
When an alert flashes on your screen - a drug interaction warning, a lab result flagged as critical, a system outage notice - your body doesn’t wait for you to think. Your heart jumps. Your breath tightens. Your mind goes blank. This isn’t weakness. It’s biology. And it’s happening more often than you realize. In 2026, the average person receives 67 alerts per week across work, health apps, and personal devices. Most of these are noise. But when one turns real - a medication recall, a patient’s abnormal vitals, a security breach - panic can turn a simple response into a costly mistake.
Why Alerts Trigger Panic
Your brain treats sudden alerts like a lion appearing on the savanna. Even if it’s just a false alarm, your amygdala - the part of your brain that handles fear - takes over. It shuts down your prefrontal cortex, the area responsible for logic, planning, and weighing options. This isn’t a flaw. It’s a survival mechanism. But in modern life, where alerts are constant and rarely life-threatening, this reaction becomes a liability. Studies show that during panic, decision-making ability drops by up to 67%. People make rushed choices, ignore key details, or freeze entirely. In healthcare, this can mean giving the wrong dose. In cybersecurity, it can mean shutting down a system that doesn’t need it. In finance, it can mean selling stocks at a loss. The problem isn’t the alert. It’s how you react to it.Step 1: Pause Before You Act
The first rule after any alert? Don’t move for five seconds. That’s it. Just stop. Breathe. Wait. This tiny pause breaks the automatic panic loop. Your body needs time to shift from fight-or-flight to calm-and-assess. You don’t need to solve the problem yet. You just need to stop reacting. Here’s how to do it: Place one hand on your chest, the other on your belly. Breathe in slowly through your nose for four counts. Hold for seven. Exhale through your mouth for eight. Repeat three times. This 4-7-8 breathing technique lowers your heart rate from 110+ beats per minute to 70-85 in under 90 seconds. That’s the difference between panic and control.Step 2: Ground Yourself in the Present
When your mind is racing, it’s stuck in the future - imagining worst-case scenarios. To pull yourself back, use the 5-4-3-2-1 method. It’s simple, fast, and proven.- Look around and name 5 things you can see - the monitor, the coffee cup, the clock, the plant, the door.
- Touch 4 things - your chair, your pen, your phone, your sleeve.
- Listen for 3 sounds - the hum of the computer, distant traffic, your own breath.
- Notice 2 smells - mint gum, coffee, soap, paper.
- Identify 1 thing you can taste - water, toothpaste, the last bite of lunch.

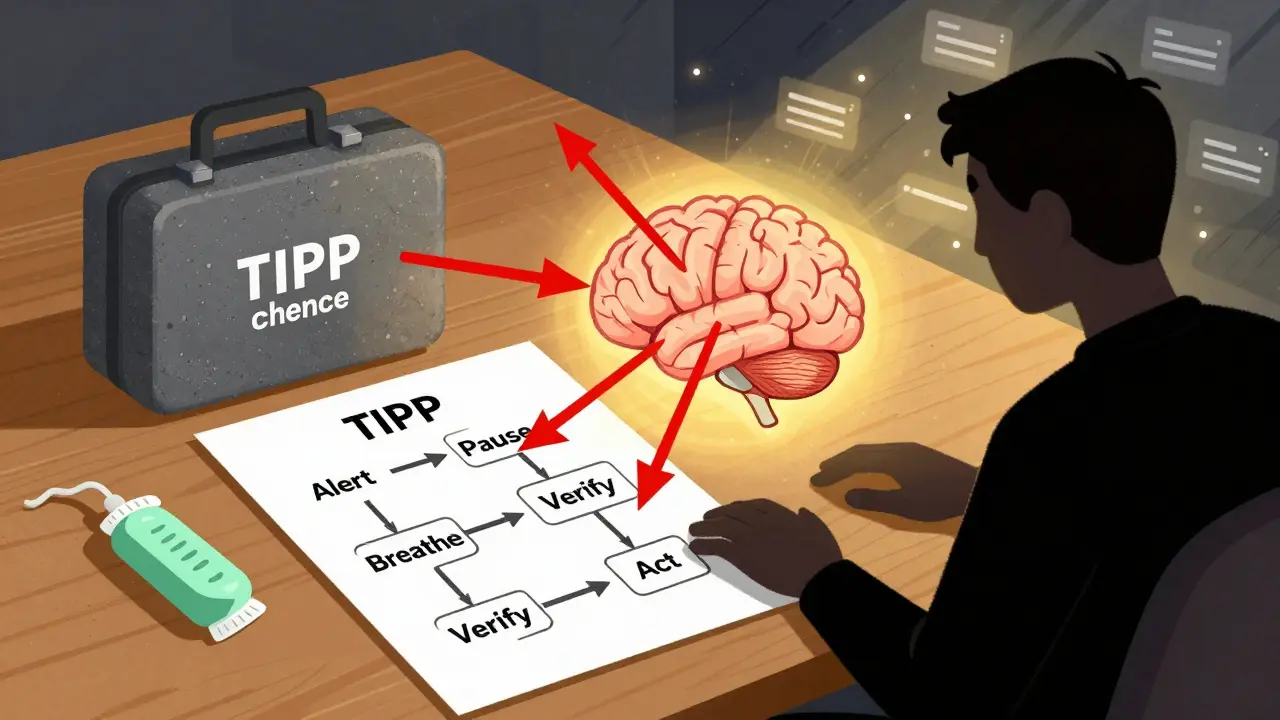
Step 3: Use the TIPP Technique for Immediate Calm
If you’re still feeling overwhelmed, try TIPP - a set of four quick physical actions designed to reset your nervous system. These are used by first responders and ER staff worldwide.- Temperature: Splash cold water on your face, or hold an ice pack against your wrists for 15 seconds. Cold triggers the mammalian dive reflex - it slows your heart rate instantly.
- Intense Exercise: Do 30 seconds of jumping jacks, run in place, or push hard against a wall. This burns off adrenaline.
- Paced Breathing: Go back to 4-7-8 breathing. Do it again. This time, focus on making the exhale longer than the inhale.
- Paired Muscle Relaxation: Tense your fists for five seconds. Then release. Do the same with your shoulders, your jaw, your feet. Tension and release tells your brain: “You’re safe.”
Step 4: Ask the Right Questions
Once you’re calm, don’t jump to action. Ask yourself these three questions:- What’s the actual risk? Is this alert life-threatening? Or is it a false positive? Check the source. Look at the details. Don’t assume.
- What’s the worst that could happen if I wait 10 minutes? Most alerts aren’t time-critical. Waiting gives you space to verify, consult, or get help.
- What’s my core value here? Are you acting to protect safety? To avoid blame? To look competent? If your motive is fear, pause again. If it’s care, keep going.
Step 5: Build a Personal Alert Response Kit
You wouldn’t walk into a hospital without a stethoscope. Don’t walk into an alert without a plan. Create a small physical or digital kit to keep near your workspace.- A textured stone or stress ball (for touch grounding)
- Mint gum or a scented lotion (for smell and taste)
- A printed one-page cheat sheet with the 5-4-3-2-1 method and TIPP steps
- A simple decision flowchart: “Alert → Pause → Breathe → Verify → Act”
Long-Term: Train Your Brain Before the Alert
The biggest mistake? Waiting until you’re in crisis to learn how to calm down. Panic doesn’t care if you’ve never practiced. The solution? Daily mindfulness. Just 10 minutes a day. Sit quietly. Focus on your breath. When your mind wanders (it will), gently bring it back. No judgment. Just return. Research from Mindful.org shows that after eight weeks of this practice, gray matter in your prefrontal cortex increases by 4.3%. That’s not just feel-good stuff. It means your brain becomes better at staying calm under pressure. Your decisions get sharper. Your reactions get slower - in the best way. Also, sleep. Caffeine. Movement. These aren’t optional. People who get 7-9 hours of sleep, limit caffeine to under 200mg a day, and move for 150 minutes weekly reduce baseline anxiety by 41%, according to BHB Hospital’s 2022 trial. Lower baseline anxiety = less panic when alerts hit.What’s Changing Now
The world is catching up. Starting in January 2025, the European Union’s Digital Operational Resilience Act (DORA) requires companies to include human psychological responses in their alert and incident plans. That means training, not just tech. New tools are emerging too. Wearables now detect when your heart rate spikes during an alert and automatically trigger calming audio or breathing prompts. AI systems are being trained to guide users through questions during alerts - not just list warnings, but walk you through what to do next. By 2026, 65% of enterprise alert systems will have built-in panic management features. But until then, you have to be your own system.Final Thought: You’re Not Broken
If you’ve ever frozen during an alert, you’re not failing. You’re human. The system is just designed for machines, not people. The goal isn’t to never feel fear. It’s to not let fear make your decisions for you. Every time you pause, breathe, ground yourself, and ask the right questions - you’re not just avoiding panic. You’re reclaiming your power. You don’t need to be perfect. You just need to be prepared. And you’re already on the way.Why do I panic when I get an alert, even if it’s not serious?
Your brain is wired to treat sudden alerts like threats - even if they’re not. This is called the fight-or-flight response. It’s controlled by the amygdala, an ancient part of your brain that prioritizes survival over logic. In modern life, where alerts are constant, this system often overreacts. It’s not you being weak. It’s your biology misfiring. The good news? You can train it to respond better.
How long does it take to see results from panic management techniques?
You can feel calmer within minutes using techniques like breathing or grounding. But real, lasting change takes practice. Most people notice a significant drop in panic intensity after 30 days of daily 10-minute mindfulness sessions. After 8 weeks, brain scans show actual physical changes - more gray matter in areas responsible for calm thinking. Consistency matters more than intensity.
Can I use these techniques if I’m not in healthcare?
Absolutely. These methods work for anyone facing high-pressure alerts - whether you’re a trader reacting to market swings, an IT worker responding to a security breach, a parent getting a school emergency notice, or someone getting a health app warning. Panic doesn’t care about your job title. These tools are universal.
What if I forget the steps during a real alert?
That’s normal - 68% of people report this. The fix? Practice before it happens. Keep a printed reminder near your workstation. Set a daily phone alarm that says “Pause. Breathe. Ground.” Use the 5-4-3-2-1 method - it’s the easiest to remember because it uses your senses. If you can see, touch, hear, smell, or taste something, you’re already grounding yourself. Start there.
Are there apps or tools that help with alert-related panic?
Yes. Some apps now integrate with wearable devices to detect elevated heart rate and trigger breathing exercises automatically. Others offer guided 60-second grounding sessions. Look for tools that use evidence-based methods like TIPP, 4-7-8 breathing, or mindfulness. Avoid apps that just count breaths without context. The best ones combine tech with clear, simple instructions you can follow even when stressed.







8 Comments
Okay but can we just take a second to appreciate how this article didn’t just throw tech advice at us like a generic checklist? I’ve been using the 5-4-3-2-1 method since last month and holy crap-it actually works. I’m a nurse and I used to freeze every time a monitor went off. Now? I touch my stethoscope, smell the hand sanitizer, hear the AC, see the chart, taste my gum-and suddenly I’m not a panic mess. I even printed the cheat sheet and taped it to my badge holder. My coworkers think I’m weird, but they’re asking me how I stay so calm now. You’re not broken. You’re just surrounded by machines that forgot we’re human.
I love this. I’m a sysadmin in London and our alert system used to give me anxiety attacks. Now I keep a stress ball and a peppermint oil roll-on on my desk. The cold splash trick? Game changer. I did it during a false ransomware alert last week-my whole team was screaming, I just walked to the bathroom, splashed water, and started checking logs. No one else could even type. I didn’t fix the problem faster, but I stopped the panic from spreading. Small things matter.
LMAO. All this breathing and grounding nonsense? Just turn off the damn alerts. If your system is pinging you 67 times a week, it’s broken, not you. I’ve worked in IT for 15 years. The real solution? Reduce noise. Automate the crap out of everything. If it’s not critical, it shouldn’t ping. If it’s critical, it should auto-resolve or escalate to a human who’s actually trained. Stop making people meditate to survive their jobs. Fix the system. That’s it.
Shawn’s got a point, but he’s missing the bigger picture. You can’t just turn off alerts in healthcare or finance-some of them save lives. What this article gives you isn’t a bandaid, it’s a toolkit. I’m a pharmacist and I’ve seen people give wrong meds because they panicked at a drug interaction alert. The 4-7-8 breathing? I teach it to new hires. It takes 90 seconds. It’s not about avoiding alerts. It’s about not becoming the alert’s victim. And yeah, we need better systems too-but until we get them, this stuff works.
The cited studies lack methodological rigor. The Abundance Therapy Center is not a peer-reviewed institution. The 67 alerts/week statistic appears to be extrapolated from non-representative consumer data. The TIPP technique, while derived from DBT, was not validated in alert-response contexts. The claim about gray matter increase is misleading-it conflates correlation with causation. This article reads like a marketing piece disguised as neuroscience.
Wow. Sarah’s comment is like someone reading a self-help book and then writing a 10-page critique of the font size. Meanwhile, I’m over here in the ER, watching a nurse use the 5-4-3-2-1 method after a code blue alert-and she didn’t miss a beat. The science? Maybe imperfect. But the result? People are surviving. You can’t quantify courage with a p-value. Sometimes the best tool isn’t the most rigorously studied one-it’s the one that gets you to breathe when your heart’s about to explode.
Bro, I’m from India and I work in fintech. We get alerts like crazy-fraud flags, system crashes, API timeouts. I used to lose sleep. Then I started doing the 4-7-8 breathing before my morning coffee. Now I do it before every alert. It’s not magic, but it’s like hitting pause on my panic button. I even made a little sticky note with ‘BREATHE → CHECK → ACT’ and stuck it on my monitor. My team started copying it. We’re not just better at our jobs-we’re nicer to each other. This isn’t just about alerts. It’s about being human in a world that wants you to be a robot. 🙏
While the heuristic frameworks presented are empirically supported in clinical anxiety contexts, their transferability to high-stakes operational environments remains under-documented. The 5-4-3-2-1 protocol, while effective for acute panic episodes, introduces latency in time-critical decision chains. For instance, in a cardiac ICU, a 90-second pause may exceed the acceptable response window for a critical arrhythmia alert. The TIPP technique’s physiological grounding mechanisms are valid, yet their efficacy is contingent upon environmental affordances (e.g., access to cold water, space for exercise). A more robust solution would integrate these behavioral protocols into automated alert escalation workflows, embedding decision-support prompts directly into EHR and SIEM interfaces. Until then, individual coping mechanisms remain necessary, albeit insufficient, compensatory strategies.