
For women with PCOS and obesity, losing weight isn’t just about looking different-it’s about fixing broken hormones, getting periods back, and lowering the risk of type 2 diabetes. For years, metformin was the go-to, but it often only helped a little. Now, a new class of drugs called GLP-1 receptor agonists is changing the game. These aren’t magic pills, but for many women, they’re the most effective tool they’ve ever had to take back control of their health.
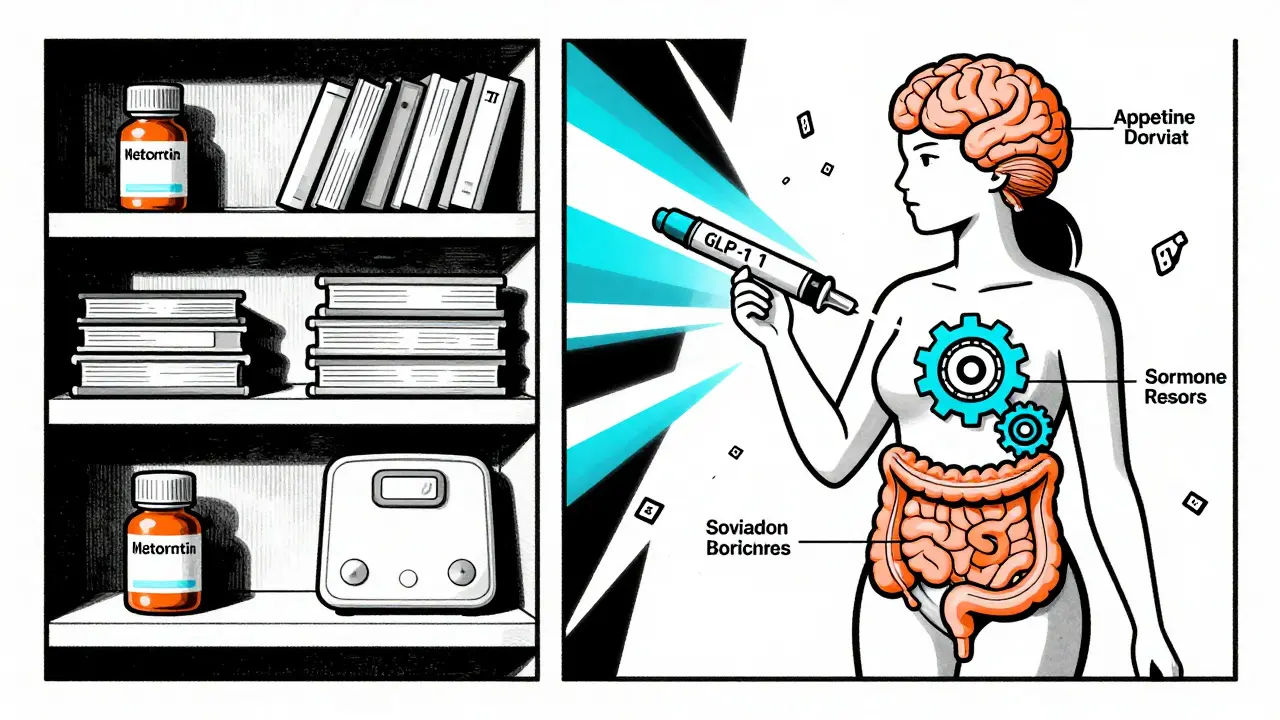
What GLP-1s Actually Do
GLP-1s-like liraglutide (Saxenda) and semaglutide (Wegovy)-were first made to treat type 2 diabetes. But doctors noticed something surprising: patients lost weight. A lot of it. Turns out, GLP-1 receptors aren’t just in the pancreas. They’re in the brain, the gut, and even the ovaries. These drugs slow down how fast food leaves your stomach, make you feel full faster, and reduce cravings. For women with PCOS, where hunger signals are often scrambled and insulin resistance is common, this is huge.
It’s not just about appetite. GLP-1s help the body use insulin better, lower testosterone levels, and reduce fat around the organs-visceral fat-that’s linked to heart disease and diabetes. In one study, women with PCOS using semaglutide lost nearly 6% of their body weight in just 12 weeks. That’s not just a number-it’s the difference between not ovulating and ovulating regularly.
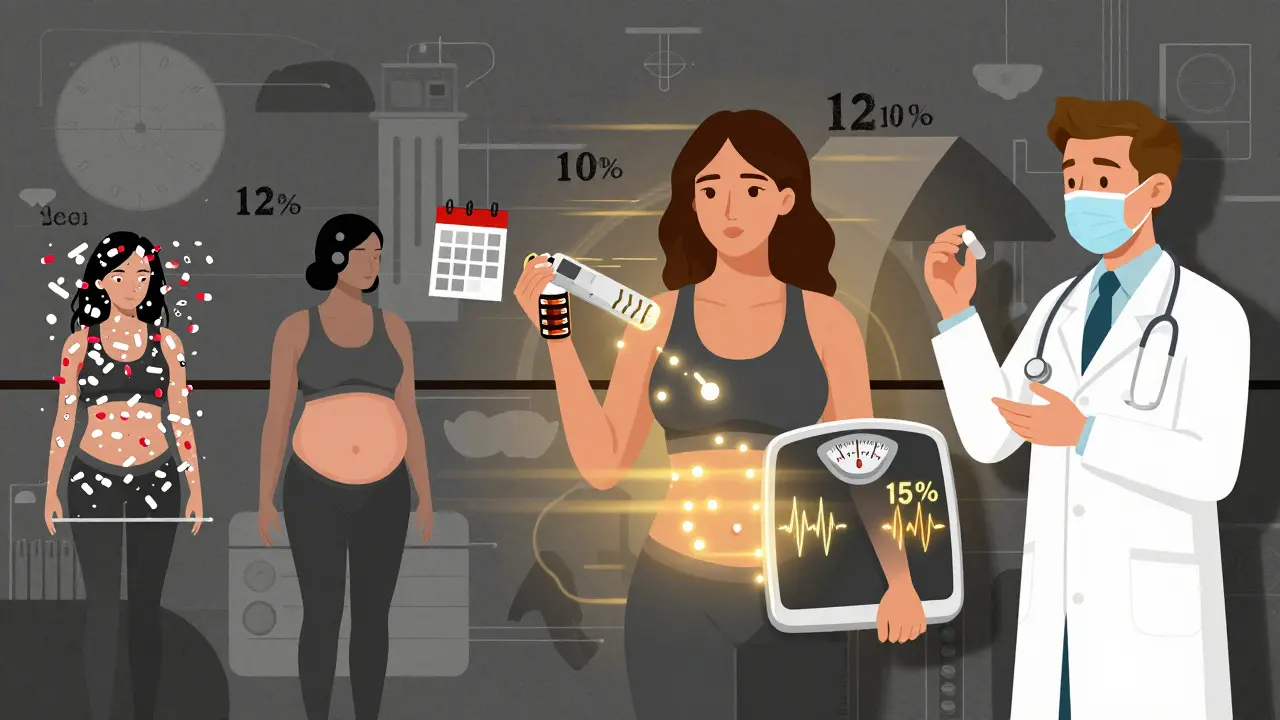
How Much Weight Can You Really Lose?
Let’s be clear: results vary. But the data is hard to ignore. In clinical trials, women with PCOS on liraglutide lost an average of 5-10% of their starting weight. With semaglutide, it’s even higher-up to 15% over a year. Compare that to metformin, which typically leads to 2-5% loss. That extra weight isn’t just fat on the scale. It’s fat around the liver, fat around the heart, fat that’s fueling inflammation and high testosterone.
One woman in a 2022 study saw her testosterone drop from 68 to 42 ng/dL after six months on semaglutide. She had her first regular period in three years. That’s not luck. That’s biology responding to weight loss. When you lose 5% of your body weight, your body starts to reset. Insulin sensitivity improves. Androgen levels fall. Ovulation returns. GLP-1s help you get there faster.
GLP-1s vs. Metformin: The Real Comparison
Metformin is still useful. It’s cheap, safe, and helps with insulin resistance. But it doesn’t touch appetite the way GLP-1s do. If you’re trying to lose weight and metformin hasn’t worked after six months, you’re not failing-you just need a different tool.
Here’s the numbers: a 2024 meta-analysis showed GLP-1s led to 3.57 kg more weight loss than placebo. Compared to metformin, they reduced BMI by 1.11 kg/m² more. That might sound small, but in real life, that’s an extra 10-15 pounds off your frame. And it’s not just weight. GLP-1s also lower triglycerides, improve HDL cholesterol, and reduce markers of inflammation linked to heart disease.
The catch? Cost. Metformin costs $10-$20 a month. GLP-1s? $800-$1,400. That’s why many women use them for a year, then switch back to metformin to hold onto the gains. One study found that women who stayed on metformin after stopping semaglutide kept 70% of their weight loss. Those who stopped both? They regained most of it.
Side Effects: What No One Tells You
These drugs aren’t easy. Nausea is the most common side effect-about 44% of users report it. Vomiting, dizziness, and constipation happen too. Most of the time, it gets better after a few weeks. But for some, it doesn’t. That’s why doctors start low: 0.25 mg of semaglutide once a week, then slowly increase every four weeks. Rushing the dose? You’ll feel awful.
People on Reddit’s r/PCOS forum talk about it openly. One user wrote: “Spent $1,200 a month on Wegovy. Lost 15 pounds, but I couldn’t keep anything down. Switched back to metformin.” Another said: “Six months in, I lost 28 pounds. My periods came back. Worth every penny.” The difference? Patience and support. Starting slow. Eating smaller meals. Avoiding greasy or sugary foods. Drinking water. These aren’t optional-they’re part of the treatment.
Who Benefits Most-and Who Doesn’t
GLP-1s work best for women with PCOS who have a BMI over 30 and signs of insulin resistance: dark skin patches (acanthosis nigricans), high fasting insulin, or prediabetes. If you’re lean with PCOS-normal weight, no metabolic issues-you’re unlikely to see much benefit. These drugs target metabolic dysfunction. They’re not for everyone.
They’re also not for everyone with a history of thyroid cancer. And they’re not approved yet for PCOS in most countries. Right now, they’re used off-label. That means your doctor has to explain the risks and benefits. Insurance rarely covers them for PCOS. You’re paying out of pocket.
What’s Next? The Future Is Coming Fast
In June 2024, the European Medicines Agency accepted a new application for semaglutide 2.4 mg to be officially approved for PCOS. A decision is expected in early 2025. That’s huge. If approved, it will change how doctors treat PCOS. No more off-label guessing. Insurance might start covering it. More clinics will offer it.
Even bigger: new drugs are coming. Retatrutide, a triple agonist that hits GLP-1, GIP, and glucagon receptors, is showing 24% weight loss in early trials. Oral versions of GLP-1s, like Rybelsus, are already available for diabetes and could make this easier to take long-term.
One thing’s certain: the days of treating PCOS with birth control pills alone are fading. We now know it’s a metabolic disorder first. Weight loss isn’t a side effect-it’s the treatment. And GLP-1s are the most powerful tool we’ve had to make that happen.
How to Get Started
If you’re considering GLP-1s:
- Get tested for insulin resistance-fasting insulin, HOMA-IR, or glucose tolerance test.
- Track your weight and symptoms for a few months on lifestyle changes first. If you’re stuck, it’s time to talk about medication.
- Find a doctor experienced in PCOS and metabolic health. Not all endocrinologists know about this.
- Ask about starting low and going slow. Don’t rush the dose.
- Combine it with nutrition and movement. GLP-1s help, but they don’t replace healthy habits.
- Plan for cost. Consider using them for 12-18 months, then switching to metformin to maintain.
It’s not a quick fix. But for women tired of cycling through diets, birth control, and frustration, it’s the closest thing to a real solution we’ve seen in decades.
Can GLP-1s help me get pregnant if I have PCOS?
Yes, for many women. Weight loss of 5-10% often restores ovulation. In one study, 42% of women on liraglutide had spontaneous ovulation after 24 weeks. GLP-1s don’t directly trigger ovulation like fertility drugs, but by improving insulin resistance and lowering testosterone, they create the conditions for natural ovulation to return. Many women conceive after starting these medications, even without additional fertility treatment.
How long do I need to take GLP-1s for PCOS?
There’s no fixed timeline. Most studies use them for 12-72 weeks. But PCOS is a lifelong condition. Once you stop, weight often returns-especially if you go back to old eating habits. Many women use GLP-1s for 1-2 years to reset their metabolism, then switch to metformin or lifestyle changes to hold the gains. Some stay on them long-term if they can afford it and tolerate them well.
Are GLP-1s safe for long-term use?
So far, yes. Semaglutide and liraglutide have been studied for up to 5 years in obesity and diabetes, with no new major safety concerns. The biggest risks are gastrointestinal side effects and rare gallbladder issues. Long-term data specific to PCOS is still limited, but the biological mechanisms suggest sustained benefit without new dangers. Regular check-ups with your doctor are still important.
Do GLP-1s cause muscle loss?
Some weight loss from any method includes muscle, but studies show GLP-1s preserve more muscle than dieting alone. One trial found that 70% of the weight lost with semaglutide was fat, not muscle. To protect muscle, it’s important to get enough protein (1.2-1.6g per kg of body weight) and do strength training 2-3 times a week.
Can I take GLP-1s if I have thyroid issues?
No-if you or a close family member has had medullary thyroid cancer, or if you have multiple endocrine neoplasia syndrome type 2, GLP-1s are not safe. They’re also not recommended if you have a personal history of pancreatitis. Always tell your doctor your full medical history before starting.





9 Comments
so i tried wegovy for 3 months and lost 18lbs but my stomach felt like it was gonna explode every time i ate anything that wasn’t plain chicken breast and steamed broccoli. also i spent like 1200 a month and my insurance said no. i’m back on metformin and eating pizza again. worth it?? idk.
oh here we go again with the ‘glp-1s are magic’ narrative. let me guess, you also think intermittent fasting cures cancer and kale fixes your trauma? this isn’t medicine, it’s capitalism selling you a $1400 placebo with nausea as a bonus feature. women with pcos have been surviving without this for centuries. why are we suddenly so desperate to chemically ‘fix’ our bodies instead of fixing the system that makes us feel broken?
Oh sweet summer child, you think losing 15% of your body weight magically ‘resets’ your hormones? How quaint. Let me remind you that PCOS isn’t just a ‘weight issue’-it’s a systemic metabolic collapse fueled by patriarchal neglect of women’s health. You’re treating symptoms like they’re the disease. And don’t get me started on how this drug is marketed to women who’ve been gaslit by doctors for decades into thinking their bodies are ‘broken’-when really, the medical system just refuses to invest in real solutions. Also, 1400 a month? That’s not healthcare, that’s financial exploitation dressed up as empowerment.
And yes, I’ve read the studies. The ones that don’t mention how 70% of participants dropped out due to GI misery. But sure, let’s celebrate the 30% who made it through while ignoring the rest of us who just wanted to eat a burrito without crying.
It’s fascinating how we’ve reduced the complex endocrine dysregulation of PCOS down to a single pharmacological lever. GLP-1 agonists don’t ‘fix’ anything-they modulate appetite and insulin sensitivity, which are symptoms, not root causes. The real tragedy isn’t the cost or the nausea-it’s that we’ve created a medical culture where the only acceptable solution to a chronic, multifactorial condition is a high-priced injection that requires lifelong compliance. We’re not treating PCOS. We’re managing its visibility. And we’re doing it in a way that only the affluent can afford. The fact that this is even considered a breakthrough says more about our healthcare priorities than it does about the drug’s efficacy.
Also, the phrase ‘reset your metabolism’ is scientifically meaningless. Metabolism isn’t a light switch. It’s a dynamic, adaptive system shaped by genetics, environment, stress, sleep, and socioeconomic factors. To reduce it to a 12-week weight loss campaign is not just reductive-it’s dangerous.
metformin is trash. i lost 22lbs on semaglutide in 6 months. nausea sucked for the first 2 weeks but then it was fine. i got my period back after 4 years. no more acne no more hair everywhere. worth every penny. people who say its too expensive are just scared to try. also dont eat fried food. duh.
I just want to say-this isn’t about magic pills or quick fixes. This is about giving women who’ve been told for years that they just need to ‘try harder’ or ‘eat less’ a real shot at reclaiming their health. I’ve seen patients cry because they finally ovulated after a decade of trying. That’s not just a lab result-that’s hope. Yes, the cost is insane. Yes, side effects suck. But if you’ve been through the cycle of diets, birth control, and despair, and then you get a tool that lets you breathe again? That’s not a trend. That’s medicine catching up to biology.
And to those saying ‘it’s capitalism exploiting women’-I get it. But sometimes, the tool is good even if the system is broken. We fight the system by demanding access, not by rejecting the only thing that’s actually working. Start low, go slow, eat protein, move your body, and don’t let the cost make you feel like you don’t deserve to feel better.
you people are so naive. this is just another way for big pharma to make billions off women’s pain. they don’t care if you live or die-they care if you keep buying. and now you’re all acting like you’re some kind of hero because you lost weight? you’re not healing, you’re being manipulated. i’ve seen too many women get addicted to these drugs and then crash when they can’t afford them. this isn’t science, it’s a pyramid scheme with needles.
glp-1s are just a band-aid. real change comes from fixing your diet, sleeping better, and reducing stress. if you’re relying on a drug to make you ‘normal,’ you’re already lost. you think losing weight magically fixes everything? congratulations, you’re now a skinny woman with the same hormonal chaos inside. the real problem is we’ve been taught to hate our bodies instead of learning to live in them.
I just want to say-I started semaglutide last year and I lost 31 pounds. My periods came back. I stopped having panic attacks before every doctor’s appointment. I went from being scared to look in the mirror to actually smiling at myself. I know it’s expensive. I know it’s not perfect. But if you’ve ever felt like your body was working against you every single day-this gave me back my life. Not my ‘ideal’ body. Just my body. And that’s worth everything.
To the people saying it’s a scam or a trap-I get it. I was you. I thought I was weak for needing this. But healing isn’t about being tough. It’s about being kind to yourself. And sometimes, kindness comes in the form of a tiny injection. I’m not proud of how I looked before. I’m proud of how I feel now. And that’s enough.