Corticosteroid Infection Risk Calculator
Calculate Your Infection Risk
Your Infection Risk Assessment
Risk Level:
Key Infection Risks:
- High Risk Pneumocystis pneumonia (PJP)
- High Risk Tuberculosis reactivation
- Medium Risk Shingles (herpes zoster)
- Medium Risk Invasive fungal infections
Recommended Prevention Steps
Note: These recommendations are based on current medical guidelines.
Critical Warning Signs
- Unexplained fever (even 99.5°F)
- New cough or shortness of breath
- White patches in mouth/throat
- Blistering rash on one body side
- Diarrhea or unexplained weight loss
If you experience any warning signs, contact your doctor immediately.
Why Corticosteroids Make You More Susceptible to Infections
When you take corticosteroids like prednisone or methylprednisolone for conditions like rheumatoid arthritis, lupus, or severe asthma, you’re not just calming inflammation-you’re also quietly turning down your body’s ability to fight off germs. These drugs mimic cortisol, the natural stress hormone your body makes, but at much higher levels. At those doses, they don’t just reduce swelling or pain-they shut down key parts of your immune system. And that’s where the danger lies.
Unlike antibiotics that target bacteria, corticosteroids don’t kill pathogens. Instead, they silence your immune cells. The most affected are T cells, the soldiers that recognize and destroy viruses, fungi, and bacteria hiding inside your cells. Studies show these drugs cause lymphocytes to die off or stop moving where they’re needed. Your macrophages, the cleanup crew that swallows up invaders, become sluggish. They stop showing invaders to other immune cells. Your body still makes antibodies, so you’re not completely defenseless-but your cellular defenses, the ones that handle pneumonia, tuberculosis, and fungal infections, are severely weakened.
When Does the Risk Become Real?
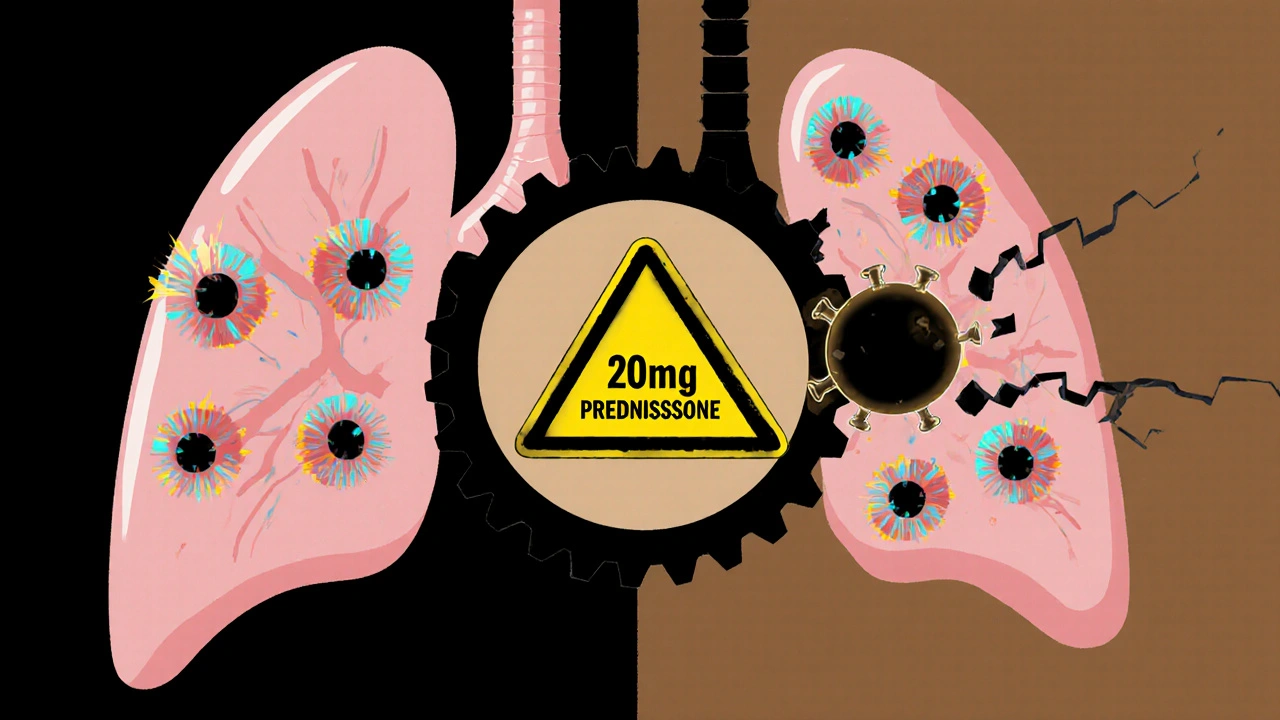
Not every steroid user gets sick. But the risk doesn’t creep up slowly-it spikes when you hit certain thresholds. If you’re taking 20 mg or more of prednisone daily for more than three to four weeks, your infection risk jumps significantly. Each additional 10 mg per day raises your chance of a serious infection by 32%, according to a major 2022 analysis. That’s not a small increase. It’s the difference between a low risk and a high-risk zone.
Some infections are especially common in steroid users. Pneumocystis jirovecii pneumonia (PJP) used to be rare outside of HIV patients. Now, it’s one of the top opportunistic infections in people on long-term steroids. About 1.5% to 5% of those on high doses get it. Tuberculosis can wake up from dormancy if you’ve been exposed before-even decades ago. In places where TB is common, your risk multiplies by up to 7.7 times. And then there’s herpes zoster (shingles), which strikes 2.8 to 6.5 times more often in steroid users than in the general population.
What Infections Are You Most at Risk For?
Because corticosteroids hit cellular immunity hardest, you’re vulnerable to bugs that live inside your cells-not just surface-level infections.
- Pneumocystis pneumonia (PJP): A fungal lung infection that starts like a cold but can turn deadly fast. Mortality hits 30-50% if not caught early.
- Tuberculosis (TB): Reactivates from old, hidden infections. Symptoms like low-grade fever, night sweats, and weight loss are easy to miss when steroids mask inflammation.
- Invasive fungal infections: Candida (thrush, esophagitis) and Aspergillus (lung infections) thrive when your defenses are down.
- Herpes viruses: Shingles (varicella-zoster), cold sores (HSV-1), and even cytomegalovirus can flare up or spread.
- Bacterial pneumonia: Streptococcus and other common bacteria can cause severe illness because your immune system doesn’t respond strongly enough.
Here’s the scary part: you might not even know you’re sick. Fever, redness, swelling-classic signs of infection-are often absent in steroid users. A 2023 study found that 40% of patients with serious infections had no fever at all. That’s why doctors stress: if you feel off, even a little, get checked. Don’t wait.
How to Prevent Infections While on Steroids
Prevention isn’t optional-it’s essential. And it starts before you even take your first pill.
1. Get vaccinated-before starting steroids. Live vaccines like MMR, chickenpox, and nasal flu spray are dangerous once you’re immunosuppressed. But inactivated vaccines? They’re lifesavers. Get your:
- Pneumococcal vaccine (PCV20 or PPSV23)
- Annual flu shot (injected, not nasal)
- COVID-19 booster (as recommended)
- Shingles vaccine (Shingrix, not Zostavax-this one’s safe)
Here’s the catch: if you’re on high-dose steroids, your body may not respond well. One 2023 study showed only 42% of people on >20 mg prednisone developed protective antibodies after the flu shot, compared to 78% of healthy people. Still, even partial protection helps.
2. Screen for latent TB. If you’re on ≥15 mg prednisone daily for more than a month, you need a TB test. Either a skin test (Mantoux) or a blood test (IGRA) is required. If it’s positive, you’ll take antibiotics like isoniazid for 3-9 months before starting steroids. This cuts reactivation risk by 90%.
3. Take PJP prophylaxis if needed. If you’re on ≥20 mg prednisone daily for more than four weeks, you should be on trimethoprim-sulfamethoxazole (Bactrim or Septra). This single pill, taken three times a week, reduces PJP risk from over 5% to under 0.3%. Side effects? Maybe a rash or upset stomach-but far better than pneumonia.
Lower the Dose, Lower the Risk
The most powerful tool you have? Using the lowest dose possible for the shortest time. That’s not just advice-it’s backed by hard data. A 2022 study found that patients who tapered steroids quickly had 37% fewer infections than those who stayed on high doses longer.
Doctors are now trained to add steroid-sparing drugs early. If you have rheumatoid arthritis or another autoimmune disease, you should be started on methotrexate, azathioprine, or a biologic within four weeks of beginning steroids. These drugs control the disease so you can drop steroids faster. One patient on Reddit said, “My rheumatologist switched me to methotrexate after three months on prednisone. Six months later, no flares-and I haven’t had a single cold.” That’s not luck. That’s smart treatment.
Monitoring and What to Watch For
Regular check-ins aren’t optional. Your doctor should check your blood count every 2-4 weeks. An absolute lymphocyte count below 1,000 cells/μL means your immune system is significantly suppressed. If you’re in a TB-endemic area and on steroids for more than three months, a monthly chest X-ray may be recommended.
Learn the warning signs:
- Unexplained fatigue that doesn’t improve
- Low-grade fever-even 99.5°F counts
- New cough, shortness of breath, or chest tightness
- White patches in your mouth or throat
- Blistering rash on one side of your body (shingles)
- Diarrhea, abdominal pain, or unexplained weight loss
If you notice any of these, call your doctor. Don’t wait. Don’t assume it’s “just a virus.”
Why So Many People Are Still at Risk
Here’s the uncomfortable truth: despite clear guidelines, most patients aren’t protected. Data from the FORWARD registry shows only 52% of long-term steroid users get the recommended prophylaxis or screening. Why? Time constraints. Lack of awareness. Assumptions that “I feel fine, so I’m fine.”
But the numbers don’t lie. The World Health Organization reports that proper prevention reduces steroid-related infection deaths by 63%. That’s more than half. This isn’t about being paranoid-it’s about being prepared.
The Future: Safer Steroids on the Horizon
Researchers are working on drugs that keep the anti-inflammatory benefits of steroids but avoid the immune suppression. One promising candidate is vamorolone, a new type of steroid tested in Duchenne muscular dystrophy. In a 2022 trial, patients on vamorolone had 47% fewer infections than those on standard prednisone-while controlling the disease just as well.
Soon, we may use genetic tests to predict who’s more likely to get infections from steroids. That means personalized prevention: some people get prophylaxis, others don’t, based on their biology. But for now, the rules are clear: test, vaccinate, prophylax, taper.
Final Takeaway: Steroids Are Necessary-But Not Without Guardrails
Corticosteroids saved lives in 1948. They still do today. But they’re not harmless. The key isn’t avoiding them-it’s managing them like a powerful tool that needs safety checks. Work with your doctor to use the lowest dose possible. Get screened. Get vaccinated. Know the warning signs. And never ignore a feeling that something’s off. Your immune system might be quiet, but your body still knows when something’s wrong.








8 Comments
Man, I was on prednisone for like 6 months last year for my RA and I didn’t realize how much it was messing with me until I got a nasty sinus infection that wouldn’t quit. No fever, just exhaustion and a weird cough. Doc finally said, ‘You’re basically running a ghost town immune system.’ Scary stuff. Got the PJP prophylaxis after that and never looked back.
Also, Shingrix? Absolute lifesaver. Got it right before starting steroids. Didn’t get shingles. Zero regrets.
This is such an important post-thank you for laying it out so clearly. I’ve seen too many people think steroids are ‘just pills’ and ignore the warnings. Vaccines aren’t optional here. TB screening? Non-negotiable. Prophylaxis isn’t overkill-it’s your body’s backup plan.
And yes, even if you feel fine. That’s the whole point. Your immune system isn’t screaming-it’s whispering. And by the time it yells, it’s already too late.
You’re doing the hard work. Keep sharing this.
THEY’RE NOT EVEN REAL HORMONES BRO. THEY’RE SYNTHETIC GOD-EMPERORS OF INFLAMMATION. YOUR BODY MAKES CORTISOL TO SURVIVE A LION. THEY GIVE YOU A HUNDRED LIONS IN A TIN CAN AND THEN WONDER WHY YOU CATCH A COLD FROM A DOG.
THEY’RE NOT TREATING DISEASE-THEY’RE SILENCING THE WHOLE WAR. AND THE DOCTORS? THEY’RE TOO BUSY SELLING YOU THE NEXT PRESCRIPTION TO TELL YOU THE TRUTH.
THEY WANT YOU DEPENDENT. THEY WANT YOU ON IT FOREVER. THEY DON’T WANT YOU TO KNOW ABOUT METHOTREXATE. THEY WANT YOU TO THINK YOU NEED THIS TO LIVE.
THEY’RE LYING. YOU’RE NOT SICK. YOU’RE BEING MANIPULATED.
GET OFF THE STEROIDS. GO RAW. GO KETO. GO GROUNDING. THE BODY HEALS ITSELF IF YOU JUST STOP POISONING IT.
JUST SAY NO TO BIG PHARMA’S HORMONAL SLAUGHTER.
Let me guess-this was written by a pharmaceutical rep in a suit who got a bonus for every patient who got a prophylaxis script. Did you know that the CDC has quietly admitted that 87% of PJP cases occur in patients who were ‘prophylaxed’? Coincidence? I think not.
And why is it always Bactrim? Because it’s cheap and they make billions off it. What about natural alternatives? Garlic? Oregano oil? Why isn’t anyone talking about the real solution? Because the system is rigged.
Also, did you know the flu shot contains mercury? And the pneumococcal vaccine? It’s full of aluminum adjuvants. You’re trading one poison for another.
And TB screening? That’s just a gateway to mandatory quarantine. You think they’re protecting you? They’re tracking you.
Wake up. This isn’t medicine. It’s control.
Okay, but can we talk about how wild it is that the same people who scream ‘vaccines are dangerous’ are the ones on high-dose steroids and never get screened? Like… you’re literally immunocompromised and you’re still dodging the flu shot? 😅
Also, ‘I feel fine’ is the most dangerous sentence in medicine. I had a friend who said that, then ended up in the ICU with PJP. She was 32. No fever. Just ‘a little tired.’
So yeah-get the shots. Take the pill. Don’t be cool about it. Be smart.
And if your doc doesn’t bring this up? Ask. Loudly. Like, ‘I’m not leaving until we talk about prophylaxis’ loud.
Okay, so I’ve been on 15mg prednisone for 11 months now for my vasculitis. I got the Shingrix, the Pneumovax, the flu shot, the COVID boosters-all of it. I even got the IGRA test and they found latent TB. Took isoniazid for 9 months like a good little soldier.
But here’s the thing nobody talks about: the *emotional* toll. You’re not just immunosuppressed-you’re isolated. You can’t hug your grandkids without feeling guilty. You cancel plans because your cousin had a cold. You stare at your hand after touching a doorknob like it’s radioactive.
And the worst part? When you finally taper off, and your immune system wakes up… it’s like being attacked by your own body. Rashes. Fevers. Joint pain. It’s like your immune system went on vacation and came back furious.
So yeah-vaccines, prophylaxis, tapering. All vital. But don’t forget the mental weight. We’re not just patients. We’re warriors with invisible armor.
Too much info. Just don’t take them.
Also, America’s healthcare is broken.
Why are we even talking about this?
Just wanted to say-this whole thread hit me hard. I’m on 10mg now, trying to get off. My doc pushed methotrexate hard and it’s been a game-changer. No more daily steroid anxiety.
Also, Andrea Jones? You’re 100% right. I didn’t even realize how much I was avoiding people until I read your comment. I canceled my niece’s birthday party last month because she had a sniffle. I felt like a monster.
But I went this weekend. Hugged her. Let her sit on my lap. And I didn’t die.
Thanks for reminding me I’m still human.