When you start taking a statin to lower your cholesterol, you expect to protect your heart-not feel like your muscles are breaking down. But for many people, that’s exactly what happens. Muscle pain, weakness, cramps, and fatigue are common complaints after starting statins. Some dismiss it as just aging or overdoing it at the gym. But for others, it’s something deeper: statin-induced myopathy. This isn’t just a nuisance. It’s a spectrum of muscle damage that can range from mild discomfort to life-threatening breakdown.
What’s Really Going On in Your Muscles?
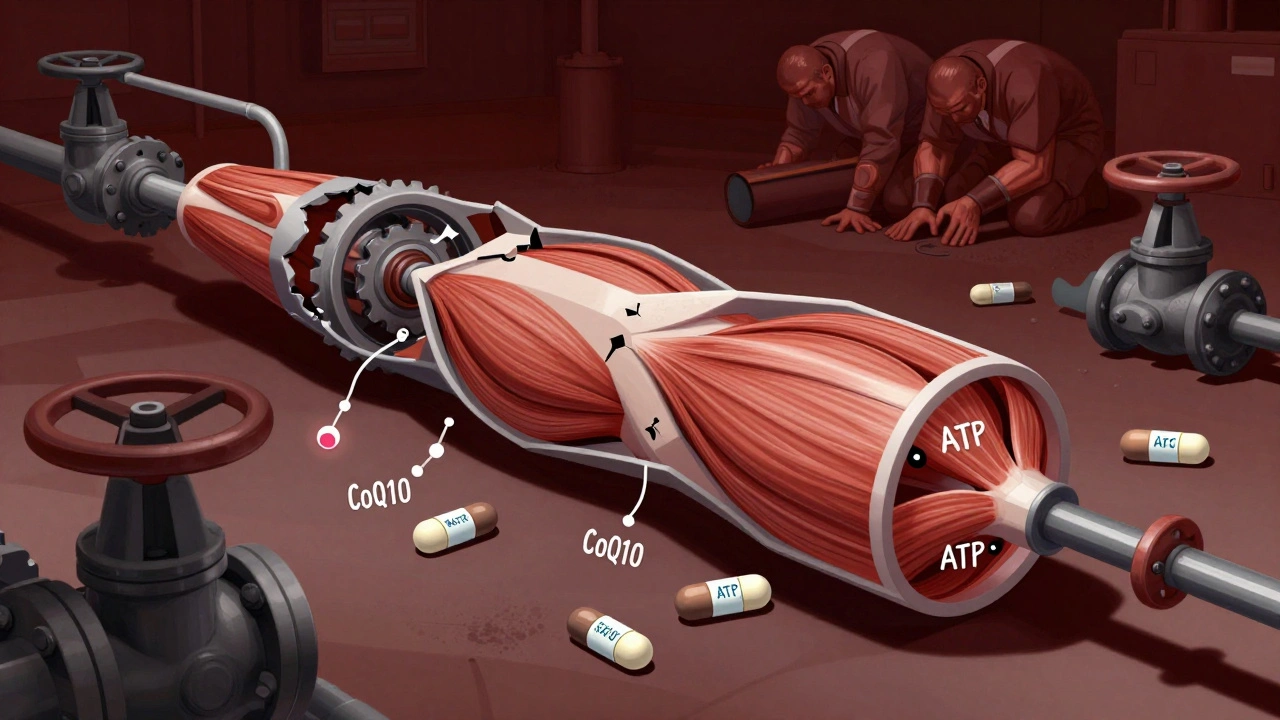
Statin drugs work by blocking HMG-CoA reductase, an enzyme your liver uses to make cholesterol. But that same enzyme is also part of a bigger pathway that produces other essential molecules-like coenzyme Q10 (CoQ10), dolichols, and prenylated proteins-that your muscles need to function properly. When statins shut this down, your muscle cells start running low on energy. Studies show that taking 40 mg of simvastatin daily can reduce CoQ10 levels in muscle tissue by up to 40%. Without enough CoQ10, your mitochondria-the powerhouses inside your muscle cells-can’t make enough ATP, the fuel your muscles use to contract. That’s why you feel tired, weak, or sore even when you haven’t done anything unusual. But it’s not just energy. Statins also interfere with protein prenylation, a process that helps regulate calcium levels inside muscle cells. When this goes wrong, calcium spills into the wrong places, triggering enzymes that chew up muscle proteins. One study found that muscle biopsies from statin users showed a 300-400% increase in activity of the ubiquitin-proteasome system-the body’s main cleanup crew for damaged proteins. In normal conditions, this system helps recycle old parts. On statins, it starts eating healthy muscle tissue.Myalgia vs. Myositis: Not the Same Thing
Not all muscle pain from statins is the same. The most common form is myalgia. This is when you feel achy, stiff, or weak muscles-but your blood test for creatine kinase (CK), a marker of muscle damage, stays normal. Around 10-29% of people on statins report this. It’s frustrating because doctors often say, “Your labs are fine, so it’s not the statin.” But symptoms are real, even without elevated CK. Then there’s myositis. This is muscle inflammation with actual damage. Your CK levels rise-usually between 10 and 40 times the normal upper limit. You might notice difficulty climbing stairs, lifting your arms, or getting up from a chair. Unlike myalgia, this is a clear sign your muscles are being injured. It affects about 0.5% of statin users. The most serious form is rhabdomyolysis. This is rare-only 0.01-0.1% of users-but dangerous. CK levels spike above 40 times normal. Muscle fibers break down so badly that they release myoglobin into your bloodstream, which can clog your kidneys and cause acute kidney failure. Symptoms include dark, tea-colored urine, extreme weakness, and swelling. If you have these, go to the ER immediately.The Hidden Culprit: Immune-Mediated Necrotizing Myopathy
There’s another type of statin-related muscle damage that doesn’t get enough attention: immune-mediated necrotizing myopathy (IMNM), also called statin-associated autoimmune myopathy (SAAM). It’s rare-only 2-3 cases per 100,000 statin users-but it’s devastating. In SAAM, your immune system starts attacking your own muscle tissue. A specific antibody, anti-HMGCR, forms in response to statins. This happens in people who carry a genetic marker called HLA-DRB1*11:01. Once triggered, your body keeps making these antibodies-even after you stop the statin. That’s why symptoms don’t go away like they do with regular myalgia. People with SAAM often have:- Progressive weakness in shoulders and hips (proximal muscles)
- CK levels over 2,000 IU/L (normal is 30-200)
- No improvement after stopping statins
- Muscle biopsy showing dead muscle fibers with little inflammation
Why Do Some People Get It and Others Don’t?
It’s not random. Genetics play a big role. A variation in the SLCO1B1 gene-rs4149056-makes it harder for your body to clear certain statins like simvastatin. People with this variant have a 1.4% risk of myopathy, compared to 0.6% in those without it. African Americans are 1.8 times more likely to develop statin myopathy than Caucasians, likely due to this same gene. Drug interactions matter too. If you’re on amiodarone, clarithromycin, or grapefruit juice, your body can’t break down statins properly. That can spike statin levels by 300-500%, dramatically increasing muscle damage risk. Age is another factor. SAAM mostly hits people over 50. Vitamin D deficiency, thyroid problems, and kidney disease also raise your risk. That’s why doctors should check these before blaming muscle pain on statins.What Should You Do If You Have Muscle Pain?
If you started statins and now have new muscle pain, don’t ignore it. Don’t assume it’s “just part of getting older.” Here’s what to do:- Stop the statin-don’t wait. Muscle damage can worsen even after you stop taking it, especially with SAAM.
- Get a CK blood test. Normal levels don’t rule out myalgia, but high levels (over 10x ULN) signal real damage.
- Check your thyroid and vitamin D. Low levels can mimic statin side effects.
- If pain lasts more than 3 weeks after stopping statins, ask for an anti-HMGCR antibody test.
- If positive, see a neuromuscular specialist. You may need steroids (like prednisone) and immunosuppressants like methotrexate.
Can You Go Back on Statins?
Yes-for some people. If you had mild myalgia and no antibody response, switching to a different statin might work. Rosuvastatin and fluvastatin are less likely to cause muscle problems. A 2021 study showed 73% of people who couldn’t tolerate simvastatin tolerated rosuvastatin after switching. Some people can even go back on statins at a lower dose or every other day. The IMPROVE-IT trial found 40% of patients with myalgia tolerated intermittent dosing (like 40 mg atorvastatin every other day). But if you have SAAM? Avoid all statins. Even low doses can trigger a flare-up. The antibodies stick around for years. Your best bet is non-statin options like ezetimibe, PCSK9 inhibitors (alirocumab, evolocumab), or bempedoic acid.
What’s Next for Treatment?
New tools are emerging. A 2023 study identified a blood test using microRNAs (miR-206 and miR-133a) that can tell apart SAAM from regular muscle pain with 89% accuracy. That means faster diagnosis and less waiting. For tough SAAM cases, a drug called ravulizumab-a complement inhibitor-showed a 75% response rate in a small 2022 pilot study. It’s not approved yet, but it’s a promising path. In the future, doctors may use genetic testing to pick the right statin for you before you even start. The American Heart Association predicts that within five years, pharmacogenomic testing could cut statin myopathy rates by 30-40%.The Bigger Picture
Stopping statins because of muscle pain sounds logical. But here’s the catch: a 2023 Circulation study found that people who quit statins due to side effects had a 25% higher risk of heart attack or stroke over the next 10 years. That’s huge. The goal isn’t to avoid statins entirely. It’s to manage the risk. If you have muscle pain, get tested. If you have SAAM, get treated. If you can’t tolerate statins, there are alternatives. Don’t let fear stop you from protecting your heart-but don’t ignore your muscles either.Frequently Asked Questions
Can statin muscle pain go away on its own?
Yes-but only if it’s simple myalgia. Most people feel better within 1-2 weeks after stopping the statin. If your pain lasts longer than 3 weeks, especially if you’re still weak or your CK is high, it could be immune-mediated myopathy, which won’t resolve without treatment.
Is CoQ10 supplementation effective for statin muscle pain?
The evidence is mixed. Some small studies show slight improvement, but three out of seven major trials found no benefit. CoQ10 doesn’t fix the underlying immune reaction in SAAM. It may help with energy levels, but don’t rely on it as a solution.
What’s the difference between statin myopathy and fibromyalgia?
Fibromyalgia causes widespread pain, fatigue, and sleep issues, but no muscle damage or elevated CK. Statin myopathy causes true muscle weakness, often in the hips and shoulders, and shows up on blood tests and biopsies. Many SAAM patients are misdiagnosed with fibromyalgia-delaying proper treatment by over a year.
Can I take a different statin if one caused muscle pain?
Possibly. About 73% of people who couldn’t tolerate simvastatin tolerated rosuvastatin after switching. Fluvastatin and pravastatin are also lower-risk options. But if you had SAAM (anti-HMGCR positive), avoid all statins-they can trigger a relapse.
How do I know if I have immune-mediated statin myopathy?
Look for these signs: persistent muscle weakness after stopping statins, CK levels above 2,000 IU/L, no improvement in 3 months, and weakness focused on hips and shoulders. A blood test for anti-HMGCR antibodies and a muscle biopsy are needed to confirm it. See a neuromuscular specialist if you suspect this.
Are there alternatives to statins if I can’t tolerate them?
Yes. Ezetimibe lowers LDL by about 20%. PCSK9 inhibitors like evolocumab can drop it by 60% and are given as monthly injections. Bempedoic acid works in the liver like statins but doesn’t enter muscle tissue, so it’s much less likely to cause muscle pain. These options protect your heart without the muscle risks.







12 Comments
statins made me feel like my legs were made of wet cement. stopped ‘em. felt better in a week. doc said it was all in my head. lol.
bro the HMG-CoA reductase inhibition cascade is wild. you’re basically sabotaging the mevalonate pathway which means you’re downregulating isoprenoid intermediates that are critical for membrane integrity and calcium homeostasis. it’s not just CoQ10-it’s the whole damn prenylation axis. most docs don’t even know this.
My uncle had SAAM. Took him 2 years to get diagnosed. He was misdiagnosed with fibromyalgia for 18 months. By the time they did the anti-HMGCR test, he could barely lift his coffee cup. IVIG saved him, but he’s still on methotrexate. If you’ve had muscle pain for more than 3 weeks after stopping statins-get tested. Don’t wait.
YOU ARE NOT ALONE. 💪 I was on Lipitor for 3 years and thought I was just getting old. Then I couldn’t climb stairs. I cried in the grocery store because I couldn’t lift my own cart. Stopped the statin. Got tested. Anti-HMGCR positive. IVIG changed my life. You deserve to move without pain. Fight for your health.
Let’s be real-pharma doesn’t want you to know this. Statins are billion-dollar drugs. SAAM? Rare? Sure. But how many people are just told to ‘tough it out’ while their muscles rot? I’ve seen three people in my neighborhood go from hiking to wheelchairs after statins. And the doctors? They blame age, arthritis, ‘lack of exercise.’ Meanwhile, the real culprit is sitting in a pill bottle labeled ‘heart-healthy.’
And don’t get me started on CoQ10 supplements. It’s like putting a bandaid on a gunshot wound. You need to address the immune system, not just the mitochondria. If your CK is over 2000 and you’re still weak after 3 months? You’re not lazy. You’re immunocompromised by a drug you were told was safe.
And yes, I’m mad. I should’ve known better. But I trusted the system. Now I’m the guy who reads every paper on HLA-DRB1*11:01 and tells everyone I know to get tested before starting statins. You’re not crazy. You’re just one of the 0.002% who got screwed by a system that doesn’t care until you’re in a wheelchair.
Oh please. Everyone’s just mad because they can’t eat fried food anymore. My cholesterol was 280. I took the statin. I felt fine. If you’re weak, maybe you’re just out of shape. Stop blaming Big Pharma for your laziness.
My dad had rhabdo. Ended up in ICU. CK was 80,000. They said it was the simvastatin + grapefruit juice combo. He didn’t even know grapefruit was a problem. Now he’s on ezetimibe. No muscle pain. No drama. Just a daily pill that works. Point is: don’t assume you’re immune. Read the damn label.
As someone who grew up in a family of cardiologists, I’ve seen this play out too many times. Statins are miraculous for high-risk patients-yes. But the blanket prescribing culture in the U.S. is terrifying. We treat cholesterol like a villain instead of a molecule with a job. And when muscle pain hits, the reflex isn’t investigation-it’s dismissal. ‘It’s just aging.’ ‘Try yoga.’ ‘Maybe you’re depressed.’
SAAM isn’t a myth. It’s a tragedy waiting to happen to someone’s mother, father, sibling. And we’re not talking about a few outliers. We’re talking about a biological betrayal-your own immune system, turned against you by a drug meant to save you.
I’m not anti-statin. I’m pro-informed consent. If you’re going to prescribe a drug that can trigger autoimmune destruction, you owe the patient a conversation about HLA typing, SLCO1B1 variants, and the real risk of irreversible damage. Not a pamphlet and a prescription.
Statins are a scam. America’s big pharma racket. You think they care if you can’t walk? Nah. They just want you to keep buying the pills. I stopped mine and my energy came back. Now I eat butter, eggs, bacon. My cholesterol’s still high. But I can lift my grandkids. That’s worth more than a number on a lab report.
Wow. So the guy who wrote this is basically saying ‘if you’re not rich enough to afford $1400/month PCSK9 inhibitors, you’re just gonna die of a heart attack.’ Real compassionate. Also, ‘don’t rely on CoQ10’-cool, so what’s the alternative? A miracle? Or just… die quietly?
One must contemplate the epistemological paradox inherent in pharmaceutical intervention: if a drug that reduces mortality also induces iatrogenic myopathy, does its net benefit remain quantifiable? Or does the subjective suffering of the individual nullify the statistical advantage of the population? The data is clear-but the human cost is silent in the RCTs. We are not variables. We are flesh, mitochondria, and memory.
I had myalgia for 8 months. Thought I was just stressed. Then I found this post. Got tested. Anti-HMGCR positive. Started prednisone. My strength came back in 3 months. I’m not saying don’t take statins. I’m saying: if your pain doesn’t go away after stopping, don’t accept ‘it’s all in your head.’ Push. Get the test. Your muscles aren’t lying.