Warfarin Side Effects: What You Need to Know Before It’s Too Late
When you’re on warfarin, a blood thinner used to prevent dangerous clots in people with atrial fibrillation, artificial heart valves, or a history of deep vein thrombosis. Also known as coumadin, it’s one of the most prescribed anticoagulants in the world—but it’s not harmless. Many people think because it’s been around for decades, it’s safe to take without thinking. That’s where things go wrong.
Warfarin works by slowing down your blood’s ability to clot. That’s good if you’re at risk of a stroke or pulmonary embolism. But if your dose is even slightly off, or if you eat too many leafy greens, take an antibiotic, or skip a dose, your blood can either clot when it shouldn’t—or bleed when it shouldn’t. The biggest red flag? warfarin side effects like unusual bruising, nosebleeds that won’t stop, or blood in your urine or stool. These aren’t normal. They’re warnings. And they’re not rare. Studies show nearly 1 in 5 people on long-term warfarin will have a major bleeding event at some point. That’s why regular INR levels, a blood test that measures how long it takes your blood to clot are non-negotiable. If your INR is too low, you’re at risk for clots. Too high, and you’re one fall away from a dangerous bleed.
Warfarin doesn’t work in a vacuum. It’s affected by diet, especially foods high in vitamin K like kale, spinach, and broccoli. One week you eat a salad every day, the next you skip it—your INR swings. Same thing with alcohol, which can make warfarin stronger and increase bleeding risk. Even over-the-counter painkillers like ibuprofen or aspirin can turn a minor cut into a serious problem. And don’t forget about antibiotics, many of which interact with warfarin and can spike your INR overnight. That’s why every new medication—even a cold pill—needs to be checked with your doctor before you take it.
Some side effects are subtle. Fatigue, dizziness, or swelling in your legs might seem like aging or stress. But with warfarin, they could signal internal bleeding or a clot forming. And while most people focus on bleeding, warfarin can also cause skin necrosis—rare, but terrifying. It starts as red, painful patches that turn dark, usually in the first few days of treatment. If you see this, stop the drug and get to a hospital. It’s not something to wait on.
You’re not alone in this. Thousands of people manage warfarin safely every day. But it takes attention. Not just to the pill, but to your body, your food, your other meds, and your test results. The posts below dig into real cases: how hand swelling can be linked to blood thinners, what happens when warfarin mixes with other heart drugs, how to spot early signs of trouble before it becomes an emergency, and what to do when your INR won’t stay in range. These aren’t theory pieces. They’re from people who’ve been there—and lived to tell the story. Read them. Know your risks. Ask the right questions. Your life might depend on it.
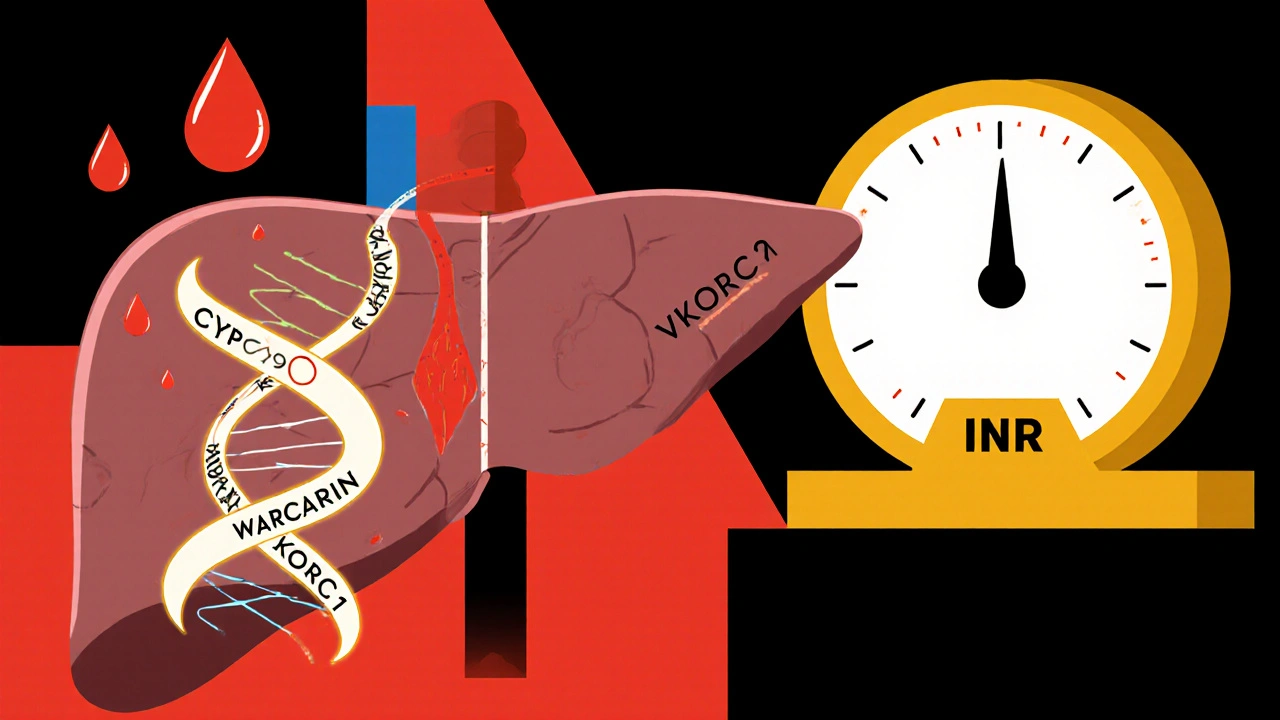
Warfarin Genetics: How CYP2C9 and VKORC1 Variants Affect Bleeding Risk and Dosing
Warfarin dosing varies wildly based on genetics. CYP2C9 and VKORC1 variants can make you dangerously sensitive to the drug. Testing before starting can cut bleeding risk by 32% and save lives.
read more