High cholesterol isn’t something you feel. No chest pain. No dizziness. No warning signs. That’s why it’s so dangerous. By the time symptoms show up-like a heart attack or stroke-it’s often too late. Hypercholesterolemia, the medical term for high cholesterol, quietly builds up in your arteries for years, silently increasing your risk of heart disease, the number one killer worldwide.
What Exactly Is Hypercholesterolemia?
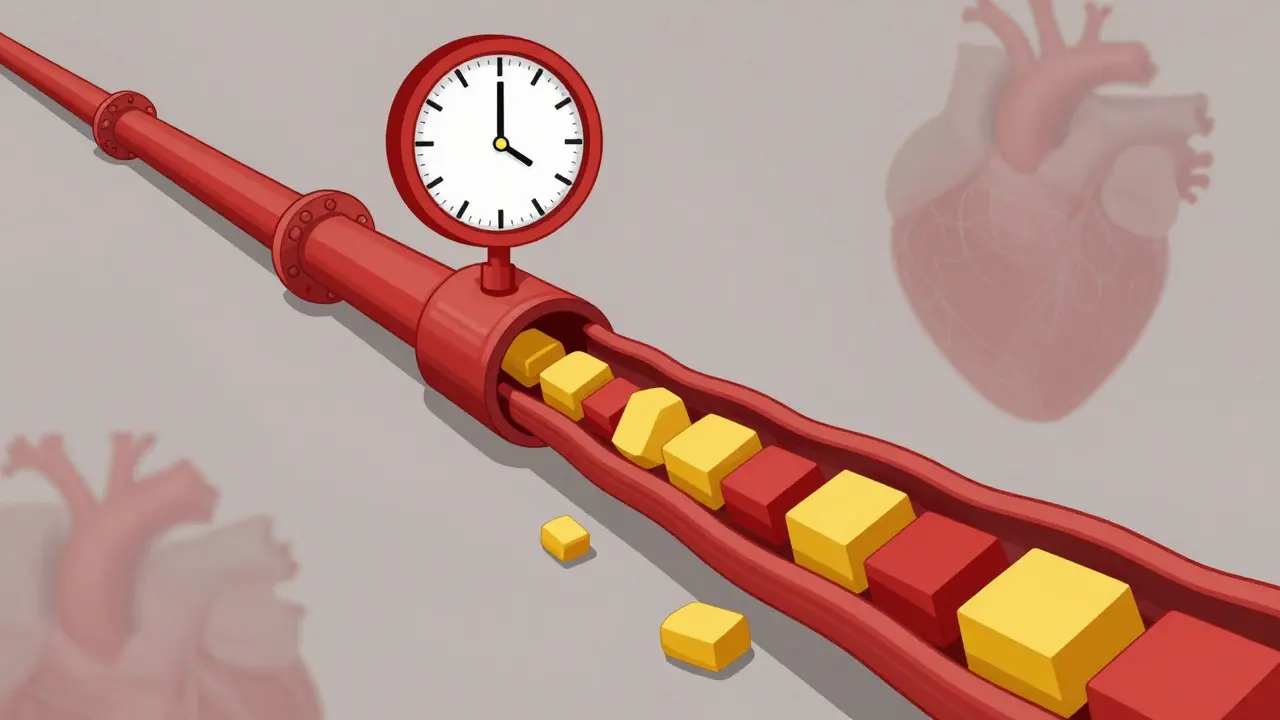
Hypercholesterolemia means your blood has too much cholesterol-specifically too much LDL, the so-called "bad" cholesterol. Cholesterol isn’t all bad. Your body needs it to build cells, make hormones, and digest food. But when LDL levels climb too high, it sticks to your artery walls, forming plaque. Over time, that plaque narrows your arteries, restricting blood flow to your heart and brain.
The American Heart Association says about 93 million American adults have total cholesterol above 200 mg/dL. But it’s not just the number that matters-it’s the type. LDL cholesterol should ideally be under 100 mg/dL. Levels above 160 mg/dL are considered high, and above 190 mg/dL are classified as severe. At that point, it’s often not just about diet or lifestyle-it could be genetics.
Familial Hypercholesterolemia: It’s Not Just Bad Habits
Many people think high cholesterol is just from eating too much butter or fried food. That’s true for some-but not all. About 1 in 250 people have a genetic condition called familial hypercholesterolemia (FH). This isn’t something you develop. You’re born with it.
If you have heterozygous FH (one faulty gene from a parent), your LDL levels are typically above 190 mg/dL from childhood. If you have homozygous FH (two faulty genes), levels can soar past 450 mg/dL. These people aren’t eating poorly-they’re genetically wired to process cholesterol incorrectly. Their bodies can’t remove LDL from the blood properly because of mutations in the LDLR or PCSK9 genes.
Without treatment, people with FH have a 20 times higher risk of heart disease before age 40. Some suffer heart attacks in their teens or twenties. Physical signs like yellowish fatty bumps on the eyelids (xanthelasmas) or thickened tendons in the heels (tendon xanthomas) are red flags. If you see these, get tested-even if you’re young and feel fine.
What Causes High Cholesterol Besides Genetics?
Not everyone with high cholesterol has FH. For most, it’s secondary-caused by other factors:
- Diabetes: About 68% of people with type 2 diabetes have abnormal cholesterol levels. High blood sugar damages blood vessels and lowers "good" HDL while raising LDL and triglycerides.
- Hypothyroidism: When your thyroid doesn’t make enough hormones, your liver can’t clear cholesterol efficiently. Up to 20% of hypercholesterolemia cases link back to an underactive thyroid.
- Chronic kidney disease: People on dialysis often have cholesterol levels above 240 mg/dL. The kidneys help regulate fat metabolism, and when they fail, cholesterol builds up.
- Medications: Some blood pressure pills (like thiazide diuretics), steroids, and certain antivirals can raise LDL by 10-15%.
- Obesity and inactivity: Excess weight, especially around the waist, lowers HDL and raises triglycerides. Lack of movement slows down your body’s ability to process fats.
Even if you’re eating healthy, these hidden causes can still push your numbers up. That’s why testing is critical-not just for those who eat burgers daily, but for anyone with risk factors.
How Is It Diagnosed?
The only way to know your cholesterol levels is through a simple blood test called a lipid panel. You no longer need to fast before the test. The U.S. Preventive Services Task Force recommends screening for all adults between 40 and 75. But if you have a family history of early heart disease, or you’re under 40 with risk factors like obesity or diabetes, get tested earlier.
The test measures:
- Total cholesterol
- LDL (bad cholesterol)
- HDL (good cholesterol)
- Triglycerides
Doctors use these numbers along with your age, blood pressure, smoking status, and whether you have diabetes to calculate your 10-year risk of a heart attack or stroke. If your risk is high, even a moderate LDL level might need treatment.
Treatment: It’s Not Just About Statins
For most people, the first step is lifestyle changes: eating more fiber, cutting out trans fats, moving more, and losing weight. The Portfolio Diet-rich in plant sterols, oats, nuts, and soy-can lower LDL by 10-15% in a few months, according to JAMA Cardiology studies.
But if your LDL is above 190 mg/dL, or you have FH or other heart disease risks, lifestyle alone won’t cut it. That’s where medication comes in.
Statins are the first-line treatment. Drugs like atorvastatin and rosuvastatin can slash LDL by 50% or more. They’re safe, affordable, and proven to prevent heart attacks. But about 1 in 5 people can’t tolerate them due to muscle pain or other side effects.
For those who can’t take statins, or need extra help, there are other options:
- Ezetimibe: Blocks cholesterol absorption in the gut. Lowers LDL by about 18%.
- PCSK9 inhibitors: Injectables like alirocumab and evolocumab that help the liver remove more LDL. They can lower LDL by another 50-60% on top of statins.
- Inclisiran (Leqvio): A newer shot given just twice a year. It works at the genetic level to reduce LDL production. Approved in 2021, it’s a game-changer for people who struggle with daily pills.
People with FH often need a triple combo: a high-dose statin, ezetimibe, and a PCSK9 inhibitor just to reach target levels. It’s not ideal-but it’s life-saving.
Why So Many People Still Don’t Get Treated
Here’s the scary part: even though we have effective treatments, most people with high cholesterol aren’t getting them. Only about 55% of eligible U.S. adults are on statins. Among Black adults, the rate drops to 42%. Women are less likely to be prescribed medication than men, even when their risk is equal.
Why? Some people don’t feel sick, so they don’t think they need medicine. Others can’t afford it. Some fear side effects. And many doctors don’t push hard enough-especially for younger patients or women.
Adherence is another problem. Half of people stop taking their statins within a year. But skipping doses doesn’t just mean your cholesterol goes up-it means your risk of a heart attack goes up too.
The Big Picture: Cost, Impact, and the Future
High cholesterol isn’t just a personal health issue-it’s a public health crisis. In the U.S., heart disease linked to high cholesterol costs $218 billion a year. That’s $142 billion in medical bills and $76 billion in lost work and productivity.
Pharmaceutical companies made $14.3 billion selling statins in 2022. Newer drugs like PCSK9 inhibitors brought in $1.8 billion, but they’re expensive-around $14,000 a year. That’s why they’re usually reserved for high-risk patients.
The future is moving toward personalized care. Doctors are now using genetic tests to identify polygenic hypercholesterolemia-where many small gene variants add up to high cholesterol. This helps target treatment earlier, even before LDL hits 190 mg/dL.
But the biggest threat ahead? Obesity. By 2030, half of U.S. adults could be obese. That means more diabetes, more high cholesterol, and more heart disease. The American Heart Association’s goal is to improve cardiovascular health by 20% by 2030. That means better access to testing, affordable meds, and real support for healthy eating-not just advice.
What You Can Do Today
If you’ve never had your cholesterol checked, make an appointment. Don’t wait for symptoms. Don’t assume you’re too young or too healthy.
If you’ve been told you have high cholesterol:
- Ask if you have familial hypercholesterolemia-especially if a close relative had a heart attack before age 55.
- Get a full lipid panel, not just total cholesterol.
- Don’t ignore medication if your doctor recommends it. Statins aren’t perfect, but they save lives.
- Pair meds with real food changes: swap butter for olive oil, white bread for oats, soda for water.
- Move daily-even a 30-minute walk helps.
High cholesterol is silent. But you don’t have to be. Knowing your numbers, asking the right questions, and sticking with treatment can mean the difference between a long, healthy life and a preventable tragedy.
Can high cholesterol be reversed without medication?
For some people with mild, diet-related high cholesterol, yes-especially if caught early. Losing weight, cutting out trans fats, eating more fiber (oats, beans, vegetables), and exercising can lower LDL by 10-15%. But if your LDL is above 190 mg/dL, or you have a family history of early heart disease, lifestyle changes alone usually aren’t enough. Genetics play a bigger role than most people realize.
Is familial hypercholesterolemia rare?
It’s not rare-it’s underdiagnosed. About 1 in 250 people have heterozygous familial hypercholesterolemia. That means in a city of 500,000, around 2,000 people have it. Yet less than 10% are diagnosed. Many are told they’re just "eating too much fat" when they actually have a genetic disorder that needs specific treatment.
Do I need to fast before a cholesterol test?
No, you don’t. Guidelines from the National Lipid Association and the American Heart Association now say fasting isn’t required for standard lipid panels. Non-fasting tests give accurate readings for total cholesterol, HDL, and LDL. Fasting was once standard, but research shows it doesn’t improve accuracy for most people-and makes testing harder.
Are statins safe for long-term use?
Yes, for most people. Statins have been used for over 30 years, and large studies involving millions of patients show they’re safe over decades. The most common side effect is mild muscle soreness, which affects about 1 in 10 people. Serious side effects like liver damage or muscle breakdown are extremely rare. The benefit-reducing your risk of heart attack or stroke by up to 30%-far outweighs the risks for high-risk individuals.
Can I stop taking cholesterol medication if my levels improve?
Usually not. High cholesterol is a chronic condition, not a one-time problem. Even if your numbers drop with medication and lifestyle changes, stopping the drug often causes levels to rise again within weeks. Think of it like high blood pressure or diabetes-you manage it daily. Stopping medication without your doctor’s guidance increases your risk of heart disease.
Does dietary cholesterol (like eggs) raise blood cholesterol?
For most people, dietary cholesterol has a small effect. The bigger issue is saturated and trans fats, which have a much stronger impact on LDL levels. That’s why the Dietary Guidelines removed the 300 mg daily limit on cholesterol. But a 2019 JAMA study found that every extra 300 mg of cholesterol per day (about 1.5 eggs) was linked to a 17% higher risk of heart disease. So while eggs aren’t the enemy, eating a dozen a week isn’t smart if you already have high cholesterol.





13 Comments
My dad had LDL over 200 since he was 30 and never ate fast food. Got diagnosed with FH at 45 after his first angioplasty. Turns out his dad died of a heart attack at 38. No one talked about it back then. If we’d known, he could’ve been on statins in his 20s. Why do we wait for crises to act?
It is an undeniable fact that the American medical establishment has, through decades of flawed dietary dogma, misattributed the root cause of cardiovascular pathology to cholesterol intake rather than systemic insulin dysregulation and industrialized fat consumption. The entire lipid hypothesis is a construct of pharmaceutical influence and outdated epidemiology.
Wait so if you have FH and your LDL is 250 at 18, you’re basically ticking a time bomb? And the only way to slow it down is stacking statins + ezetimibe + PCSK9 inhibitors? That’s wild. I had no idea it was this extreme. My cousin was diagnosed at 22 and now she’s on three meds. She says she feels fine but has to get blood work every 3 months. That’s insane.
Get tested. Don’t wait. Statins work. Stick with them.
It’s not optional if your numbers are high.
In India we don’t talk about this enough. My uncle had heart attack at 42. Everyone said he ate too much ghee. But his sister and his son both have LDL over 200 too. No one ever tested them. We think it’s just food. It’s not. It’s genes.
One must acknowledge the profound institutional inertia that perpetuates the myth of cholesterol as a singular villain. The conflation of correlation with causation, the commodification of lipid-lowering pharmaceuticals, and the systemic neglect of metabolic syndrome as the true driver of atherosclerosis-these are not oversights. They are failures of epistemic integrity.
My doc put me on a statin after my lipid panel came back at 210. I was scared at first. But after six months, I feel better than ever. Energy up, no brain fog. And I didn’t even change my diet that much. Just swapped white rice for quinoa and started walking after dinner. It’s not magic. It’s medicine working.
It is both tragic and deeply predictable that the American populace continues to abdicate responsibility for its own biological integrity, outsourcing health to the pharmaceutical-industrial complex while clinging to the delusion that bacon is a benign indulgence. One cannot out-eat a genetic predisposition, nor can one out-purchase a lifetime of metabolic negligence.
I used to think cholesterol was just about eggs and butter. Then my mom got diagnosed with FH after her stroke. She was 54. She never ate fried food. She walked every day. But her numbers were through the roof since she was a teen. Now she’s on inclisiran. Two shots a year. Life changed. I got tested last month. My LDL was 198. I’m starting statins next week. Better late than never.
I’m 32, female, active, eat clean. My LDL was 185. My doctor said ‘maybe try diet first.’ I did for six months. No change. Then I asked for a genetic test. Turned out I had FH. I started statins. My LDL is now 82. I feel like an idiot for waiting. Don’t let anyone tell you it’s ‘just a number.’ It’s your future.
Everyone thinks cholesterol is about fat but no one talks about the real villain-soybean oil. It’s everywhere. In your salad dressing, your chips, your ‘healthy’ snacks. It’s inflammatory, it wrecks your liver, and it’s the real reason LDL skyrockets. Stop blaming butter. Blame Big Ag.
My brother had a heart attack at 28. Turned out he had homozygous FH. LDL was 510. He’s on a triple combo now. Gets a PCSK9 shot every two weeks. He’s alive because he got diagnosed early. I got tested. My LDL was 188. I started ezetimibe. No side effects. I don’t feel different but I know I’m doing something. My kids are getting tested next month. This isn’t just about me.
So let me get this straight. You’re telling me that if I’m a 40-year-old guy who eats a burger once a week and runs 5Ks but my LDL is 205, I’m basically a ticking time bomb because of genes, not lifestyle? And if I don’t take a pill every day, I’m just gambling with my life? Cool. Thanks for the guilt trip.