
Every year, half a million people in the U.S. get sick from a bacteria most of us have never heard of: C. difficile. It doesn’t come from bad food or dirty water. It comes from something most people think is harmless-antibiotics. When antibiotics wipe out the good bacteria in your gut, C. difficile takes over. It causes severe diarrhea, stomach pain, and in the worst cases, colon rupture or death. For many, standard treatments fail. But there’s a surprising solution: a fecal transplant.
How Antibiotics Trigger C. difficile Infection
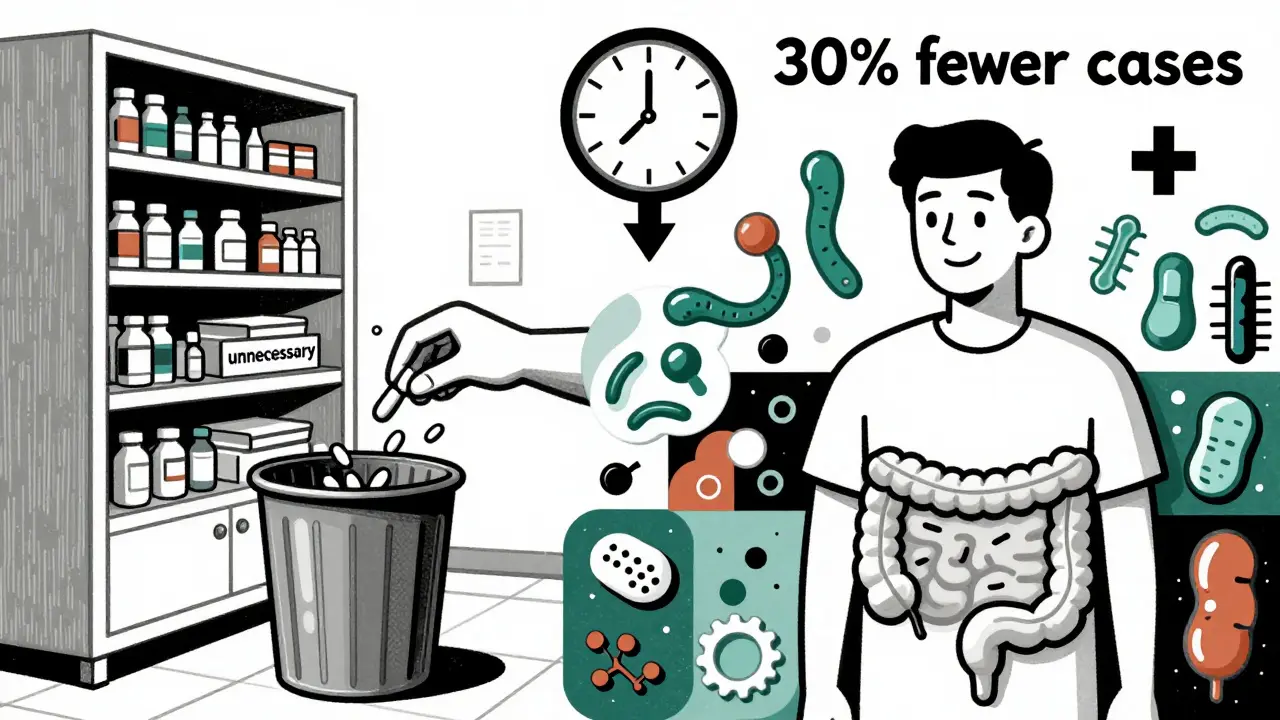
Antibiotics are lifesavers. But they don’t discriminate. When you take them for a sinus infection, a urinary tract infection, or even a dental procedure, they don’t just kill the bad bugs-they also wipe out the trillions of good bacteria that live in your gut. These good bacteria keep harmful ones like C. difficile in check. Once they’re gone, C. difficile multiplies fast, releasing toxins that attack the colon lining. The result? Diarrhea that won’t quit, fever, and intense abdominal cramping.
Not all antibiotics carry the same risk. Some are far more dangerous than others. Research shows that clindamycin, later-generation cephalosporins like ceftriaxone, and fluoroquinolones like ciprofloxacin are the biggest culprits. But one of the most surprising findings? Piperacillin-tazobactam-a common hospital antibiotic-has the highest risk of all. A 2023 study of over 33,000 hospital patients found that this drug nearly doubled the chance of getting C. difficile compared to other antibiotics. Even more telling: every extra day on antibiotics increases your risk by 8%. After 14 days, the danger spikes again.
It’s not just about which antibiotic you take-it’s how long you take it. The CDC and other health agencies now push for something called “antibiotic stewardship.” That means doctors should ask: Do we really need this? Can we use something narrower? Can we stop sooner? Studies show that cutting antibiotic use by even a few days can drop C. difficile cases by 30% in hospitals.
Why Recurrent Infections Are So Hard to Beat
Many people think once the diarrhea stops, the infection is gone. But that’s not true. About 20% of patients get it again after treatment. And for 1 in 5 of those, it comes back a second or third time. Each recurrence gets harder to treat. Vancomycin, the go-to drug for years, works for the first infection-but fails more often with each return. Why? Because it doesn’t fix the broken gut ecosystem. It just temporarily suppresses the bacteria.
People who’ve had multiple recurrences often describe the same story: they’re on antibiotics for weeks, feel better for a few days, then the diarrhea comes back worse than before. Some try probiotics. But studies show most probiotics don’t help-and in vulnerable patients, they can even cause dangerous infections. The Cleveland Clinic says for some, simply stopping the antibiotic is enough. Their gut recovers on its own. But for others, nothing works until they try something radical.

The Fecal Transplant Revolution
Imagine taking a stool sample from a healthy person and putting it into someone with C. difficile. It sounds bizarre. But it’s one of the most effective treatments we have.
The first major proof came in 2013, when researchers in the New England Journal of Medicine compared standard vancomycin treatment to fecal microbiota transplantation (FMT). The results were shocking: 94% of patients who got the transplant were cured after one or two treatments. Only 31% of those on vancomycin were. Since then, dozens of studies have confirmed this. Today, FMT cures 85% to 90% of recurrent C. difficile cases.
How does it work? It’s not magic. It’s ecology. The healthy donor’s stool contains hundreds of different bacterial strains that crowd out C. difficile, restore balance, and rebuild the gut’s natural defenses. The transplant isn’t about adding “good bacteria”-it’s about bringing back the whole community.
There are three main ways to deliver it: through a colonoscopy (most common), an enema, or oral capsules. Capsules are becoming more popular because they’re less invasive and easier to store. In 2022 and 2023, the FDA approved two standardized, frozen stool products-Rebyota and Vonjo-making FMT more like a medicine than a procedure. These are not DIY experiments. They’re rigorously screened, tested for viruses and drug-resistant bugs, and produced under strict guidelines.
Who Gets FMT-and Who Doesn’t
FMT isn’t for everyone. Guidelines from the American Gastroenterological Association say it’s recommended for people who’ve had three or more C. difficile infections. It’s also used when standard treatments fail, even after just two recurrences. But it’s not a first-line option. Doctors still try fidaxomicin (a more targeted antibiotic) or add bezlotoxumab (a monoclonal antibody that neutralizes one of the toxins). These reduce recurrence by about 10%.
There are risks. FMT can cause temporary bloating, cramps, or fever. Rarely, it can transmit infections if donor screening fails. That’s why all approved products use donors who undergo extensive testing-for HIV, hepatitis, E. coli, and even antibiotic-resistant strains. Long-term effects? Still being studied. Some researchers worry about weight gain, allergies, or even mood changes linked to microbiome shifts. But for someone who’s been hospitalized five times with C. difficile, the benefits far outweigh the unknowns.
The Hidden Burden: Community Cases Are Rising
For years, people thought C. difficile was only a hospital problem. That’s changed. Since 2011, community cases have grown by 14% every year. More than half of new infections now happen outside hospitals. Why? Because antibiotics are overused everywhere-doctors prescribe them for viral colds, pet owners give them to animals, and patients demand them. A 2023 study found nearly half of community C. difficile patients had taken antibiotics within the last 30 days.
Even scarier: some people carry C. difficile without symptoms. These silent carriers can spread it to others. Antibiotics don’t just make them sick-they can trigger outbreaks. That’s why experts say we need smarter antibiotic use not just in hospitals, but in clinics, nursing homes, and pharmacies.
What’s Next: Beyond the Stool
Scientists are already working on the next generation of treatments. One promising option is SER-109, an oral pill made of purified bacterial spores from healthy donors. In a 2022 trial, it cured 88% of recurrent cases-almost as good as FMT. Other companies are developing synthetic microbiome therapies, engineered to target C. difficile without introducing whole stool. The goal? A treatment as precise as a drug, without the “yuck factor.”
Cost is also a factor. A single FMT procedure can cost $1,500 to $3,000. But a hospital stay for recurrent C. difficile averages $11,000. Insurance now covers FMT for recurrent cases, and the new FDA-approved products are becoming more widely available. The market for these therapies is expected to hit $250 million by 2027.
By 2030, experts predict a 30% drop in C. difficile cases thanks to better antibiotic rules and new microbiome treatments. But until then, the simplest defense remains the most powerful: don’t take antibiotics unless you absolutely need them. And if you do, ask your doctor: Is this the right one? How long do I really need it?
Can you get C. difficile without taking antibiotics?
Yes, but it’s rare. Most cases are linked to recent antibiotic use. However, about 1 in 5 infections now happen in people who haven’t taken antibiotics in the past month. These are called community-associated cases. They often occur in people with weakened immune systems, recent hospital visits, or exposure to someone with C. difficile. Even healthy people can carry the bacteria without symptoms and spread it.
Is a fecal transplant safe?
When done through approved methods, yes. FDA-approved products like Rebyota and Vonjo come from donors screened for over 50 infectious agents, including HIV, hepatitis, and drug-resistant bacteria. The risk of serious infection from these products is extremely low. Unregulated, homemade transplants carry higher risks. Always choose a medically supervised procedure. Side effects like bloating or mild fever are common but temporary.
Why not just use probiotics instead of FMT?
Most probiotics don’t work for C. difficile. Studies show they offer little to no protection against infection or recurrence. Some even increase the risk of bloodstream infections in people with weak immune systems. FMT works because it restores the entire gut ecosystem-not just one or two strains. Probiotics are like adding a few trees to a burned forest. FMT replants the whole forest.
How long does it take to recover after a fecal transplant?
Many patients notice improvement within 24 to 48 hours. Diarrhea usually stops within a few days. Full gut recovery takes longer-weeks to months-as the new bacteria establish themselves. Most people report feeling like themselves again within a week. Follow-up testing isn’t usually needed unless symptoms return.
Can C. difficile come back after a successful transplant?
Yes, but it’s uncommon. About 10% to 15% of people who get FMT experience another episode, usually if they take antibiotics again afterward. That’s why doctors advise avoiding unnecessary antibiotics for at least 3 to 6 months after the transplant. In rare cases, the new microbiome doesn’t fully take hold, or the person is re-exposed to the bacteria. But recurrence after FMT is far less common than after antibiotic treatment alone.








