Pancreatic duct blockage: what it is and why it matters
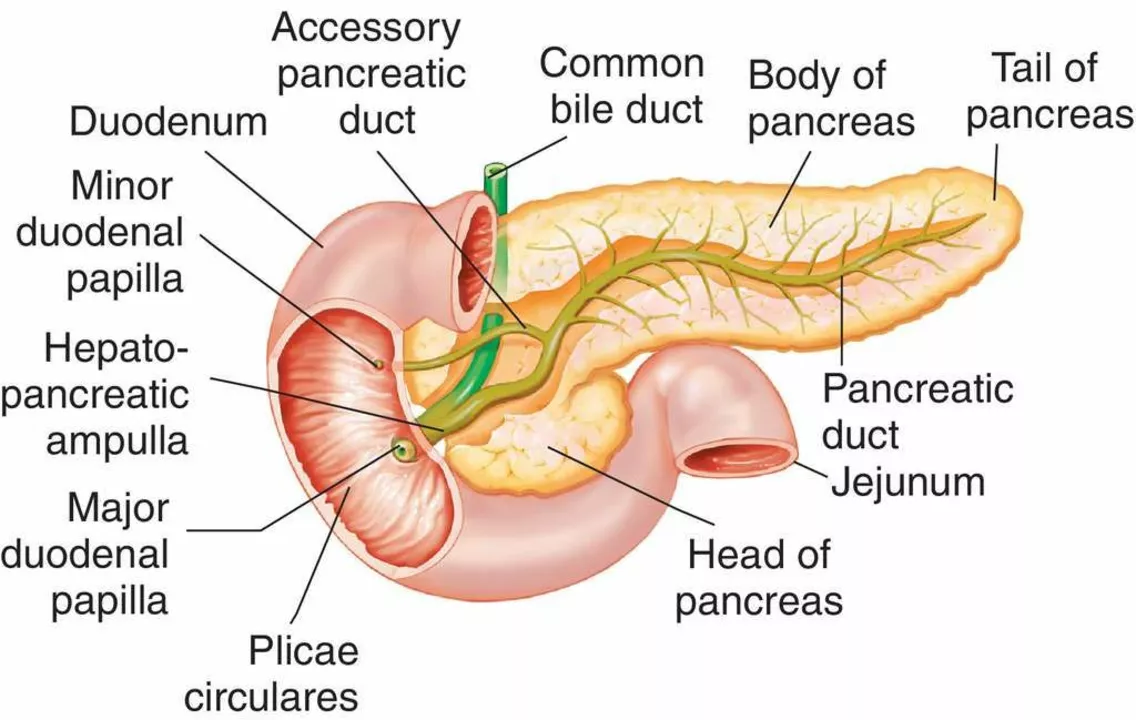
A blocked pancreatic duct can feel like bad indigestion at first, but it can quickly become serious. The duct carries digestive juices from the pancreas to the small intestine. When it’s blocked, those enzymes back up, irritate the pancreas, and can cause sudden pain, inflammation, and even infection.
Common causes and who gets it
Blockage happens for a few clear reasons: gallstones that travel into the duct, chronic pancreatitis with scar tissue and strictures, pancreatic tumors that press on the duct, trauma, or congenital issues like pancreas divisum. People who drink heavily over time, have recurrent gallstones, or have certain genetic conditions face higher risk.
Think you’re immune just because you feel fine now? Not always. Some blockages are partial and cause dull, recurring symptoms before a severe flare-up.
Signs to take seriously
The most common symptom is sudden, severe pain in the upper belly that often radiates to the back. Other signs: nausea, vomiting, fever (if infected), jaundice (yellow skin or eyes) when a bile duct is involved, oily stools, and unexplained weight loss. If pain comes in waves or gets steadily worse, don’t wait.
Blood tests often show high pancreatic enzymes (amylase and lipase) during inflammation. But imaging is key to spotting the exact problem.
Doctors use abdominal ultrasound and CT scans first because they’re fast and widely available. MRCP (MRI of the bile and pancreatic ducts) gives a noninvasive look at obstructions. Endoscopic ultrasound is useful for small stones or tumors. ERCP is special: it both shows the blockage and lets doctors treat it during the same procedure.
Treatment depends on the cause. If gallstones are to blame, ERCP can remove stones and place a temporary stent to keep the duct open. For strictures, balloons and stents can widen the duct. Tumors may need surgery (or oncology care) and chronic pancreatitis is managed with lifestyle changes, pain control, and sometimes surgery to drain or bypass the blocked segment.
In emergency cases with severe pancreatitis, hospitals give IV fluids, pain meds, and monitor for infection or organ problems. If the duct is infected, antibiotics and urgent drainage are needed.
Want to lower the odds of a repeat blockage? Treat gallstones proactively, cut back on alcohol, quit smoking, and follow up with your specialist. If the pancreas stops making digestive enzymes, your doctor may prescribe enzyme replacements and check blood sugar, since diabetes can follow chronic damage.
If you have sudden severe belly pain, fever, persistent vomiting, or yellowing of the skin, seek emergency care. These signs can mean a serious blockage or infected pancreas that needs quick treatment.
Questions about tests, ERCP, or living with pancreatic disease? Talk to your gastroenterologist — a short visit can clear up options and next steps.
The Role of Stress in the Development of Pancreatic Duct Blockage
In recent studies, I've discovered that stress plays a significant role in the development of pancreatic duct blockage. When we experience stress, our body's inflammatory response can cause inflammation in the pancreas, leading to blockage in the ducts. This blockage can result in painful and potentially life-threatening conditions such as pancreatitis. It's essential for us to manage our stress levels to maintain a healthy pancreas and overall well-being. By practicing relaxation techniques and stress reduction strategies, we can potentially reduce the risk of developing pancreatic duct blockage.
read more