Pharmacogenetic Testing: How Your Genes Affect Medication Response
When you take a pill, your body doesn’t just react the same way everyone else’s does. Your genes play a big role in how fast you break down drugs, whether they’ll work at all, or if you’re at risk for dangerous side effects. This is where pharmacogenetic testing, a medical test that looks at how your genes affect your response to medications. Also known as genetic drug testing, it helps doctors pick the right drug and dose for you—before you even take it. It’s not science fiction. It’s happening in clinics right now, especially for drugs like antidepressants, blood thinners, and pain meds.
Take Citalopram, an antidepressant that can cause dangerous heart rhythm changes if the dose is too high in certain people. Some folks have a gene variant that slows how their liver processes it. Give them the standard dose, and they’re at risk for QT prolongation—a heart issue that can be deadly. Pharmacogenetic testing catches this before it happens. Same with Metformin, a common diabetes drug that can cause lactic acidosis if kidney function is low and the patient has certain genetic markers. Or Carbamazepine, a seizure and nerve pain drug that can trigger a life-threatening skin reaction in people with a specific HLA gene variant. These aren’t rare cases. They’re predictable—and preventable—with the right genetic info.
Pharmacogenetic testing doesn’t just stop bad reactions. It helps you avoid the trial-and-error mess of trying three different antidepressants before one sticks. It cuts down on hospital visits from drug side effects. It saves money by stopping prescriptions that won’t work for you. And it’s not just for chronic conditions. Even antibiotics like Minocycline, used for acne and infections, can have unpredictable side effects based on your genes. The more we learn, the clearer it becomes: one-size-fits-all medicine is outdated.
You’ll find posts here that connect the dots between your genes and the drugs you take. From how pharmacogenetic testing explains why some people get swelling from meds while others don’t, to why certain heart drugs need dose limits based on DNA, to how genetic risks show up in fertility meds and mental health treatments. This isn’t theory. These are real stories from real patients, backed by clinical data. What you’re about to read will help you ask the right questions—and understand why your doctor might be thinking about your genes before writing your next prescription.
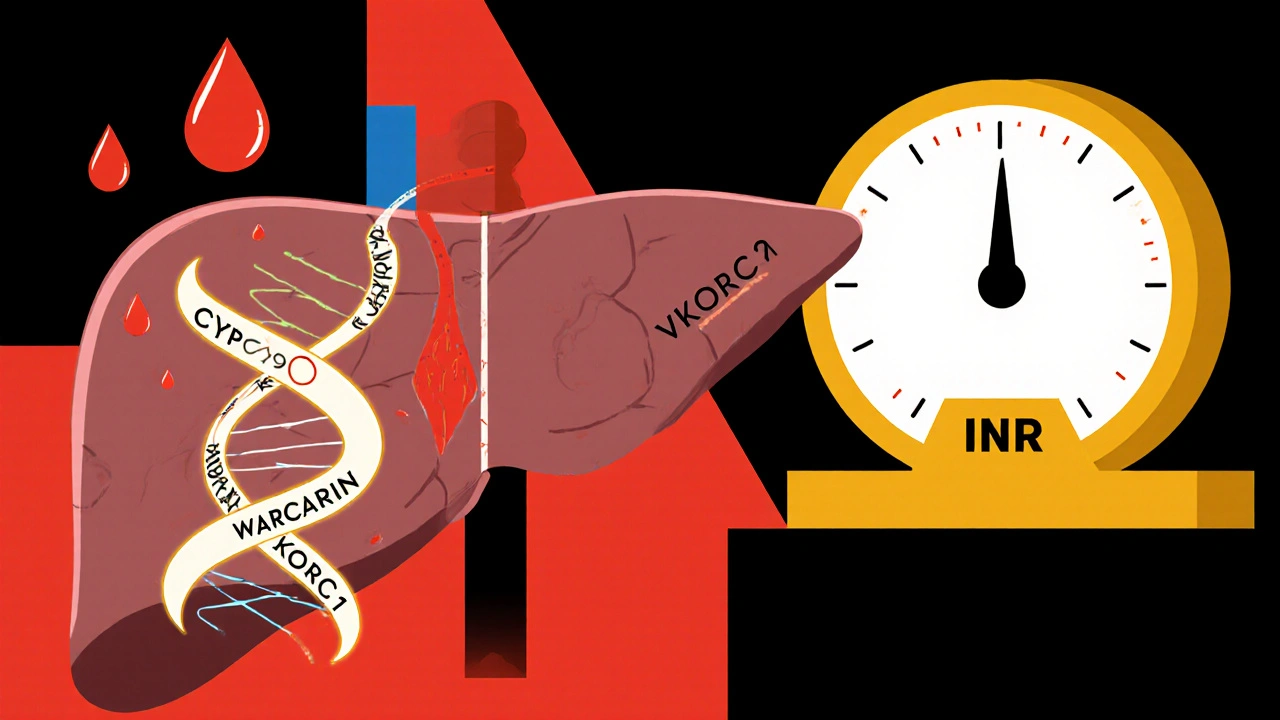
Warfarin Genetics: How CYP2C9 and VKORC1 Variants Affect Bleeding Risk and Dosing
Warfarin dosing varies wildly based on genetics. CYP2C9 and VKORC1 variants can make you dangerously sensitive to the drug. Testing before starting can cut bleeding risk by 32% and save lives.
read more