What Are TNF Inhibitors?
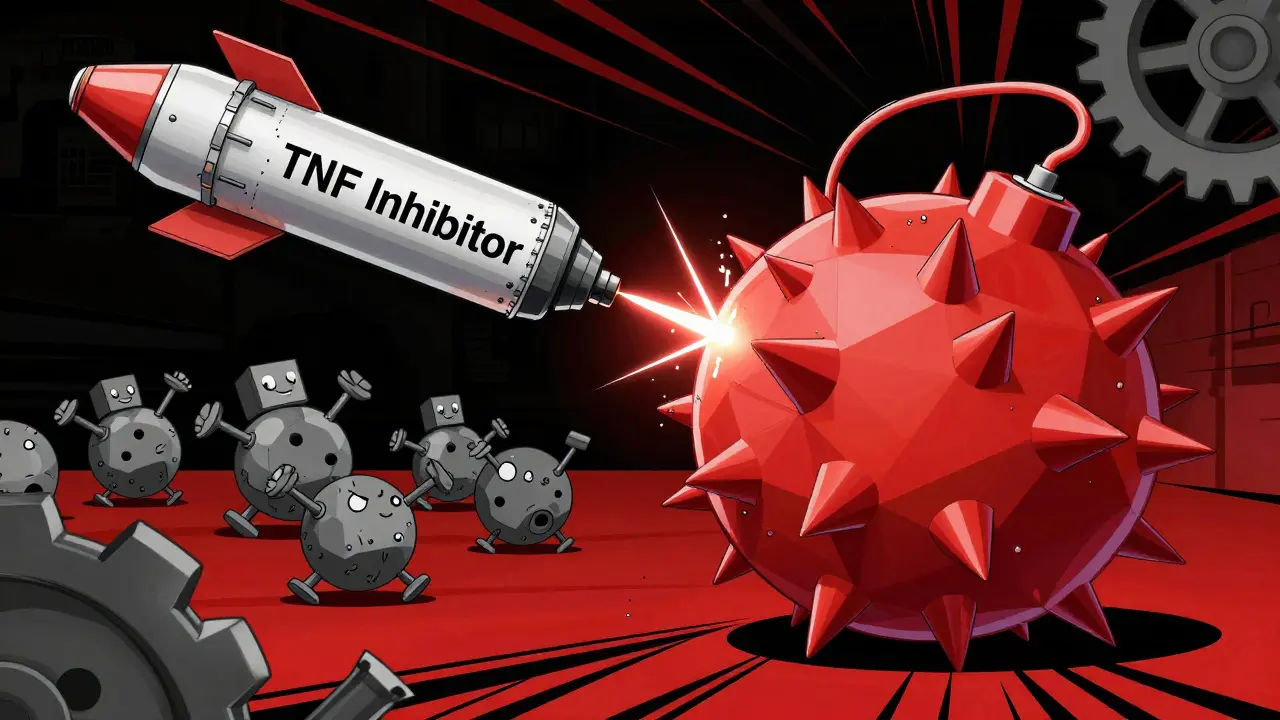
TNF inhibitors are a type of biologic drug designed to block tumor necrosis factor-alpha (TNFα), a protein that drives inflammation in autoimmune diseases. Unlike traditional pills that work broadly across the body, TNF inhibitors are made from living cells and act like precision missiles. They target only TNFα - a key signal that tells the immune system to attack healthy tissues. This makes them powerful tools for conditions like rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, and plaque psoriasis.
Before TNF inhibitors came along, doctors relied on drugs like methotrexate or sulfasalazine, known as DMARDs. These helped ease symptoms but didn’t stop joint damage in many patients. TNF inhibitors changed that. Studies show 50-60% of people with rheumatoid arthritis see major improvement on TNF blockers, compared to just 20-30% on older drugs. For some, it means going from using a cane to walking without pain.
How TNF Inhibitors Actually Work
TNFα is made mostly by immune cells called macrophages. When things go wrong in autoimmune diseases, these cells pump out too much TNFα. That signal tells other cells to swell, attack, and destroy tissue - especially in joints, skin, and the gut.
TNF inhibitors stop this by grabbing onto TNFα before it can bind to its receptors, TNFR1 and TNFR2. Think of it like cutting the wires between a bomb and its trigger. Without TNFα signaling, the body doesn’t send out the inflammatory command. That means less swelling, less pain, and slower damage to organs.
But not all TNF inhibitors work the same way. There are two main types:
- Fusion proteins - like etanercept - act as decoys. They look like part of the TNF receptor, so TNFα latches onto them instead of your real receptors.
- Monoclonal antibodies - like adalimumab, infliximab, golimumab, and certolizumab pegol - are lab-made antibodies that bind directly to TNFα and mark it for destruction.
Certolizumab is unique because it’s a fragment of an antibody, not a full one. It doesn’t trigger immune cells to attack, which may explain why it’s sometimes used in pregnancy. Etanercept, on the other hand, can’t bind to membrane-bound TNF as well, so it works mostly on the floating kind.
The Five FDA-Approved TNF Inhibitors
Five TNF inhibitors are approved in the U.S. for autoimmune conditions. Each has different ways of being given, how often you need them, and how they interact with your immune system.
| Drug Name | Brand Name | Type | How It’s Given | Frequency | Key Feature |
|---|---|---|---|---|---|
| Etanercept | Enbrel | Fusion protein | Subcutaneous injection | Once or twice a week | Decoy receptor; doesn’t trigger immune cell killing |
| Infliximab | Remicade | Monoclonal antibody | IV infusion | Every 4-8 weeks | Strongly binds both forms of TNF; can cause infusion reactions |
| Adalimumab | Humira | Monoclonal antibody | Subcutaneous injection | Every other week | Most prescribed; high rates of antibody development |
| Golimumab | Simponi | Monoclonal antibody | Subcutaneous injection | Once a month | Long-acting; good for spine inflammation |
| Certolizumab pegol | Cimzia | PEGylated Fab’ fragment | Subcutaneous injection | Every 2-4 weeks | Doesn’t cross placenta; often used in pregnancy |
Some, like infliximab, require visits to a clinic for IV infusions. Others, like Humira or Enbrel, can be self-injected at home after a short training session. Most patients learn to give themselves shots in 1-2 weeks. Manufacturers like AbbVie and Janssen offer support programs with nurses, injection training, and help with insurance costs.
Why They Don’t Work for Everyone
Even though TNF inhibitors are life-changing for many, they don’t help everyone. About 30-40% of patients experience what’s called “secondary failure.” That means the drug works at first - maybe even brilliantly - but after months or years, it stops working.
The main reason? The body starts making anti-drug antibodies. Your immune system sees the biologic as a foreign invader and attacks it. These antibodies bind to the drug and clear it from your bloodstream before it can do its job. This is more common with infliximab and adalimumab than with etanercept.
Some people never respond at all - this is called “primary non-response.” Doctors don’t always know why. Genetics, the type of disease, or how advanced it is might play a role. If a TNF inhibitor doesn’t work after 3-6 months, switching to a different biologic - like one that blocks IL-17 or IL-23 - is often the next step.
The Hidden Risks: Infections and Paradoxical Reactions
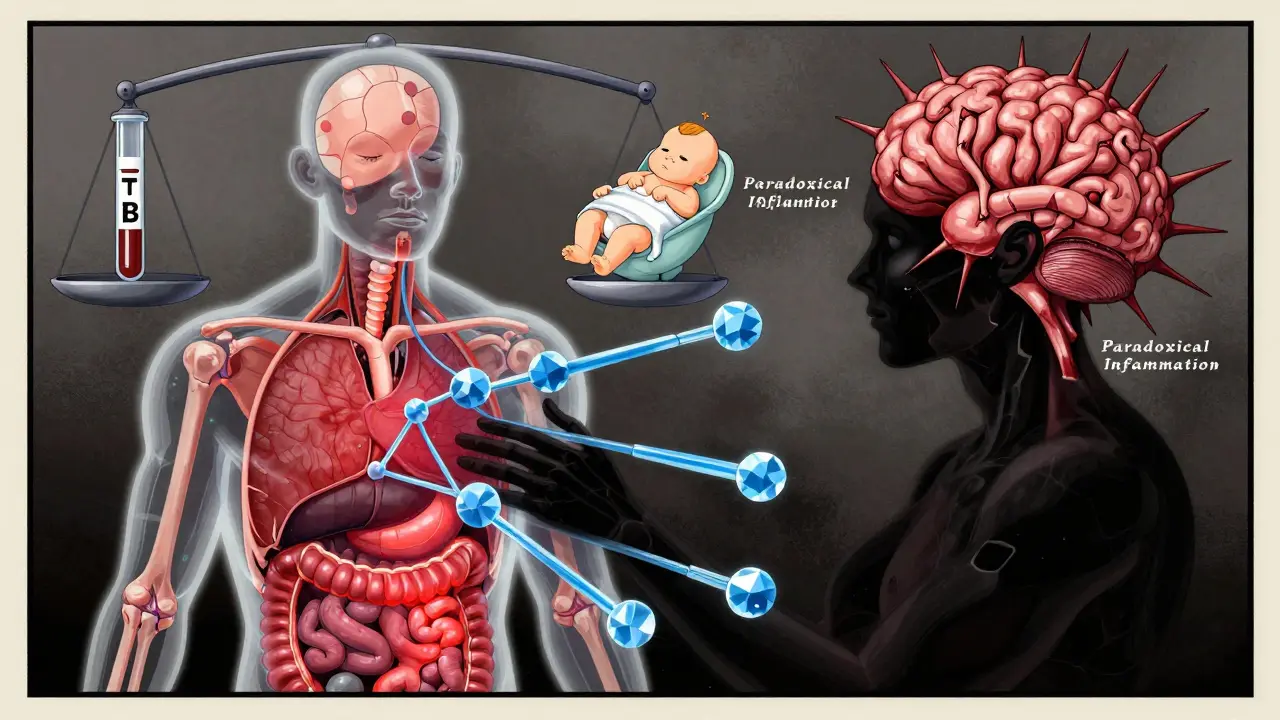
Blocking TNFα weakens your immune system’s ability to fight off certain infections. People on these drugs have a 2-5 times higher risk of serious infections like tuberculosis, pneumonia, and fungal infections.
That’s why everyone gets tested for latent TB before starting treatment. If you’ve had TB before, even if it was years ago, the drug can wake it up. Screening usually involves a skin test or blood test, and sometimes a chest X-ray.
There’s also something strange called “paradoxical inflammation.” Even though TNF inhibitors reduce inflammation in joints or guts, they can sometimes cause new inflammation elsewhere - like in the skin (new psoriasis), nerves (demyelination), or even the brain. Studies show patients on TNF blockers have a 2.3 times higher risk of developing inflammatory conditions in the central nervous system.
Why? Because TNFα isn’t just a bad guy. It helps control infections, regulates immune cell death, and even protects nerves. When you block it everywhere, you might accidentally shut down helpful signals. TNF inhibitors can’t cross the blood-brain barrier, so while they calm inflammation in the body, they might leave the brain in a confused state - leading to unwanted immune reactions.
Real-Life Impact: What Patients Say
On forums like Reddit and HealthUnlocked, patients share raw stories. One person wrote: “After six months on adalimumab, I went from barely walking to hiking five miles a week.” Another said: “The injections hurt, and I hated the thought of carrying needles everywhere - but I’d do it again in a heartbeat.”
But there are also tough experiences. Injection site reactions - redness, itching, swelling - happen in 20-30% of users. Some people feel anxious about giving themselves shots. Others worry about long-term risks. One patient on r/RA shared: “I’ve been on Humira for 8 years. It saved my life, but I’m terrified of getting sick.”
For many, the trade-off is worth it. Before biologics, life with severe rheumatoid arthritis meant constant pain, joint deformities, and early retirement. Now, many people work, travel, and raise families without being held back by their disease.
What Comes Next?
TNF inhibitors dominated the biologics market for over 20 years. In 2022, the global market was worth $35 billion, with Humira alone bringing in $21.2 billion. But things are changing. Biosimilars - cheaper versions of the original drugs - are now widely available. Amjevita, a biosimilar to Humira, captured 25% of the U.S. market by 2022.
Newer drugs that block IL-17 or IL-23 are showing better results for psoriasis and psoriatic arthritis. Some doctors now use those first for skin-focused disease. But for rheumatoid arthritis and Crohn’s disease, TNF inhibitors are still the most proven option.
Research is now focused on smarter drugs - ones that block only TNFR1 (the bad actor) and leave TNFR2 (the protector) alone. Early animal studies show this could reduce side effects while keeping the benefits. It’s not here yet, but it’s coming.
For now, TNF inhibitors remain a cornerstone of autoimmune care. They’re not perfect, but for millions, they’re the difference between living with disease and living well.
How long does it take for TNF inhibitors to start working?
Most people notice some improvement in pain and swelling within 2-6 weeks. Full benefits usually take 3-6 months. Some patients feel better sooner, especially with infliximab infusions, while others need more time. If there’s no change after 12 weeks, your doctor may consider switching treatments.
Can I stop taking TNF inhibitors if I feel better?
Usually not. Stopping the drug often leads to a flare-up of symptoms within weeks. Even if you’re in remission, continuing treatment helps keep the disease under control. Some patients under strict medical supervision may try tapering, but this is rare and risky. Never stop without talking to your rheumatologist or gastroenterologist.
Are TNF inhibitors safe during pregnancy?
Certolizumab pegol is the only TNF inhibitor proven to cross the placenta very little, making it the preferred choice during pregnancy. Adalimumab and infliximab can cross in the third trimester, so doctors often stop them after 20 weeks. Etanercept is considered low-risk but still monitored. Always plan ahead with your doctor if you’re thinking about pregnancy.
Do TNF inhibitors cause cancer?
There’s a small increased risk of certain skin cancers and lymphoma, but the overall risk remains low. The underlying autoimmune disease itself carries cancer risks too. Regular skin checks and avoiding excessive sun exposure are recommended. Most studies show the benefits outweigh the risks for most patients.
What’s the difference between a biologic and a biosimilar?
A biologic is the original drug made from living cells - like Humira or Enbrel. A biosimilar is a highly similar version made after the original patent expires. Biosimilars aren’t generics; they’re complex copies that match the original in safety, purity, and potency. They’re cheaper and work the same way. Amjevita is a biosimilar to Humira and is approved for all the same conditions.
Next Steps if You’re Considering TNF Inhibitors
If your doctor suggests a TNF inhibitor, ask these questions:
- Have I tried and failed at least two conventional DMARDs?
- Do I have any active infections or a history of TB?
- What are the risks of infection or paradoxical reactions for my specific condition?
- Can I manage the injection schedule, or should I consider an IV option?
- Is there a biosimilar available that’s covered by my insurance?
Most insurance plans require prior authorization. Your doctor’s office will handle this, but you’ll need to provide records showing you’ve tried other treatments first. Support programs from drugmakers can cut your out-of-pocket cost by 70-90% if you qualify.
TNF inhibitors aren’t magic. They come with risks, costs, and daily management. But for the millions who’ve regained their mobility, their jobs, and their lives - they’re one of the most important medical advances of the last 30 years.







14 Comments