
When you’re pregnant, your body changes in ways you never expected. One of the most surprising? Your pancreas suddenly has to work three times harder just to keep your blood sugar in check. That’s because the placenta starts pumping out hormones that block insulin - your body’s natural way of moving glucose into cells. For most women, the pancreas rises to the challenge. But for about 1 in 10, it can’t keep up. That’s gestational diabetes - high blood sugar that starts during pregnancy and usually disappears after birth. But if it’s not managed, it can lead to big problems for both you and your baby.
Why Gestational Diabetes Happens
It’s not your fault. You didn’t eat too much sugar. You didn’t skip workouts. This isn’t about willpower. Gestational diabetes happens because of hormones - specifically, those made by the placenta. Around weeks 24 to 28, these hormones start making your cells resistant to insulin. Your body needs to produce up to three times more insulin than normal to keep glucose levels stable. If your pancreas can’t meet that demand, glucose builds up in your blood. That’s gestational diabetes.It’s not rare. In the U.S., it affects 2 to 10% of pregnancies every year. And the numbers are climbing. Back in 2000, about 4.6% of pregnant women had it. By 2019, that number jumped to 9.2%. Why? Older moms, higher body weight, and more sedentary lifestyles are all playing a role. The good news? If you catch it early and manage it right, your chances of having a healthy baby are nearly the same as someone without gestational diabetes.
What the Numbers Mean
Your doctor will likely screen you between 24 and 28 weeks with a glucose challenge test. You’ll drink a sugary solution, then have your blood drawn one hour later. If your result is above 140 mg/dL, you’ll move on to a more detailed test - a three-hour oral glucose tolerance test. That’s when they check your blood sugar four times after drinking a stronger sugar mix. Diagnosis happens if two or more readings are too high.Once diagnosed, you’ll get specific targets to hit every day:
- Fasting or before meals: under 95 mg/dL
- One hour after eating: under 140 mg/dL
- Two hours after eating: under 120 mg/dL
These aren’t random numbers. They’re based on decades of research showing that keeping blood sugar within this range cuts the risk of having a baby too big (over 8 pounds 13 ounces), reduces the chance of shoulder injuries during delivery, and lowers the risk of your newborn having low blood sugar right after birth. Studies show that women who stick to these targets have outcomes nearly identical to those without gestational diabetes.
Food Is Your First Tool
About 70 to 85% of women can manage their blood sugar with diet and movement alone. No pills. No shots. Just smarter eating.Carbohydrates are your biggest challenge - not because they’re bad, but because they turn into glucose fast. The key isn’t to cut them out. It’s to control how much and when you eat them.
Most experts recommend:
- 35-40% of your daily calories from complex carbs
- 45 grams of carbs per meal
- 15-30 grams per snack
- 17-19 carb choices per day (1 choice = 15 grams of carbs)
That means: one slice of whole grain bread, half a cup of oatmeal, or a small apple each count as one choice. A cup of cooked rice? That’s three choices. A large banana? Also three. Portion control matters more than you think.
Here’s what works for most women:
- Start every meal with protein or healthy fat - chicken, eggs, fish, avocado, nuts, or cheese
- Then eat vegetables
- Save carbs for last
This simple trick - eating protein and veggies before carbs - can lower your post-meal blood sugar by 25 to 40 mg/dL. Why? It slows digestion. Your body doesn’t get hit with a sugar rush all at once.
Pairing carbs with fat or protein also helps. Eat an apple with a tablespoon of peanut butter instead of just the apple. Have whole grain toast with eggs instead of toast with jam. These small swaps make a huge difference.
And don’t skip snacks. Eating three meals plus two to three small snacks spread through the day keeps your blood sugar steady. Going too long without food can cause your liver to dump glucose into your blood - especially in the morning. That’s why many women struggle with high fasting levels. A bedtime snack with 15 grams of carbs and some protein - like six crackers and an ounce of cheese - can help prevent that.

Move Your Body - Even a Little
Exercise isn’t optional. It’s medicine.Thirty minutes of moderate activity five days a week - like walking, swimming, or prenatal yoga - can drop your blood sugar by 20 to 30 mg/dL. The best time? 15 to 30 minutes after a meal. That’s when your blood sugar is highest, and movement helps your muscles soak up glucose without needing extra insulin.
Many women find that a 15-minute walk after dinner cuts their evening spike. Others swear by morning walks to lower their fasting numbers. One Reddit user shared that her morning walk brought her fasting glucose down by 15 to 25 mg/dL. That’s the difference between needing insulin and staying on diet alone.
You don’t need to run a marathon. Just move. Even if it’s just pacing while talking on the phone or doing squats while brushing your teeth - every bit helps.
When Diet and Exercise Aren’t Enough
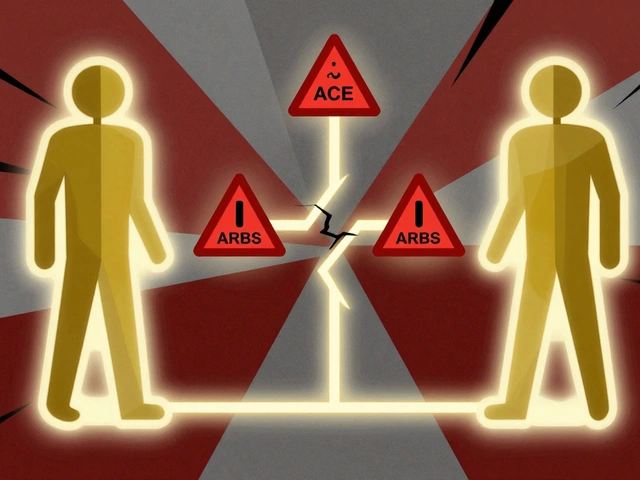
About 15 to 30% of women still can’t hit their targets, even with perfect food and movement. That’s when insulin becomes necessary. And it’s not a failure. It’s science.Insulin is safe during pregnancy. It doesn’t cross the placenta, so it won’t affect your baby. Many women worry about needles, but most find the injections easier than they expected. Some use insulin pens, which are small and quiet. Others get a pump if their numbers are all over the place.
Metformin is sometimes used, especially in places where insulin isn’t easily available. But it’s not the first choice. Studies show that about 30% of women on metformin still need to add insulin later. The American Diabetes Association says insulin remains the gold standard for when diet isn’t enough.
Continuous glucose monitors (CGMs) are becoming more common. These tiny sensors, worn on your arm or belly, track your sugar levels all day and night. They’re especially helpful if you’ve had Type 1 diabetes before, or if your numbers are hard to control. One study showed CGMs reduced the risk of having a very large baby by 39% and lowered severe newborn low blood sugar by 54%.
Monitoring Is Non-Negotiable
You’ll need to check your blood sugar 4 to 6 times a day - before meals and 1 to 2 hours after eating. Record what you ate, what time you ate, and your number. That’s how you learn what works.Some women track with paper logs. Others use apps like MyFitnessPal or MySugr. The goal is to spot patterns. Do your numbers spike after rice? After fruit? After lunch? Once you see the pattern, you can adjust.
Don’t skip this step. Women who check less than four times a day are more than twice as likely to have a baby who ends up in the NICU. That’s not scare tactics - that’s data from the SWIFT trial.
What Happens After the Baby Is Born
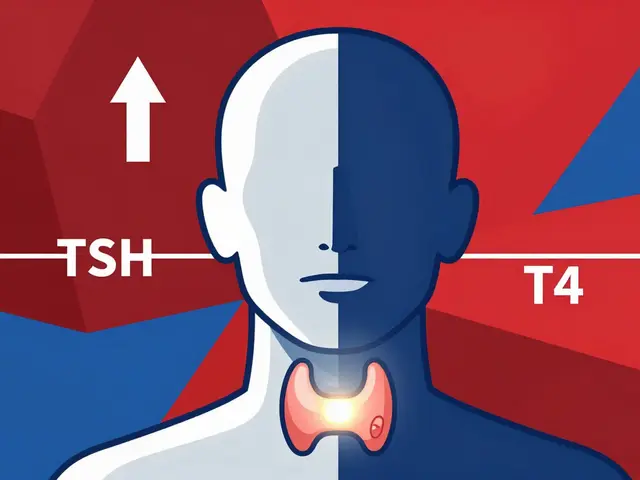
Here’s the good news: for 70% of women, gestational diabetes disappears after delivery. Your body resets. Your pancreas catches up.But here’s the warning: 50% of women who had gestational diabetes will develop Type 2 diabetes within 10 years. That’s not fate. It’s a signal.
Within 6 to 12 weeks after birth, you’ll get a glucose test - usually a 75-gram oral glucose tolerance test. If your fasting number is above 126 mg/dL or your 2-hour number is above 200 mg/dL, you have Type 2 diabetes. If it’s between 140 and 199 mg/dL, you have prediabetes. Either way, you’re at high risk.
But you can change that. The TODAY2 study found that losing just 5 to 7% of your body weight after pregnancy - about 10 to 15 pounds for most women - cuts your risk of Type 2 diabetes by 58% over 15 years. That means eating whole foods, staying active, and keeping your weight in check isn’t just for now. It’s for your future.
Support Is Out There
Getting diagnosed can feel overwhelming. Sixty-eight percent of women say the initial diagnosis was emotionally hard. Forty-two percent were scared of insulin. But 85% of women who got clear, consistent education said they felt in control.Work with a certified diabetes care and education specialist (CDCES). They’ll teach you carb counting, how to use your meter, and how to read your patterns. Most clinics offer one-on-one sessions and follow-up calls. Many women say those weekly check-ins were the reason they stayed on track.
Online communities like Reddit’s r/GestationalDiabetes are full of real stories. Women share what worked: meal prep tips, favorite snacks, how to handle cravings, and how to deal with judgment from family members who say, “But you’re just eating a little sugar.” You’re not being dramatic. You’re protecting your baby.
What Not to Do
Don’t ignore your numbers. Don’t wait until you feel “bad” to check. Don’t assume it’ll go away on its own. Don’t let conflicting advice from different providers confuse you. If your OB and your endocrinologist give you different carb limits, ask them to talk to each other. Your health is too important for mixed messages.And don’t believe the myth that gestational diabetes means you have to eat bland, boring food. You can still have pizza - just pair it with a big salad and chicken. You can have dessert - just have half a serving and wait 20 minutes before eating it. You’re not on a punishment diet. You’re learning how to eat smarter for two.


8 Comments
Just ate a bagel with cream cheese. My sugar’s 180. Guess I’m failing.
I was terrified when I got diagnosed-thought I’d ruined my pregnancy. But after working with my CDCES and learning to pair carbs with protein, everything changed. I started walking after every meal-even just 10 minutes-and my numbers dropped like magic. The snacks? Game-changer. A handful of almonds + a small apple before bed? No more 110 fasting. You’re not broken. You’re adapting. And you’re doing better than you think.
Let’s be honest: this is just capitalism’s latest weaponized guilt-trip wrapped in a ‘healthy pregnancy’ bow. The real issue? The medical-industrial complex has turned gestational diabetes into a profit engine-CGMs, insulin pens, certified specialists, apps, labs. Meanwhile, the root cause? Poor food systems, corporate sugar subsidies, and the commodification of maternal health. You’re not ‘failing’-you’re just the latest target in a billion-dollar industry selling ‘control’ to exhausted women. Eat real food. Move. Breathe. And stop paying for someone else’s panic.
Interesting how the narrative sidesteps the epigenetic elephant in the room. The placental insulin resistance isn’t a ‘dysfunction’-it’s an evolutionary adaptation to nutrient scarcity. In ancestral environments, this mechanism conserved glucose for fetal brain development during famine. Now, in a hypercaloric, hyperglycemic milieu, it’s maladaptive. We’re essentially seeing a mismatch between Paleolithic physiology and neoliberal food policy. Insulin? Fine. But the real intervention is cultural: decouple ‘health’ from moral virtue. You’re not a failed metabolizer-you’re a biological artifact of systemic dietary collapse. 🤷♂️
Let’s not sugarcoat this (pun intended). The 70-85% success rate with diet/exercise? That’s a statistical mirage. Most of those women are either under-reporting their numbers, skipping tests, or have a naturally more responsive pancreas. The real 15-30% who need insulin? They’re the ones who actually followed the guidelines. The rest are just deluding themselves with ‘apple with peanut butter’ magic. And don’t get me started on the ‘walk after meals’ cult-studies show it only helps if you’re already lean. For overweight women? It’s placebo with a pedometer. The system rewards compliance, not outcomes. You’re being sold a lie wrapped in a Whole Foods tote bag.
For anyone feeling overwhelmed: you’re not alone. I had two babies with GD. The first time, I cried every night because I felt like a failure. The second time, I had a certified diabetes educator who didn’t just give me charts-she asked me what I liked to eat, and we built a plan around it. I ate sushi rolls with brown rice, roasted veggies with tofu, and dark chocolate-covered almonds as snacks. I checked my numbers religiously-and yes, it sucked. But I didn’t need insulin. I didn’t have a NICU baby. And I didn’t lose my mind. You can do this. Not perfectly. Just consistently. And if you slip? Eat something healthy next meal. No guilt. Just next step.
OMG I just tried the ‘protein-veggies-first’ trick and my post-lunch spike dropped from 172 to 118!! 🙌 I used to eat rice and curry like it was a religion-now I eat the chicken and broccoli first, then the rice like a dessert. Also, my mom called me ‘crazy’ for not eating her homemade ladoos-so I sent her this article and now she brings me kale chips. 💪 You’re not being dramatic-you’re saving your baby. And your future self. #GestationalDiabetesWarrior
THEY’RE LYING TO YOU!!! The ‘disappears after birth’ myth? It’s a cover-up. The CDC KNOWS that 80% of women who get GD develop Type 2 within 5 years-not 10. They don’t tell you because Big Pharma needs insulin sales. And CGMs? They’re surveillance tools for insurance companies to raise your premiums. You’re being tracked, monitored, and manipulated. Stop checking your numbers. Stop walking. Eat real food-meat, eggs, butter. No carbs. No apps. No ‘specialists.’ Your body knows what to do. Trust it. Or else… they’ll take your baby. I’m not joking.