
Every year, more than 1.5 million people in the U.S. are harmed by medications they took exactly as prescribed. That’s not a typo. These aren’t overdoses or street drugs - these are errors made while following a doctor’s orders. And it’s happening in hospitals, pharmacies, and right in your own medicine cabinet.
Medication Errors Are More Common Than You Think
One in every 20 patients worldwide experiences harm from a medication error. That’s 5% of everyone taking pills, injections, or creams. In the U.S. alone, that translates to more than 1.3 million people hurt each year. About 7,000 of those cases end in death - mostly in hospitals. And it’s not just a problem in big cities or poor countries. It’s everywhere.
Think about it: you get a prescription. You take it. You don’t feel worse. So you assume it’s working. But what if the dosage was wrong? What if the pill looked different this time? What if you mixed it with something you didn’t know was dangerous? These aren’t rare mistakes. They’re built into the system.
Which Drugs Are Most Dangerous?
Not all medications carry the same risk. Some are far more likely to cause harm than others. Antibiotics top the list, responsible for about 20% of all medication-related injuries. Why? Because they’re overused, misprescribed, or taken incorrectly. People stop taking them early when they feel better - and that breeds resistant bacteria.
Antipsychotics come in second at 19%. These are often given to elderly patients with dementia, even though they increase the risk of stroke and sudden death. Central nervous system drugs like sedatives and antidepressants follow at 16%. And cardiovascular drugs - blood pressure pills, heart medications - cause 15% of serious errors.
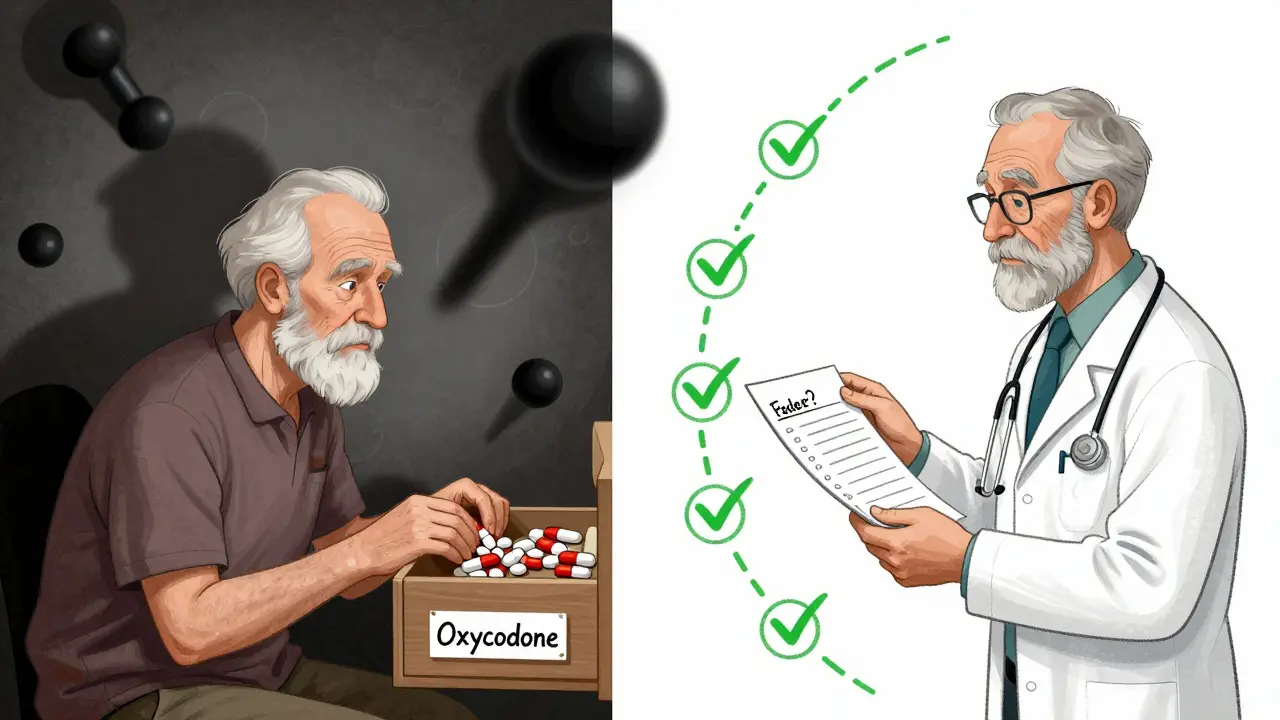
But the scariest trend? Fake drugs. In the U.S., one in three counterfeit pills seized by the DEA are found in North America. Between 2019 and 2021, over half of all opioid overdose deaths involved fake oxycodone laced with fentanyl. In 2023, the DEA seized over 80 million fentanyl-laced counterfeit tablets. These aren’t street drugs - they’re sold as legitimate prescriptions, sometimes even through online pharmacies.
Where Do Errors Happen?
Most people assume mistakes happen in hospitals. And yes, IV medications are the worst offenders - between 48% and 53% of errors happen with injections given directly into the bloodstream. Nurses make errors between 16% and 44% of the time, according to global studies. But here’s the truth: most errors happen after you leave the hospital.
At home, between 2% and 33% of patients make mistakes with their meds. Common ones? Taking the wrong dose, skipping doses, taking two pills by accident, mixing meds with alcohol or grapefruit juice. A Reddit analysis of 1,247 medication posts showed 68% of users were confused about dosage instructions. Another 22% didn’t know what side effects to watch for.
Older adults are especially at risk. In Australia, doctors cut inappropriate antipsychotic use in seniors by 11% over five years - because they realized how often these drugs were being used as chemical restraints instead of real treatment.
Why Do These Mistakes Keep Happening?
It’s not because doctors or pharmacists are careless. It’s because the system is broken.
Dr. Donald Berwick, a top patient safety expert, says: “Most medication errors are system failures, not individual failures.” That means if your doctor writes a prescription in messy handwriting, or your pharmacy fills it with a different brand, or your phone app reminds you at the wrong time - it’s not your fault. It’s the design.
Doctors are rushed. Pharmacists juggle hundreds of prescriptions a day. Nurses are understaffed. Patients get multiple prescriptions from different doctors who don’t talk to each other. And no one checks if all those pills are safe together.
Even technology isn’t fixing everything. Infusion pumps - devices that deliver IV drugs - had over 200,000 reported malfunctions in just 19 months. And 204 of those caused deaths.
What Can You Do to Protect Yourself?
You can’t control the system. But you can control what happens in your hands.
- Keep a living list of every medication you take - including vitamins, supplements, and over-the-counter drugs. Update it every time something changes. Bring it to every appointment.
- Use one pharmacy for all your prescriptions. That way, they can check for dangerous interactions.
- Ask these three questions every time you get a new drug: “What is this for?”, “How and when do I take it?”, and “What side effects should I watch for?” Don’t accept vague answers.
- Check the pills. If your pill looks different than last time - color, shape, markings - ask the pharmacist. It might be a generic, or it might be fake.
- Don’t ignore symptoms. If you feel dizzy, nauseous, confused, or have a rash after starting a new drug, call your doctor. Don’t wait.
Australia’s “5 Moments for Medication Safety” is a simple guide anyone can use:
- When you start a new treatment
- When you add a new medication
- When you move between care settings (hospital to home, doctor to pharmacy)
- When you’re taking high-risk drugs like blood thinners or insulin
- When you review your meds every 6-12 months

The Big Picture: Progress and Danger
There’s good news. More than 130 countries have created national plans to reduce medication harm. Australia cut opioid deaths by 37% since 2018 by tracking prescriptions in real time. The U.S. is rolling out 16 new safety measures for Medicare patients in 2025 - tracking things like statin use in diabetics and antipsychotic use in dementia patients.
But the threats are growing faster. Online pharmacies selling fake drugs are booming. Social media ads push counterfeit pills with no warning. Fentanyl is now the #1 cause of death for Americans aged 18 to 45. And the global market for patient safety tools is expected to hit $14 billion by 2029 - because we’re finally realizing how broken this is.
Artificial intelligence could cut errors by 30% in the next few years by automatically checking drug interactions and flagging dangerous combinations. But that tech won’t help if patients don’t speak up, don’t ask questions, and don’t demand better.
It’s Not Just About Pills - It’s About Power
Medication safety isn’t just a medical issue. It’s a power issue. Patients are expected to follow complex instructions with little support. They’re told to trust the system - even when the system fails them.
You have the right to know what you’re taking. You have the right to ask why. You have the right to see your own records. And you have the right to say no - especially if something doesn’t feel right.
Next time you pick up a prescription, don’t just walk away. Look at the label. Ask the pharmacist. Write it down. Talk to your doctor. That one extra minute could save your life.
How common are medication errors in the U.S.?
More than 1.5 million Americans are harmed by medication errors each year, and about 7,000 of those cases result in death - mostly in hospitals. These errors include wrong doses, drug interactions, and counterfeit medications.
What types of drugs cause the most harm?
Antibiotics cause about 20% of medication-related harm, followed by antipsychotics (19%), central nervous system drugs (16%), and cardiovascular medications (15%). Fake opioids laced with fentanyl are now the deadliest threat, especially among younger adults.
Can I trust my pharmacy to catch errors?
Pharmacists are trained to spot errors, but they’re often overwhelmed. One pharmacy might fill 300+ prescriptions a day. Always double-check your meds - especially if the pill looks different, or if you’re taking multiple drugs. Use one pharmacy for everything so they can track interactions.
Are online pharmacies safe?
No. Nearly one-third of counterfeit drug seizures in the U.S. come from unregulated online sellers. Many pills sold as oxycodone or Adderall are fake and contain deadly fentanyl. Only buy from pharmacies that require a prescription and are licensed in your state.
What should I do if I think I had a medication error?
Stop taking the medication and call your doctor or pharmacist immediately. If you have symptoms like chest pain, trouble breathing, confusion, or severe rash, go to the ER. Report the error to the FDA’s MedWatch program - your report helps track dangerous trends.
How can I reduce my risk at home?
Keep a written list of all your meds - including vitamins and supplements. Use a pill organizer with alarms. Never mix alcohol with prescriptions. Ask your doctor or pharmacist: ‘What is this for?’ ‘How do I take it?’ and ‘What side effects should I watch for?’ If something feels off, trust your gut.









10 Comments
This is insane and we’re doing NOTHING about it. If you’re not screaming about this in your town hall meetings, you’re part of the problem. People are dying because we let corporations and lazy bureaucrats run the system like a broken vending machine. We need federal oversight, NOW.
My grandma took her meds like a soldier and still ended up in the ER because the pharmacy gave her the wrong bottle. They didn’t even apologize. Just said ‘oops.’ Like that’s a thing you say when someone almost dies. This ain’t just bad luck - it’s negligence dressed up as bureaucracy.
Oh honey, let me break this down like I’m explaining it to your uncle who still thinks ‘natural remedies’ cure cancer. Antibiotics? Overused like cheap perfume. Antipsychotics in dementia patients? That’s not treatment - that’s chemical handcuffs. And fake oxycodone laced with fentanyl? That’s not a drug crisis. That’s a genocide disguised as capitalism. You think the DEA’s gonna save you? Nah. They’re busy raiding TikTok influencers selling gummy bears with cyanide. Meanwhile, your pharmacist’s got 120 scripts to fill before lunch and zero time to look you in the eye. You want safety? You gotta become your own damn pharmacist. Write it down. Ask the damn questions. Don’t trust the label - trust your gut. And if you feel weird after popping a pill? STOP. Call someone. Don’t wait for a textbook symptom. Your body’s not broken. The system is.
It is deeply concerning that such systemic failures persist in a nation with the world’s most advanced medical infrastructure. The lack of standardized, interoperable electronic prescribing protocols, coupled with insufficient pharmacist-to-patient ratios, constitutes a gross violation of the duty of care owed to vulnerable populations. One must question the ethical implications of permitting such avoidable morbidity to persist under the guise of ‘market efficiency.’
People need to stop being lazy. If you can’t read the label or remember to take your pills, maybe you shouldn’t be taking them at all. I’ve been on 8 meds for 15 years and I’ve never had an issue - because I use a pill organizer, I write everything down, and I don’t trust anyone but myself. If you’re confused, that’s your fault. Not the system’s. 😔
I’ve worked in a pharmacy for 12 years. We’re not monsters. We’re tired. We’re understaffed. We’re getting yelled at for giving someone a generic instead of the brand they saw on TV. We catch mistakes every day - but we can’t catch them all when we’re running on fumes. Please don’t blame us. Advocate for us. Push for better staffing. We want to help.
My mom had a stroke after a new blood pressure med was mixed up with her old one. They didn’t even check if she was on anything else. I cried for three days. But here’s what saved us: we started using one pharmacy, wrote everything on a whiteboard taped to the fridge, and asked every single question - even the dumb ones. It’s not magic. It’s just paying attention. You don’t need a degree. You just need to care enough to ask.
take your meds like you mean it. write it down. dont trust the color. ask why. if you feel weird? stop. call. you dont need to be smart. just be awake.
I’m from India and we don’t have fancy systems here - but we have family. My aunt takes 10 pills a day, and my cousin checks them every morning, writes the dates, calls the doctor if something looks off. No app. No barcode. Just love and attention. Maybe the answer isn’t more tech… maybe it’s more people who care enough to show up.
While the aforementioned statistical framework elucidates a concerning trend in iatrogenic harm, it is imperative to acknowledge that the prevailing paradigm of pharmacovigilance remains fragmented across institutional boundaries. The implementation of AI-driven decision-support systems, integrated with real-time EHR interoperability and standardized medication reconciliation protocols, may mitigate up to 30% of preventable adverse drug events - provided that regulatory agencies enforce mandatory compliance thresholds and allocate sufficient funding to frontline clinical personnel.