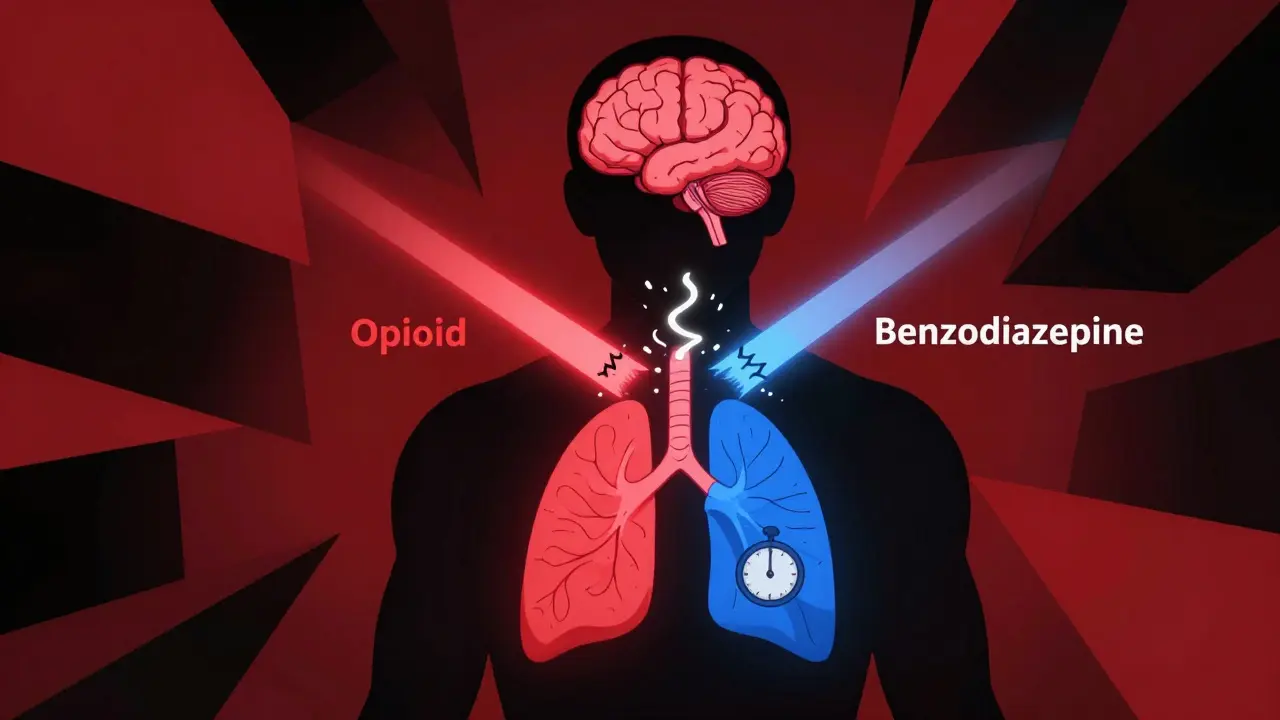
When you take opioids and benzodiazepines together, your breathing doesn’t just slow down-it can stop. This isn’t a hypothetical risk. It’s a real, documented, and often fatal outcome that happens more often than most people realize. In 2020, 16% of opioid-related overdose deaths in the U.S. involved benzodiazepines. That’s nearly one in six. And for people taking both drugs, the chance of dying from an overdose is up to 10 times higher than if they were taking opioids alone.
Why This Combination Is So Dangerous
Opioids like oxycodone, hydrocodone, and fentanyl work by binding to mu-opioid receptors in the brainstem, the part that controls automatic breathing. Benzodiazepines like alprazolam, lorazepam, and diazepam boost the effect of GABA, a calming neurotransmitter that also suppresses brain activity, including the signals that tell you to breathe. When taken separately, each drug can cause drowsiness or shallow breathing. But together? They don’t just add up-they multiply. The combination doesn’t just make you sleepy. It shuts down your body’s ability to respond to rising carbon dioxide levels in your blood. That’s the signal your brain uses to say, “You need to breathe harder.” When that signal gets drowned out, your breathing slows, then stops-often while you’re asleep. A 2021 study in the Annals of Palliative Medicine found that 85% of people who took both drugs together dropped their blood oxygen levels below 90%, compared to just 45% who took opioids alone. That’s not a minor dip. That’s a medical emergency waiting to happen.Who’s at Risk-and Why It’s Not Just About Abuse
Many assume this danger only affects people who misuse drugs. But the truth is, most of these deaths happen to people taking prescriptions exactly as directed. Think about an older adult with chronic pain and anxiety. Their doctor prescribes oxycodone for back pain and alprazolam for panic attacks. Neither drug is illegal. Neither is taken in excess. But together, they create a perfect storm. The FDA warned in 2019 that even patients who’ve been on opioids for years aren’t protected. Tolerance to opioids doesn’t mean tolerance to benzodiazepines. Your body adapts to one, but not the other. So you might feel fine during the day-until you fall asleep. The American Geriatrics Society lists this combination as potentially inappropriate for older adults in their Beers Criteria. Why? Because seniors are more sensitive to both drugs, have slower metabolism, and are more likely to fall or suffer respiratory arrest. Even young, healthy adults aren’t safe. A 2022 study in JAMA Network Open found that 15% of Medicare Part D patients on long-term opioids were also prescribed benzodiazepines. In 4.3% of cases, they were given high-risk combinations-extended-release opioids with long-acting benzos. That’s not rare. That’s common.How the Body Breaks Down These Drugs-And Why That Makes It Worse
Some opioids, like fentanyl, methadone, and oxycodone, are broken down by an enzyme called CYP3A4. Certain benzodiazepines, including alprazolam and midazolam, block this same enzyme. So when you take them together, your body can’t clear the opioid fast enough. The opioid builds up in your bloodstream, even if you’re taking the same dose you’ve always taken. This isn’t theoretical. Emergency rooms see patients who took their normal oxycodone dose and a single alprazolam tablet-and ended up in respiratory arrest. The drugs didn’t change. Their interaction did. Pfizer’s labeling for lorazepam injection notes that while healthy volunteers didn’t show reduced sensitivity to carbon dioxide at standard doses, airway obstruction occurred in rare cases when patients were excessively sedated. That’s the key word: excessively. And “excessive” doesn’t mean “high dose.” It means “combined with another depressant.”
What Happens During an Overdose
The signs aren’t always obvious. You might not see someone gasping or thrashing. Often, it’s quiet. Symptoms include:- Extreme drowsiness or inability to wake up
- Slow, shallow, or irregular breathing
- Blue lips or fingernails
- Cold, clammy skin
- Confusion, slurred speech, or unresponsiveness
What Doctors Are Supposed to Do-And What Often Goes Wrong
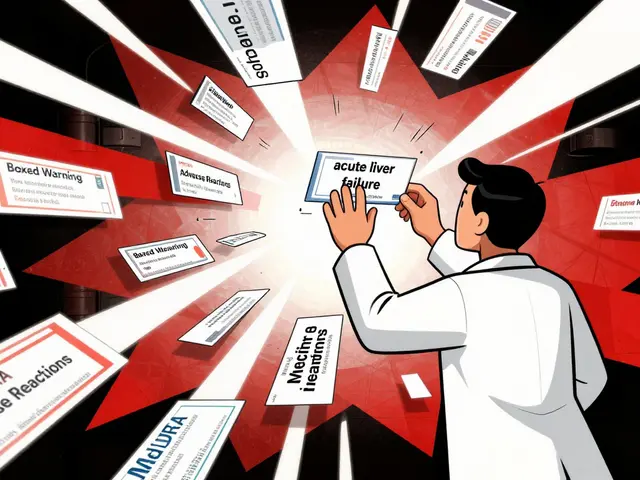
The FDA’s 2019 update mandated a Boxed Warning on all opioid and benzodiazepine labels-the strongest warning they can issue. It says clearly: combining these drugs can cause coma or death. Guidelines from the CDC and the FDA agree: avoid prescribing them together whenever possible. If absolutely necessary, start with the lowest possible dose of each. Monitor closely. Educate patients and caregivers. But in practice, it doesn’t always happen. A 2021 study found that even after the FDA’s warnings, many prescribers still didn’t adjust dosing. Some assumed patients on opioids needed higher benzo doses because they were “tolerant.” That’s a deadly myth. Tolerance to one drug doesn’t protect against the other. Electronic health record systems now often flag dangerous combinations. One study showed alerts reduced inappropriate co-prescribing by 27.3%. That’s progress. But it’s not enough. Many patients still get these prescriptions without ever being warned.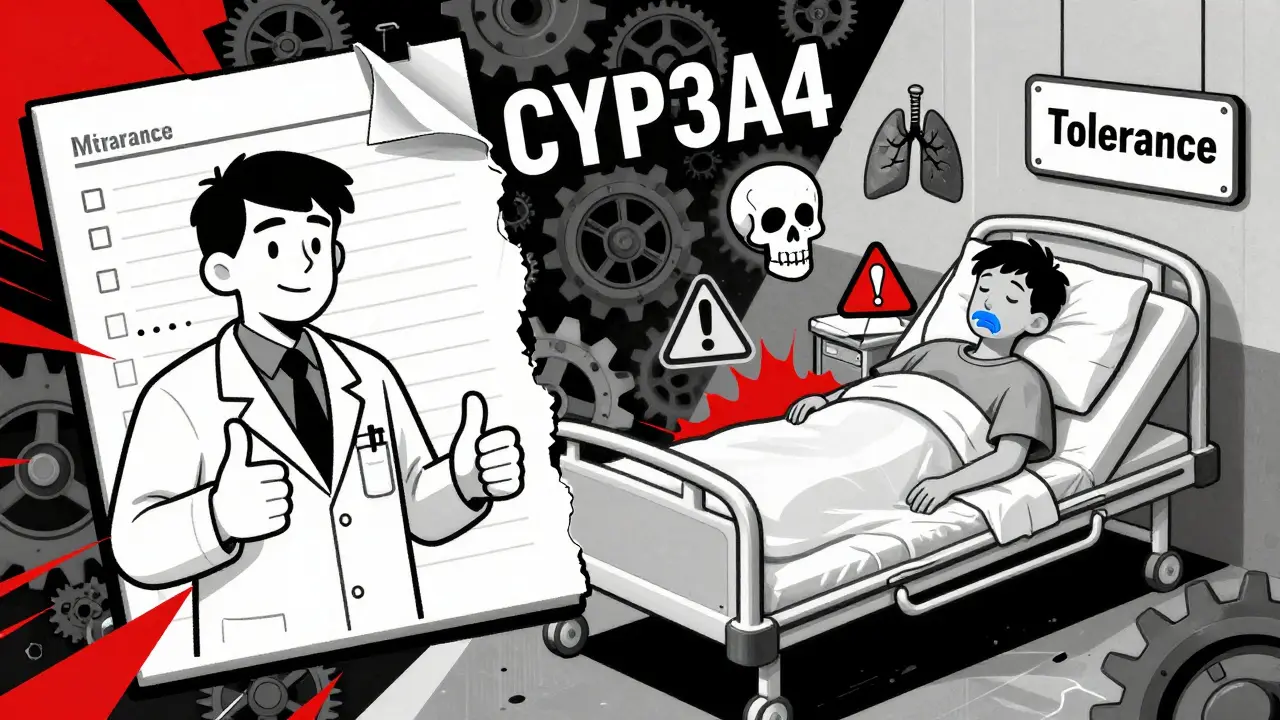
What to Do If You’re Already Taking Both
If you’re on opioids and benzodiazepines right now, don’t stop suddenly. Withdrawal from either can be dangerous. Opioid withdrawal causes nausea, sweating, and anxiety. Benzodiazepine withdrawal can trigger seizures. Talk to your doctor. Ask:- Is this combination absolutely necessary?
- Can one of these drugs be replaced with something safer?
- What’s the lowest dose I can take?
- Do I have a naloxone kit? (It won’t reverse benzodiazepine effects, but it can help if opioids are involved.)
- Have I told my family or caregiver about the risks?
What’s Being Done-and What’s Next
In 2022, the CDC awarded a research grant to UC Davis specifically to study the combined risks of opioids and benzodiazepines. Why? Because we still don’t fully understand who’s most at risk-or how to predict it. Researchers are looking at genetic factors, sleep patterns, and lung function to build better risk models. Meanwhile, hospitals and clinics are starting to use decision-support tools that block prescriptions when dangerous combinations are detected. The long-term goal? Safer pain and anxiety treatments that don’t shut down breathing. Until then, the message is simple: if you don’t need both, don’t take both.Final Warning: This Isn’t a Risk You Can Guess Your Way Out Of
You can’t tell how your body will react just by feeling “fine.” You can’t assume tolerance protects you. You can’t rely on a single dose being “safe.” This interaction doesn’t care about your age, your health, or your intentions. It only cares about chemistry. And that chemistry is deadly. If you’re prescribed both, ask questions. If you’re caring for someone who takes both, learn the signs of overdose. Keep naloxone nearby. And never, ever assume it won’t happen to you.Can you overdose on opioids and benzodiazepines even if you take them as prescribed?
Yes. Many overdose deaths occur in people who take both drugs exactly as directed by their doctor. The danger comes from how the drugs interact in the body-not from taking too much of either one. Even standard doses can cause respiratory depression when combined.
Does naloxone work if someone overdoses on both opioids and benzodiazepines?
Naloxone can reverse the effects of opioids, which may help restore breathing. But it does not reverse benzodiazepine effects. If someone overdoses on both, naloxone can be life-saving, but it’s not a complete solution. Emergency medical care is still urgently needed.
Why don’t doctors just stop prescribing these together?
Some do. But others still prescribe them together because they believe the patient needs both-for pain and anxiety, for example. The problem is, safer alternatives exist for anxiety, like SSRIs or therapy, and non-opioid pain options are growing. Many prescribers haven’t caught up with the latest safety guidelines.
Are there any situations where using both is considered safe?
In rare cases, such as end-of-life care in hospice, the benefits of comfort and symptom control may outweigh the risks. Even then, doses are kept extremely low and closely monitored. For anyone else, the risks far outweigh any potential benefit.
What should I do if I’m worried a loved one is taking both drugs?
Talk to them calmly. Ask if they’ve been warned about the risks. Check if they have a naloxone kit. Encourage them to speak with their doctor about alternatives. If they show signs of extreme drowsiness or slowed breathing, call emergency services immediately. Don’t wait.








8 Comments
Yeah right like the government actually cares if you die from your meds. They just want you hooked on something so they can keep selling it. I know a guy who got benzos and oxy for back pain and now he’s on methadone. Classic scam.
Stop crying and get a job
The pharmacodynamics here are textbook GABAergic and mu-opioid receptor synergy-synergistic respiratory depression isn’t some fringe theory, it’s basic neuropharmacology. The FDA’s boxed warning exists because the data is irrefutable. Yet we still have clinicians prescribing this combo like it’s a coffee and donut special. The real tragedy isn’t the interaction-it’s the institutional failure to prioritize harm reduction over convenience.
i had a cousin on both and he swears he felt fine but his wife said he’d zone out for like 20 mins then snap back like nothing happened. they never told the doc. now he’s on gabapentin and cbt and says he feels better than ever. guess the system just wants you to stay sick
It is profoundly disturbing that in the United States of America, a nation that prides itself on medical innovation and patient safety, we continue to permit the co-prescription of two classes of central nervous system depressants whose lethal interaction has been documented for decades. The fact that this remains a common clinical practice-not an anomaly, but a routine occurrence-speaks not to medical necessity, but to systemic negligence, inadequate physician education, and the commodification of healthcare. Patients are not data points. They are human beings whose respiratory function should not be treated as a statistical afterthought.
Oh look, another ‘educational’ post from someone who clearly never had to choose between pain and panic attacks. Let me guess-you’ve never been prescribed a benzo, never had a surgery, never had a sleepless night because your body feels like it’s dissolving? The real danger isn’t the drugs-it’s the smug, self-congratulatory virtue signaling that pretends to care while offering zero solutions. Maybe if you spent less time lecturing and more time advocating for accessible mental healthcare, we wouldn’t be in this mess.
they say dont mix but then they give you both on the same day like its normal. my dr said ‘its fine if you dont take em at the same time’ like that’s how it works. no its not. your liver dont care what time you took em. it just sees both and shuts down. i got lucky
THIS IS A BIG PHARMA COVERUP. THEY WANT YOU DEPRESSED AND DROWSY SO YOU’LL KEEP BUYING MORE DRUGS. THE FDA IS IN BED WITH PFEIZER. THEY KNOW THIS KILLS PEOPLE. THEY’RE WAITING FOR YOU TO FALL ASLEEP AND NEVER WAKE UP SO THEY CAN SELL MORE NALOXONE. THEY’RE MAKING BILLIONS OFF THIS. THEY EVEN PUT IT IN THE LABELS ON PURPOSE SO THEY CAN SAY ‘WE WARNED YOU’ AND STILL PROFIT. THIS IS A GENOCIDE. YOU THINK YOUR DOCTOR CARES? THEY GET BONUSES FOR PRESCRIBING THESE.