Bronchodilators: What They Are, How They Work, and Which Ones Actually Help
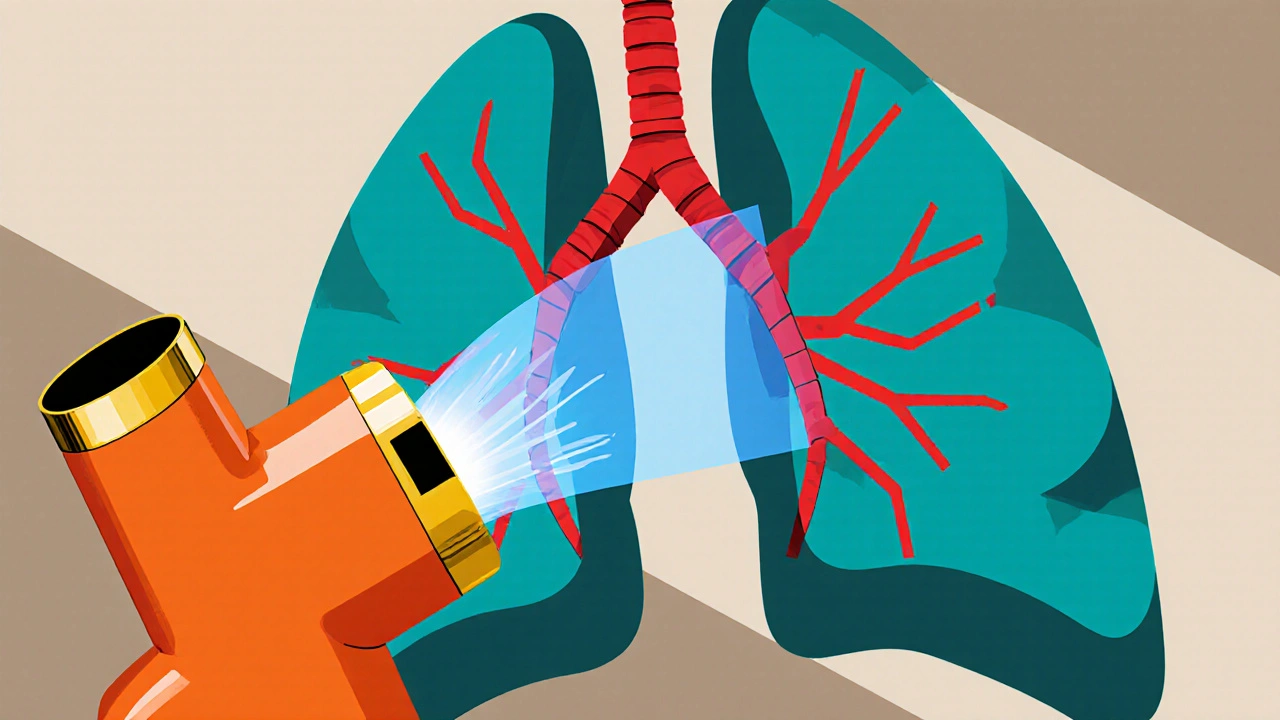
When your airways tighten up—whether from asthma, COPD, or a bad flare-up—you need something to open them back up. That’s where bronchodilators, medications that relax the muscles around your airways to improve airflow. Also known as airway relaxants, they’re one of the most common tools doctors use to help people breathe again. These aren’t just inhalers you grab when you feel tight. They’re a whole category of drugs with different styles, speeds, and uses. Some work fast for sudden attacks. Others are meant to be used every day to keep things under control. Knowing the difference can save you from unnecessary side effects or worse, a trip to the ER.
Bronchodilators fall into two main groups: beta-agonists, drugs that stimulate receptors in the lungs to loosen airway muscles and anticholinergics, medications that block signals that cause airway tightening. Albuterol is the classic beta-agonist—you’ve probably heard of it. It kicks in within minutes and lasts 4 to 6 hours. Then there’s salmeterol, a longer-acting version meant for daily use, not emergencies. Anticholinergics like ipratropium and tiotropium work differently. They don’t speed up your heart like beta-agonists can, which makes them safer for older patients or those with heart issues. Many people now use combo inhalers that mix both types for better control.
These drugs aren’t one-size-fits-all. Someone with mild asthma might only need an inhaler before exercise. Someone with advanced COPD could be on two or three different bronchodilators daily, plus steroids. The key is matching the drug to the problem. Overusing quick-relief inhalers? That’s a red flag your long-term treatment isn’t working. Relying only on long-acting ones without a rescue inhaler? That’s risky. And mixing them wrong? Could lead to tremors, fast heartbeat, or worse.
The posts below dig into real-world comparisons and practical advice. You’ll find clear breakdowns of how different bronchodilators stack up against each other, what side effects to watch for, and how to use them safely with other meds. Some posts even cover how these drugs interact with heart conditions, antibiotics, or even mental health treatments. There’s no fluff here—just facts you can use to talk smarter with your doctor, avoid dangerous mix-ups, and take back control of your breathing.
How Bronchodilators Transform COPD Treatment: Benefits, Types, and Best Practices
Explore how bronchodilators work, their different classes, and step‑by‑step guidance for using them in COPD treatment, plus safety tips and future tech.
read more




