Drug Interaction: What You Need to Know About Medication Conflicts
When you take more than one medicine, your body doesn’t always treat them like separate guests—it sees them as roommates who might fight over space, resources, or attention. This is what we call a drug interaction, a change in how a drug works when combined with another drug, food, supplement, or medical condition. Also known as medication interaction, it’s not just about pills clashing—it’s about your liver, kidneys, and gut getting overwhelmed or misled. Think of it like traffic: one drug might slow down another’s path through your system, or block its exit, or even trick your body into thinking it’s getting more or less than it should.
Some interactions are silent killers. Warfarin, for example, can turn deadly if paired with certain antibiotics or even grapefruit juice—your blood thins too much, and you risk internal bleeding. Metformin and contrast dye? That combo can trigger lactic acidosis if your kidneys aren’t filtering right. Even something as simple as cefuroxime or minocycline can behave differently if you’re also taking antacids or iron pills. These aren’t rare edge cases—they’re everyday risks, especially for people juggling three or more prescriptions. The pharmacokinetics, how your body absorbs, moves, breaks down, and gets rid of drugs is a delicate balance, and one wrong turn can throw it off.
It’s not just about what’s in the bottle. Supplements like St. John’s wort can slash the effectiveness of antidepressants. Herbal teas, calcium pills, even high-fiber meals can interfere with how your body takes in meds. And genetics? That’s another layer. Variants in genes like CYP2C9 and VKORC1 make some people ultra-sensitive to warfarin—testing before starting can cut bleeding risk by over 30%. Your doctor doesn’t always know every possible combo, so you have to speak up. Keep a list of everything you take—prescriptions, OTCs, vitamins, teas—and bring it to every appointment. Don’t assume it’s safe just because it’s natural or over-the-counter.
What you’ll find below isn’t a textbook. It’s real-world stories from people who’ve been there: swelling from meds, hair loss from carbamazepine, QT prolongation from antidepressants, fertility changes from hydroxyurea. Each post breaks down a specific interaction, explains why it matters, and tells you what to do next. No fluff. No jargon. Just clear, practical advice you can use today.
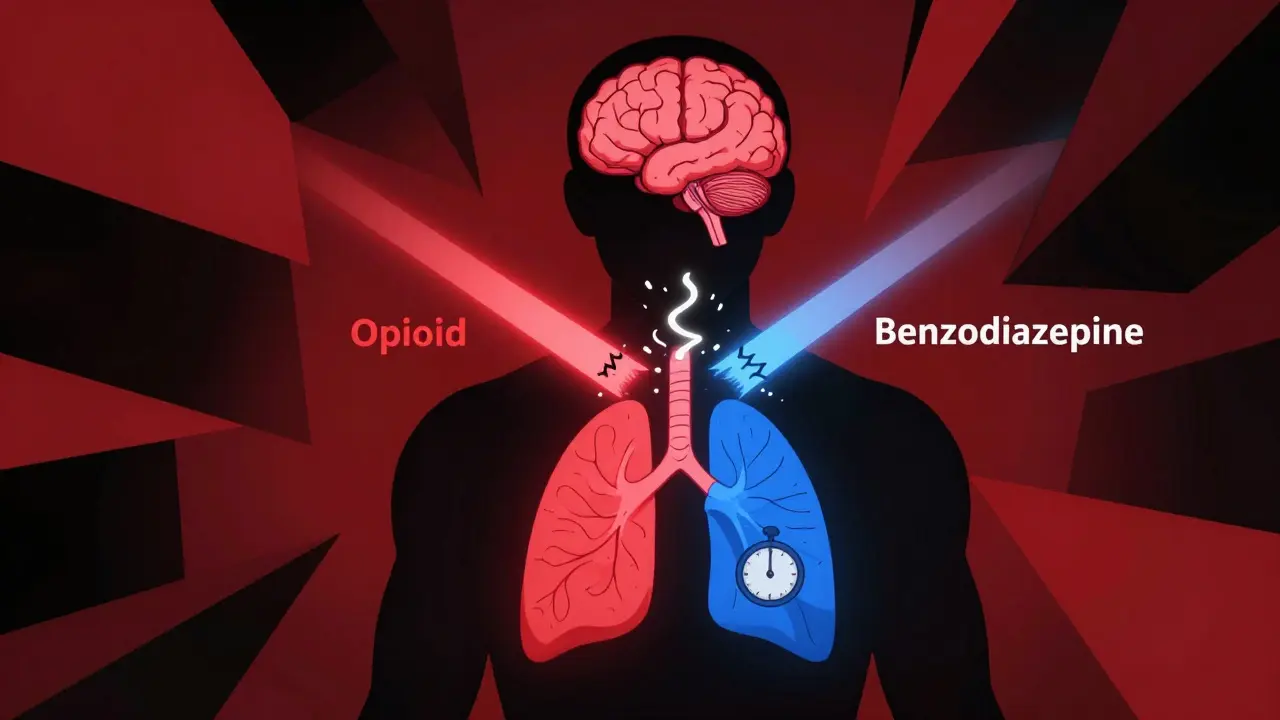
Opioids and Benzodiazepines: The Deadly Breathing Risk When Used Together
Taking opioids and benzodiazepines together can stop your breathing-even at normal doses. Learn why this combination is deadly, who’s at risk, and what to do if you’re already taking both.
read more
Statins and Antifungal Medications: How Their Interaction Raises Rhabdomyolysis Risk
Statins and certain antifungal medications can dangerously interact, increasing the risk of rhabdomyolysis-a life-threatening muscle breakdown. Learn which combinations to avoid, safer alternatives, and what to do if you're taking both.
read more




