Long-Acting Bronchodilators: What They Are, How They Work, and Which Ones Work Best
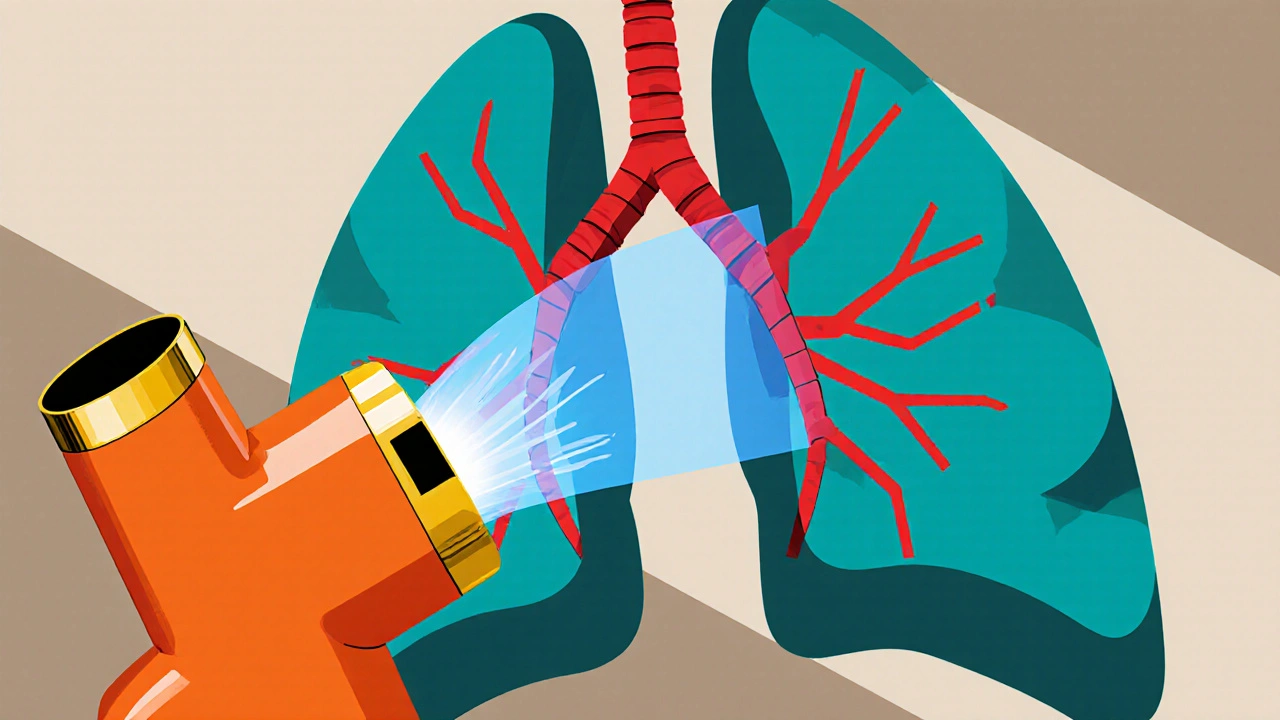
When your airways tighten up and breathing feels like trying to suck air through a straw, long-acting bronchodilators, medications that relax and open the airways for 12 hours or more. Also known as LABAs, they’re not quick fixes—they’re the steady backbone of daily control for people with COPD and persistent asthma. Unlike short-acting inhalers you reach for during a flare-up, these work quietly in the background, keeping your lungs open so you can move, sleep, and breathe without constant worry.
They don’t work alone. Most people use them with inhaled corticosteroids to tackle both inflammation and airway tightness. You’ll find them in combo inhalers like Advair, Symbicort, or Breo—devices that mix a long-acting beta-agonist, a type of bronchodilator that stimulates receptors to relax smooth muscle in the airways with a steroid. But there are also standalone LABAs like salmeterol and formoterol, and another class called long-acting muscarinic antagonists, drugs that block signals causing airway constriction, like tiotropium and aclidinium. These are often called LAMAs, and they’re especially helpful for COPD patients who don’t respond well to beta-agonists.
What makes one better than another? It’s not about being stronger—it’s about fitting your body. Some people respond better to formoterol’s faster start, while others need tiotropium’s all-day hold. Side effects like dry mouth, tremors, or a racing heart aren’t rare, but they’re usually mild and fade with time. The big question isn’t which drug is the best—it’s which one keeps you breathing easiest without extra trips to the ER.
These aren’t magic pills. They won’t cure your condition, but they can turn daily struggles into manageable routines. If you’re on one, you’ve probably learned the rhythm: morning puff, evening puff, rinse your mouth, don’t skip. And if you’re wondering why your doctor didn’t just give you a rescue inhaler, it’s because rescue inhalers don’t stop the slow buildup of tightness—they just try to undo it after it’s already happened.
Below, you’ll find real comparisons of these drugs, what they cost, how they stack up against each other, and what people actually experience when they use them. No fluff. No marketing. Just what works, what doesn’t, and what you need to know to talk to your doctor with confidence.
How Bronchodilators Transform COPD Treatment: Benefits, Types, and Best Practices
Explore how bronchodilators work, their different classes, and step‑by‑step guidance for using them in COPD treatment, plus safety tips and future tech.
read more




