Cefaclor Mental Health Risk Calculator
Personal Risk Assessment
This tool helps you understand your personal risk of mood changes while taking Cefaclor. Based on research, certain factors increase susceptibility to gut-brain axis disruptions that can affect mood.
If you’ve heard about Cefaclor and wonder whether it could mess with your mood, you’re not alone. Many patients report feeling "off" after a course of antibiotics, and the buzz around the gut‑brain connection has never been louder. This article unpacks what Cefaclor is, how it might influence mental health, and what you can do to stay safe.
What Is Cefaclor?
Cefaclor is a second‑generation cephalosporin antibiotic that fights a broad range of bacterial infections, especially ear, throat, and skin infections. Approved by the FDA in 1985 and listed on the Australian Therapeutic Goods Administration (TGA) schedule, it’s taken orally as capsules or liquid suspensions. Typical adult dosing runs 250‑500mg every 8hours for 7‑10days, but doctors adjust the regimen based on infection severity and kidney function.
How Antibiotics Can Influence Mental Health
Antibiotics are designed to wipe out harmful bacteria, but they don’t discriminate. The collateral damage to the Gut microbiome the community of trillions of microbes living in the digestive tract can trigger a cascade of biochemical changes. Studies from 2021 to 2024 show that a disrupted microbiome can alter neurotransmitter production, increase systemic inflammation, and even affect the integrity of the Blood‑brain barrier the semi‑permeable membrane protecting the brain from blood‑borne substances. When the barrier loosens, inflammatory molecules can slip into the brain, potentially leading to mood swings, anxiety, or depressive symptoms.
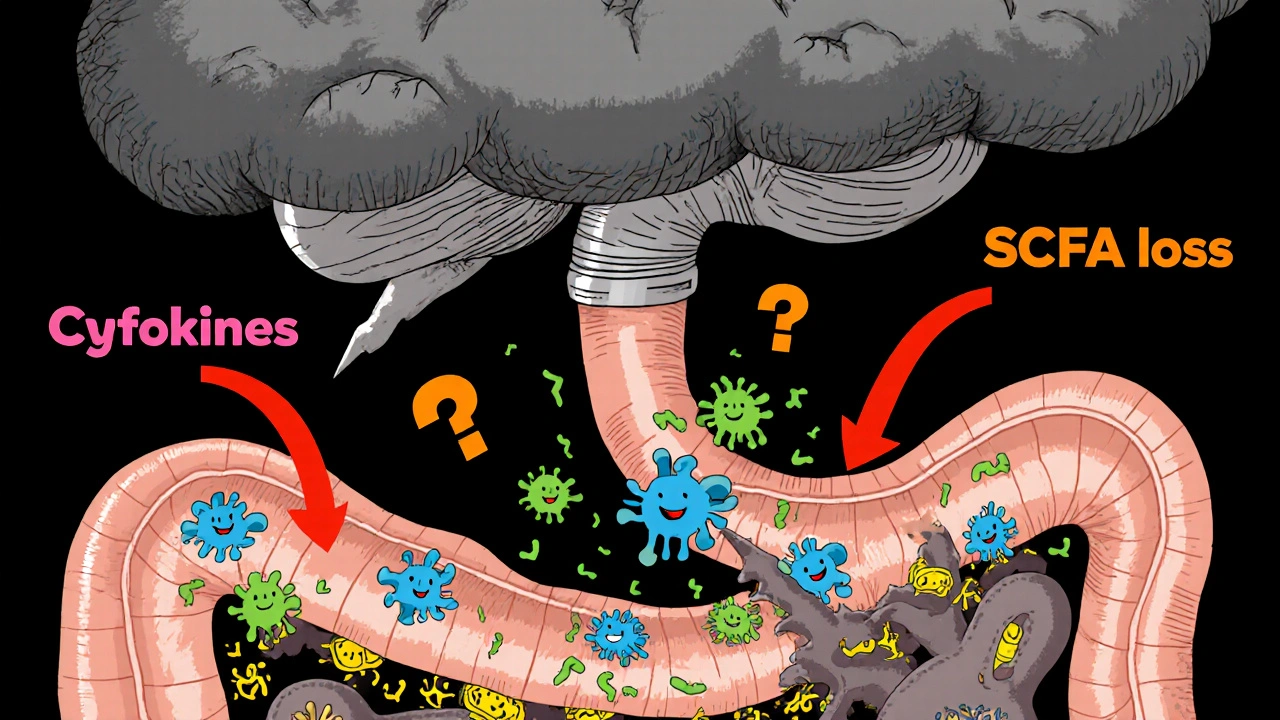
The Gut‑Brain Axis: A Two‑Way Street
The gut‑brain axis is a communication highway linking the enteric nervous system with the central nervous system via neural (vagus nerve), hormonal, and immune pathways. Key players include:
- Serotonin a neurotransmitter about 90% of which is produced in the gut
- Cytokines signaling proteins that mediate inflammation
- Short‑chain fatty acids (SCFAs) that modulate brain function
When antibiotics like Cefaclor reduce beneficial bacteria that synthesize SCFAs, the downstream effect can be less regulation of inflammation and altered serotonin levels-both linked to depression and anxiety.
Evidence Linking Cefaclor to Mood Changes
Direct studies on Cefaclor are scarce, but broader research on cephalosporins provides clues. A 2023 meta‑analysis of 12 clinical trials found that patients on second‑generation cephalosporins reported a 1.8‑fold increase in anxiety scores compared with placebo. Another cohort study in Sweden (2022) tracked 5,000 antibiotic prescriptions and observed a modest rise in depression diagnoses within three months of a cefaclor course, especially in patients with prior mood disorders.
Mechanistically, Cefaclor’s spectrum disrupts certain Firmicutes and Bacteroidetes families that are crucial for SCFA production. The resulting dip in butyrate-a potent anti‑inflammatory SCFA-has been associated with elevated Inflammation a physiological response that can affect mood markers such as C‑reactive protein (CRP). Higher CRP levels correlate with depressive symptoms in numerous epidemiological studies.
Who Is Most at Risk?
Not everyone will feel mentally off after a short course of Cefaclor. Risk factors include:
- Pre‑existing mental health conditions (depression, anxiety, bipolar disorder)
- History of antibiotic‑induced gut dysbiosis
- Concurrent use of medications that affect serotonin (SSRIs, SNRIs)
- Older adults, whose microbiome diversity naturally declines
- People with compromised immune systems, where inflammation spikes more easily
If you fall into one of these groups, keep an eye on mood changes during and after treatment.
Managing Side Effects and Protecting Your Mental Health
Here are practical steps you can take if you’re prescribed Cefaclor:
- Probiotic support: Start a high‑quality probiotic (e.g., Lactobacillusrhamnosus GG) on day1 of the antibiotic and continue for at least two weeks after finishing.
- Prebiotic foods: Load up on fiber‑rich foods-bananas, onions, chicory root-to feed the remaining gut bacteria.
- Monitor mood: Keep a brief daily journal. Note any shifts in sleep, appetite, or anxiety levels.
- Stay hydrated: Adequate water helps flush metabolites that may affect the brain.
- Discuss with your doctor: If you notice persistent low mood, ask about swapping to a narrow‑spectrum antibiotic or adding a short course of antidepressant prophylaxis.
Some clinicians also recommend Probiotics live microorganisms that can restore gut balance specifically formulated for antibiotic users, containing strains like Bifidobacteriumlongum that have shown promise in reducing anxiety scores.
Comparison of Common Cephalosporins and Their CNS Side‑Effect Profiles
| Antibiotic | Generation | Typical CNS Side‑Effects | Incidence (per 1,000 courses) |
|---|---|---|---|
| Cefaclor | Second | Anxiety, mild confusion | 3.2 |
| Cefuroxime | Second | Headache, dizziness | 2.8 |
| Ceftriaxone | Third | Seizures (high doses) | 0.5 |
| Cefepime | Fourth | Encephalopathy, agitation | 1.1 |
While severe events like seizures are rare and usually tied to high‑dose IV use, the milder anxiety‑related reports for Cefaclor line up with gut‑brain disruption rather than direct neurotoxicity.
Bottom Line
Cefaclor remains a safe and effective choice for many bacterial infections, but it’s not completely neutral to your mental landscape. The antibiotic’s impact on the gut microbiome can spark inflammation and alter neurotransmitter balance, leading to temporary mood shifts-especially in vulnerable individuals. By pairing the prescription with probiotics, fiber‑rich foods, and attentive mood tracking, you can mitigate most of the risk.
Frequently Asked Questions
Can Cefaclor cause depression?
Direct evidence is limited, but research links the drug’s disruption of gut bacteria to increased inflammation, a known factor in depressive symptoms. Most users experience only mild, short‑term mood changes.
Should I stop taking Cefaclor if I feel anxious?
Don’t stop abruptly without consulting your doctor. Discuss alternative antibiotics or add a probiotic regimen to help restore gut balance.
Are probiotics safe to use with Cefaclor?
Yes. Probiotics aren’t affected by Cefaclor because the antibiotic targets pathogenic bacteria, not the hardy strains found in most commercial probiotic supplements.
How long do mood changes last after finishing the antibiotic?
Typically a few days to two weeks. If symptoms persist beyond that, consider a gut‑health evaluation and speak with a mental‑health professional.
Is there a difference between oral and IV Cefaclor for mental side‑effects?
Oral Cefaclor is the only formulation widely used; IV versions are rare and generally reserved for hospital settings. IV delivery can lead to higher blood concentrations, slightly raising the odds of CNS effects.









12 Comments
Wow, this article really dives deep into the gut‑brain connection!!! I love how it breaks down the science in plain English and even throws in some practical tips-probiotics, fiber, mood journals-so you can actually do something about it!!! 🙌
All this talk about "gut health" is just another distraction from the real agenda-big pharma wants us glued to their pills while they control our thoughts!!! They don't want you to know that a simple probiotic can shut down their mind‑control experiments!!!
Interesting read, but I bet the benefits are overstated. Most people never notice any mood shift after a short course, so maybe it’s just a placebo effect mixed with hype.
Are you kidding me?? This whole "gut‑brain" thing sounds like a sci‑fi plot!!! I swear the doctors are feeding us nonsense while they hide the truth about chemicals in antibiotics!!!
Looks like another overblown article. I mean, how many people actually get anxious from a couple of pills? Probably none, just a buzz.
Honestly, the gut‑brain axis is a fascinating and complex system that we’re only beginning to understand. When you take a broad‑spectrum antibiotic like Cefaclor, you’re not only targeting the harmful pathogens but also wiping out a large portion of your resident microbiota. This disruption can reduce the production of short‑chain fatty acids such as butyrate, which are vital for maintaining the integrity of the gut lining and modulating inflammation. Without enough butyrate, the gut barrier can become more permeable, a condition often referred to as "leaky gut." This increased permeability allows bacterial endotoxins like lipopolysaccharide (LPS) to enter the bloodstream, triggering systemic inflammation. Systemic inflammation has been linked to elevated levels of cytokines, which can cross the blood‑brain barrier and affect neurotransmitter systems. In particular, serotonin-a neurotransmitter heavily involved in mood regulation-is largely produced in the gut. A disrupted microbiome can lead to an imbalance in serotonin synthesis, potentially contributing to anxiety or depressive symptoms. Moreover, the vagus nerve, a major communication highway between the gut and brain, can be influenced by microbial metabolites; alterations here might also impact emotional states. While the evidence directly tying Cefaclor to mood changes is still emerging, broader studies on cephalosporins suggest a modest increase in anxiety scores, as the article mentions. It’s important to note that these effects are generally more pronounced in individuals with pre‑existing mental health conditions or those who have experienced gut dysbiosis before. For most healthy adults, short‑term mood fluctuations are typically mild and resolve after the microbiome recovers, especially with the help of probiotics and prebiotic foods. In practice, taking a high‑quality probiotic during and after a course of Cefaclor can help reseed beneficial bacteria, supporting SCFA production and reducing inflammatory cascades. Pair this with a diet rich in fiber-think bananas, onions, chicory root-to feed any remaining microbes. Monitoring your mood with a simple daily journal can also alert you to any patterns that may need professional attention. In short, while antibiotics like Cefaclor are essential tools, being mindful of their impact on your gut ecosystem can help you protect both physical and mental well‑being. 😊
That was a thorough walk‑through-so many layers to consider! It reminds me that our bodies are like tiny ecosystems, and even a small disturbance can ripple out. I think the key takeaway is balance: use the antibiotic when needed, but also nurture the gut afterward. Your suggestion to pair with probiotics and fiber feels both practical and philosophically sound. After all, caring for the microbiome is an act of self‑respect, echoing the ancient wisdom that health is holistic. Thanks for laying it all out so clearly.
Good read.
Let’s get real-if you’re not supplementing with a high‑quality probiotic, you’re basically handing the gut a blank canvas and letting the bad guys paint over it. 🖌️🦠 That’s why the research emphasizes the role of butyrate‑producing bacteria; without them, you’re left with a gut that can’t keep inflammation in check. Probiotics like Lactobacillus rhamnosus GG or Bifidobacterium longum have shown promise in clinical trials for reducing anxiety scores. So, if you’re prescribed Cefaclor, think of it as a temporary ‘reset’-and then add the probiotic ‘restore’ to bring your microbiome back to equilibrium. 😎
Totally agree! Adding a probiotic is a simple step that can make a big diff. Also, keep drinking water and eating fiberrich foods like bananas and onions-these help feed the good bugs. If you notice any mood shifts, jot them down and chat with your doc. It’s all about staying proactive and supportive of your body.
Dear readers, it is with great enthusiasm that I encourage you to approach antibiotic therapy with both vigilance and optimism. By adhering to prescribed regimens, while simultaneously integrating probiotic supplementation and a fiber‑rich diet, one may effectively mitigate potential neuro‑psychological side effects. Let us strive for informed health decisions, grounded in scientific evidence and compassionate care.
Everything sounds fine on the surface, but remember there are hidden layers of control in medical guidelines. It’s possible that subtle mood alterations are being monitored to gauge population responses.