanted to say thank you for writing this. my dad was on lisinopril for years and got the cough so bad he couldn’t sleep. switching to losartan changed his life. i didn’t know about the 4-week washout though… my dr just switched him right away. i’m gonna call and ask if we should wait now. 🙏
Great breakdown. One thing I’d add: even when switching from ACEi to ARB due to cough, the bradykinin clearance isn’t instant. That 4-week washout isn’t just bureaucracy-it’s pharmacokinetics. Also, ARBs aren’t ‘safer’ across the board. In HFrEF, ACEi still have slightly better mortality data. Choice depends on the patient, not the drug label.
People who say ‘but my doctor prescribed it’ are just trusting someone who shouldn’t be prescribing. This isn’t a gray area. It’s a black-and-white guideline violation. If your doctor is still doing this, find a new one. No exceptions. Not even for ‘rare cases.’
From India: In rural clinics, we still see this combo prescribed due to lack of guidelines awareness. Many patients are on both because they ‘feel better’-but labs show rising creatinine. Need more education. Thank you for this clear summary. 🙏
I’ve been reading up on this because my aunt was hospitalized last year after being put on both drugs for ‘resistant hypertension’-she ended up with AKI and had to be dialyzed for a week. I dug into the ONTARGET trial and found that the increased risk of renal failure was statistically significant even after adjusting for age, diabetes, and baseline eGFR. The 2018 VA NEPHRON-D paper showed that the combination didn’t reduce proteinuria any better than monotherapy in diabetic nephropathy, but doubled the rate of hyperkalemia requiring hospitalization. And here’s the kicker: in patients over 75, the risk of acute kidney injury was 3.2 times higher. I also checked the 2023 survey of primary care docs-89% had stopped the combo, but in my aunt’s case, her cardiologist was still using it because he’d ‘seen success’ in the 90s. That’s the problem. Guidelines evolve, but old habits die hard. Even worse, some patients are told to ‘just keep taking both until the doctor says otherwise’-but they never follow up. No labs, no monitoring. Just hoping it works. That’s how people end up in the ICU. We need better patient education, not just doctor education. The fact that only 42% of prescribers follow the 4-week washout rule is terrifying. And don’t get me started on how many patients are still on aliskiren with an ACEi or ARB. The ALTITUDE trial was a disaster. We’re still seeing this in practice. It’s not just about knowing the guidelines-it’s about enforcing them. And patients need to be their own advocates. If your doctor says ‘it’s fine,’ ask for the evidence. Show them the VA NEPHRON-D paper. Ask for the potassium and creatinine results. Don’t let ‘I’ve always done it this way’ be an answer.
Wow, another anti-combo lecture. Newsflash: guidelines are written by committees, not patients. My uncle’s kidney function improved on both drugs. He’s been stable for 3 years. Maybe your data doesn’t fit every real-world case?