
Statin-Antifungal Interaction Checker
Check if your statin medication interacts dangerously with common antifungal drugs. This tool helps you identify potential risks and gives specific recommendations for safe medication use.
Interaction Result
Symptoms to Watch For
- Severe muscle pain (shoulders, thighs, lower back)
- Extreme muscle weakness
- Dark, tea-colored urine
- Nausea or fever
What to Do
When you take a statin to lower your cholesterol, you’re not just managing heart risk-you’re trusting your body to handle that drug safely. But add a common antifungal like fluconazole or itraconazole for a yeast infection, and suddenly, that safety net can vanish. The result? A rare but deadly condition called rhabdomyolysis, where muscle tissue breaks down so fast it floods your bloodstream, potentially crashing your kidneys. This isn’t theoretical. It happens. And it’s preventable-if you know what to look for.
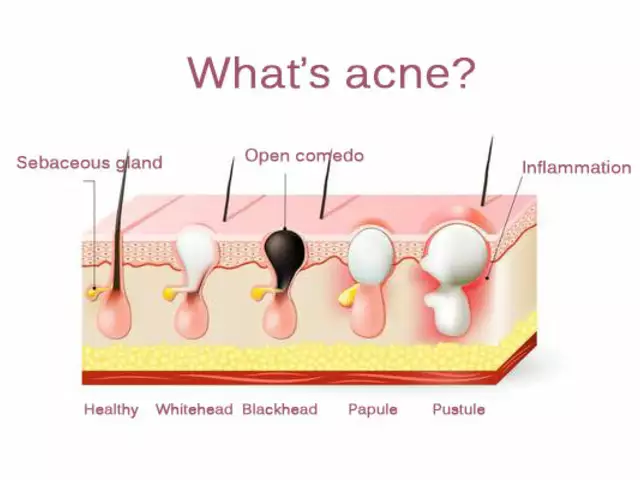
Why This Interaction Is So Dangerous
Statins like simvastatin, lovastatin, and atorvastatin don’t just float around in your blood. Your liver uses an enzyme called CYP3A4 to break them down and flush them out. Azole antifungals-used for everything from athlete’s foot to vaginal yeast infections-shut down that enzyme like flipping a switch. When CYP3A4 is blocked, statins pile up in your system. No one designed this. It’s just how chemistry works.Take simvastatin. At normal doses, it’s fine. But when you add itraconazole, your body ends up with ten times more of the drug than it should. That’s not a typo. That’s 1,160% higher exposure. For some people, that’s enough to trigger muscle damage within days. The same thing happens with lovastatin and voriconazole. Even fluconazole, which is considered a weaker inhibitor, can push simvastatin levels up by 350% when taken at 400 mg daily.
Which Statins Are Riskiest?
Not all statins are created equal when it comes to this interaction. Your risk depends entirely on how your body processes them.- High risk: Simvastatin, lovastatin, atorvastatin-all heavily broken down by CYP3A4. Simvastatin is the worst offender. A 2016 meta-analysis found the relative risk of muscle damage jumps to 22.3 when simvastatin is taken with itraconazole.
- Moderate risk: Pitavastatin and atorvastatin still get affected, but the rise in blood levels is less extreme. Still dangerous at high doses.
- Low risk: Pravastatin, fluvastatin, rosuvastatin. These use different pathways. You can usually take them safely with antifungals, even at full doses.
If you’re on simvastatin 40 mg or higher and your doctor prescribes itraconazole, you’re in the danger zone. The FDA banned this combo in 2012. Yet, a 2022 study found nearly 1 in 5 patients still get this dangerous pairing-especially older adults in outpatient clinics.
Real Cases, Real Consequences
A 68-year-old man in Australia was prescribed fluconazole for a stubborn toenail fungus. He’d been on simvastatin 40 mg for five years with no issues. Seven days after starting the antifungal, he couldn’t get out of bed. His muscles ached like he’d run a marathon without training. His urine turned dark brown. His creatine kinase (CK) level-normally under 200 U/L-shot up to 18,400 U/L. He spent three days in the hospital. He didn’t die, but he lost weeks of mobility. That case? It’s not rare.Pharmacists on Reddit report seeing 2-3 cases per year. The FDA’s adverse event database logged over 1,200 rhabdomyolysis cases tied to statin-azole combos between 2010 and 2019. Simvastatin with itraconazole made up nearly 40% of those. Simvastatin with fluconazole? Almost 30%. The symptoms are always the same: crushing muscle pain, weakness, and dark urine. Most people notice it within 7-14 days of starting the antifungal.

What Doctors Should Do
Good prescribers don’t guess. They check. Here’s what the guidelines say:- Stop simvastatin and lovastatin completely if you’re taking ketoconazole, itraconazole, or voriconazole. Don’t just lower the dose. Stop it. Restart only 2-3 days after the antifungal ends.
- Cap simvastatin at 10 mg daily if you must take fluconazole. No exceptions.
- Switch to a safer statin: Pravastatin 40 mg, fluvastatin 80 mg, or rosuvastatin 20 mg can usually be continued without adjustment.
- Check CK levels before starting the combo, then weekly during treatment. If CK is over 10 times the upper limit, stop the statin immediately.
Many hospitals now have electronic alerts that block prescriptions. Mayo Clinic’s Epic system stopped 87% of unsafe combinations after adding hard stops. That’s not magic. It’s basic safety engineering.
Newer Antifungals Offer Safer Options
There’s good news: not all antifungals are created equal. Isavuconazole, approved in 2015, barely touches CYP3A4. Studies show it doesn’t raise simvastatin levels at all. If you need long-term antifungal therapy-say, for a chronic fungal lung infection-isavuconazole is now the preferred choice over itraconazole or voriconazole.Even better? Some newer drugs are being designed with this interaction in mind. Researchers are also looking at genetics. People with a CYP3A5*3/*3 genotype (about 70% of Caucasians) break down statins slower naturally. Add an antifungal? Their risk doubles. Future guidelines may include genetic testing for high-risk patients.

What You Should Do Right Now
If you’re on a statin and your doctor just prescribed an antifungal, don’t wait. Ask these three questions:- Is this antifungal an azole? (Ketoconazole, itraconazole, voriconazole, fluconazole, posaconazole-yes, they’re all azoles.)
- Which statin am I on? (Check the bottle. Simvastatin? Lovastatin? Atorvastatin? That’s the red flag group.)
- Can we switch to pravastatin, fluvastatin, or rosuvastatin instead?
If you’re already on simvastatin and fluconazole, don’t panic-but don’t ignore it either. Muscle pain that feels worse than normal soreness? Dark urine? Weakness? Call your doctor today. Rhabdomyolysis isn’t something you wait to see if it gets better. It’s an emergency.
The Bigger Picture
This isn’t just about two drugs. It’s about how fragmented our healthcare system is. A cardiologist prescribes the statin. A dermatologist prescribes the antifungal. The pharmacist doesn’t always catch it. The patient doesn’t know to ask. And with 36 million Americans on statins and 15-20 million azole prescriptions written every year, the chances of overlap are huge.The good news? We’ve gotten better. Between 2015 and 2022, rhabdomyolysis cases from this interaction dropped by 34%. Why? Better alerts. Better guidelines. More awareness. But it’s still happening. Too often. To people who didn’t have to die.
You don’t need to be a doctor to protect yourself. Know your meds. Ask questions. Speak up. Your muscles-and your kidneys-depend on it.
Can I take fluconazole with my statin?
It depends on which statin you’re taking. If you’re on simvastatin or lovastatin, fluconazole can be dangerous-even at low doses. The FDA recommends no more than 10 mg of simvastatin daily if you must take fluconazole. For atorvastatin, stay under 20 mg daily. If you’re on pravastatin, fluvastatin, or rosuvastatin, fluconazole is generally safe at standard doses. Always check with your doctor or pharmacist before combining them.
What are the signs of rhabdomyolysis?
The main signs are severe muscle pain (especially in the shoulders, thighs, or lower back), extreme weakness, and dark, tea-colored urine. You might also feel nauseous or have a fever. These symptoms usually show up within a week or two of starting the antifungal. If you notice any of these, stop taking your statin and seek medical help immediately. High creatine kinase levels can lead to kidney failure.
Is it safe to take statins with over-the-counter antifungals?
Yes, but only if they’re topical-like creams or sprays for athlete’s foot. Oral antifungals, even those sold without a prescription, are dangerous with certain statins. Many people don’t realize that fluconazole tablets (sometimes sold for yeast infections) are oral and carry the same risk as prescription versions. Always read the label. If it’s a pill you swallow, assume it interacts with statins unless confirmed otherwise.
Why is simvastatin more dangerous than other statins?
Simvastatin is almost entirely broken down by the CYP3A4 enzyme. When an azole antifungal blocks that enzyme, simvastatin can’t leave your system. It builds up fast. Other statins like pravastatin or rosuvastatin use different pathways, so they aren’t affected the same way. Simvastatin also has a narrow safety margin-meaning the difference between a therapeutic dose and a toxic one is small. That’s why even a small increase in blood levels can cause muscle damage.
Can I switch statins to avoid this interaction?
Yes, and it’s often the best solution. Pravastatin, fluvastatin, and rosuvastatin are not significantly affected by CYP3A4 inhibitors. Your doctor can switch you to one of these while you’re on an antifungal. You’ll still get the same cholesterol-lowering benefits without the muscle risk. Many patients stay on these alternatives long-term because they’re safer overall, especially if you’re older or taking multiple medications.
How long does the interaction last after stopping the antifungal?
CYP3A4 inhibition can last for days after you stop the antifungal. For itraconazole and voriconazole, it can take up to a week for the enzyme to fully recover. That’s why doctors recommend waiting 2-3 days after finishing the antifungal before restarting simvastatin or lovastatin. Don’t restart sooner just because you feel fine. The drug is still in your system, and the risk doesn’t disappear overnight.
Are there any antifungals that are safe with all statins?
Yes. Isavuconazole is the only newer azole antifungal that doesn’t significantly inhibit CYP3A4. Studies show it doesn’t raise levels of simvastatin, atorvastatin, or other CYP3A4-metabolized statins. If you need long-term antifungal treatment, isavuconazole is now the preferred option for patients on statins. Topical antifungals (creams, lotions, sprays) are also safe because they don’t enter your bloodstream in significant amounts.
If you’re on a statin and need an antifungal, don’t assume it’s fine. Ask your doctor to check for interactions. Use tools like Medscape or Epocrates if you’re tech-savvy. Or just call your pharmacist. They’re trained for this. You don’t have to be.





15 Comments
Just got prescribed fluconazole for a yeast infection and I’m on simvastatin-this post literally saved me from a hospital trip. I called my pharmacist before taking it and they switched me to rosuvastatin same day. Don’t wait until your muscles feel like they’re melting. Ask questions. You’re worth it.
Okay but like… why are we treating statins like they’re radioactive? I mean, people used to take them with grapefruit juice and nobody died. Now we’re acting like fluconazole is the devil’s juice. Also, I’ve been on simvastatin and fluconazole for 3 years. I’m fine. Your fear is making me mad 😤
It is imperative to underscore the clinical significance of this pharmacokinetic interaction. The cytochrome P450 3A4 pathway is not merely a metabolic conduit-it is a critical gatekeeper in drug disposition. The concomitant administration of azole antifungals with CYP3A4-metabolized statins constitutes a documented hazard, as evidenced by peer-reviewed literature and regulatory advisories. Prudent clinical practice demands substitution with non-CYP3A4 substrates, such as pravastatin or rosuvastatin, to mitigate the risk of rhabdomyolysis. This is not a matter of opinion-it is standard of care.
I’ve been thinking about how we treat our bodies like machines that just need the right code to run. But this? This isn’t a bug-it’s a design flaw we didn’t know about. Like, we’re giving people drugs that were never meant to be used together, and then acting shocked when things break. Maybe we need to stop treating medicine like a menu and start treating it like a symphony. One wrong note and the whole thing collapses. And honestly… I think we’re still too loud in the orchestra.
This is why I love the NHS-pharmacists here are legally required to flag these combos. I had a mate on simvastatin get fluconazole and the pharmacy refused to dispense it until his GP changed it. No drama, no guesswork. Why can’t the US do this? We’re not asking for magic, just basic safety checks. 🇬🇧
Okay but isn’t this just another way for Big Pharma to scare people into buying ‘safer’ statins? Like… I get it, but also… people have been taking these combos for decades and most didn’t die. I think we’re overmedicalizing normal biology. Also, why is simvastatin the villain? Maybe it’s just the most popular, not the most dangerous. 🤷♀️
Given the CYP3A4-mediated pharmacokinetic interplay, the concomitant administration of azole antifungals with simvastatin represents a Class I drug-drug interaction with a documented relative risk of 22.3 for myotoxicity per the 2016 meta-analysis referenced. The absence of routine CK monitoring in outpatient settings constitutes a systemic failure in risk mitigation protocols. Furthermore, the persistence of this interaction in 19% of cases per 2022 data suggests a critical gap in prescriber education and EHR integration. The burden of proof lies not with the patient, but with the healthcare infrastructure.
Look, I get it. But this is why America’s healthcare is broken. You got some doctor in California prescribing fluconazole and another in Texas prescribing statins and no one talks. Meanwhile in Russia, they just give you one pill and tell you to shut up. We overthink everything. Just take the damn statin. You’ll be fine. I’m 52 and I’ve taken both for 4 years. No problems. Probably just weak Americans.
THIS IS WHY YOU ASK YOUR PHARMACIST 😭 I literally had this happen to my aunt-dark urine, couldn’t walk, ICU for 3 days. Now I check every single med combo on Drugs.com before I take anything. And yes, I use emojis because I’m not a robot. 💉🩸🆘
so like… fluconozole? is that the one you take for yeast? and statins are for cholestrol right? i was on both and i felt weird but i thought it was just stress. now im scared. i think i need to call my doc. thanks for the warning lol
just wanted to say i switched from simvastatin to pravastatin last year after reading this kind of stuff. best decision ever. no more muscle aches, no more panic when i get a cold. also i spelled pravastatin wrong in my notes but my pharmacist knew what i meant. thanks for the info, this helped me out.
It is, indeed, a veritable pharmacological minefield-particularly when one considers the heterogeneity of patient populations, the non-uniformity of EHR alert systems, and the lamentable lack of standardized pharmacogenomic screening. One cannot help but observe that the persistence of this interaction, despite FDA warnings since 2012, reflects a systemic dereliction of duty on the part of prescribers, institutions, and, yes, even patients who refuse to engage with their own health data. This is not a ‘risk’-it is a failure of accountability.
I keep thinking about how we’ve built this entire system on trust-trust in doctors, in pharmacies, in labels. But when two perfectly legal, commonly prescribed drugs can silently destroy your muscles… maybe trust isn’t enough. Maybe we need systems that force confirmation, not just reminders. Maybe we need to stop treating patients like they’re just data points and start treating them like people who deserve to be protected-even if they don’t know enough to ask.
Isavuconazole is the real MVP here. I’m a pharmacist and I’ve been pushing it for my high-risk statin patients since 2020. It’s pricier, sure, but when you compare it to the cost of a hospitalization for rhabdo? It’s a steal. Also, CYP3A5*3/*3 genotype carriers? They’re the ones you really need to watch. We’re not even testing for it. That’s lazy. Let’s fix that.
I read this before my appointment yesterday. Asked my doc about switching statins. She said yes, no problem. We switched me to rosuvastatin. I didn’t know I could ask. I’m just glad I did. Thanks for writing this. 🌿