
After giving birth, pain is normal. Whether you had a vaginal delivery or a C-section, your body has been through a major event. But if you’re breastfeeding, choosing the right pain medication isn’t as simple as grabbing what’s in your medicine cabinet. You want relief-fast-but you also need to know what’s safe for your baby. The good news? Most common pain relievers are perfectly safe. The bad news? Some medications you might assume are fine can be dangerous.
Start with the safest options: acetaminophen and ibuprofen
The first line of defense for postpartum pain should be acetaminophen and ibuprofen. These are the only two pain relievers consistently rated as safe by the American College of Obstetricians and Gynecologists (ACOG), the Academy of Breastfeeding Medicine, and the InfantRisk Center. Both pass into breast milk in tiny amounts-less than 1% of your dose-and even less is absorbed by your baby’s body.
Acetaminophen reaches peak levels in breast milk about 1 to 2 hours after you take it. Ibuprofen peaks around the same time. Neither affects your milk supply. You can take them on schedule, even every 4 to 6 hours, without worrying about buildup in your baby. Many hospitals now give new moms a combination of both-acetaminophen every 6 hours and ibuprofen every 8 hours-to keep pain under control without opioids.
For C-section recovery, some hospitals use Toradol (ketorolac) IV for the first 24 hours instead of oral NSAIDs. It’s effective and safe for short-term use, even while breastfeeding. After that, switch to ibuprofen. The Michigan OPEN initiative recommends this approach because it reduces opioid use right after surgery.
Avoid codeine and tramadol at all costs
Don’t take codeine or tramadol if you’re breastfeeding. Period.
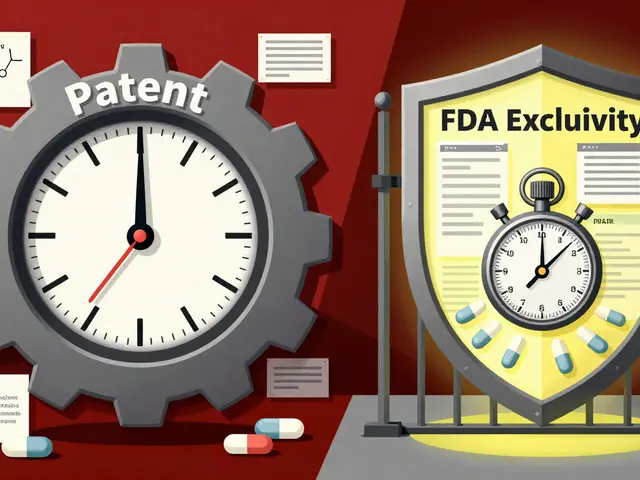
The FDA issued strong warnings in 2017 for codeine and 2018 for tramadol, saying breastfeeding is not recommended while using either drug. Why? Because some mothers are ultra-rapid metabolizers. That means their bodies turn these drugs into morphine or M1 (an active opioid metabolite) way faster than normal. About 1 in 100 Caucasian women-and even more in some other populations-are this type of metabolizer. And you won’t know unless you get tested.
That extra morphine ends up in your breast milk. In one documented case, a mother took a standard dose of codeine after a C-section. Her baby, just 12 days old, stopped breathing and died. Another infant became so sleepy he couldn’t latch. These aren’t rare flukes. The FDA reviewed over 60 cases of infant deaths linked to codeine in breastfeeding mothers.
Tramadol has the same problem. Its metabolite M1 can cause life-threatening breathing problems in babies-even when the mom takes the exact dose prescribed. In 2019, the FDA reported another case where a baby developed respiratory depression after the mother took tramadol for postpartum pain. The baby survived, but only because doctors caught it early.
Even a single accidental dose of codeine or tramadol should be treated as a red flag. Monitor your baby closely for 24 hours: Are they unusually sleepy? Are they having trouble latching? Are they breathing slowly or irregularly? If yes, call your pediatrician immediately.
If you need an opioid, choose morphine
Sometimes, ibuprofen and acetaminophen aren’t enough. After a major surgery or severe tearing, you might need something stronger. If that’s the case, morphine is the safest opioid option for breastfeeding mothers.
Why morphine? Because babies absorb almost nothing from it. Only about 0.5% to 1% of the morphine in your milk gets into your baby’s bloodstream. That’s because their immature guts can’t absorb it well. Other opioids like hydrocodone, oxycodone, and hydromorphone are okay in small, short-term doses-but they carry more risk.
Studies show oxycodone passes into milk at 0.1% to 0.5% of the maternal dose. That’s low, but still enough to make some babies sleepy or constipated. The InfantRisk Center rates morphine as the safest opioid because it’s predictable. Codeine? Unpredictable. Tramadol? Dangerous. Morphine? Reliable.
Doctors at Intermountain Health recommend taking opioids right after you breastfeed-not before. That way, your baby gets the lowest possible dose. The drug peaks in your blood and milk about 1 to 2 hours after you take it. Waiting 3 to 4 hours before the next feed gives your body time to clear most of it.
Never use opioids longer than 4 to 6 days. The goal is to get you through the worst of the pain, not to manage chronic discomfort. After that, go back to acetaminophen and ibuprofen.
Timing matters more than you think
It’s not just about which drug you take-it’s when you take it.
For acetaminophen and ibuprofen, timing doesn’t matter much. You can take them before or after feeding. But with opioids, timing is critical. Take the dose right after you nurse. Then wait at least 3 to 4 hours before the next feed. This lets your body process the drug before your baby gets more milk.
Also, don’t combine pain meds unless your doctor says so. Taking ibuprofen and acetaminophen together every 3 hours is fine-it’s actually recommended by some hospitals. But mixing opioids with NSAIDs or acetaminophen increases risk without adding much benefit.
And please, stop the “pump and dump” myth. That old advice-discarding milk for 24 hours after anesthesia or pain meds-is outdated. The Academy of Breastfeeding Medicine removed it from their guidelines in 2021. There’s no need to throw away your milk. You’re not poisoning your baby. You’re just giving them tiny, safe amounts of medicine.
Watch for signs your baby is affected
Even safe medications can cause issues in rare cases. Here’s what to look for:
- Excessive sleepiness-your baby is harder to wake for feeds
- Difficulty latching or sucking
- Slow or shallow breathing
- Constipation or less frequent poops
- Unusual fussiness or limpness
If you notice any of these, especially after starting a new pain med, contact your pediatrician. Don’t wait. Early signs of opioid overdose in babies are subtle. They might just seem “sleepier than usual.” But that’s enough to be dangerous.
For babies under 2 months old, extra caution is needed. Their livers and kidneys aren’t fully developed. They can’t clear drugs as quickly. That’s why doctors are extra careful with opioids in newborns.

What about naproxen or indomethacin?
Some moms hear that naproxen is an NSAID like ibuprofen and assume it’s safe. It’s not. Naproxen stays in your system longer. It can build up in breast milk over time. The Breastfeeding Network warns against using it in newborns or preemies because of reports of side effects like drowsiness and low blood pressure.
Indomethacin is even riskier. It’s sometimes used for premature babies to close a heart defect-but that’s under strict medical supervision. Don’t take it for postpartum pain unless your doctor specifically says so.
Stick to ibuprofen. It’s cleared quickly. It’s well-studied. It’s safe.
Future options: genetic testing
Right now, there’s no routine test to find out if you’re an ultra-rapid metabolizer. But researchers at Mayo Clinic published a study in 2023 showing that testing for the CYP2D6 gene could predict who’s at risk for dangerous reactions to codeine and tramadol. It’s not standard care yet-but it might be soon.
For now, the safest approach is simple: avoid codeine and tramadol entirely. Don’t wait for a test. Don’t gamble. If your doctor prescribes one of these, ask for an alternative. Say, “I’m breastfeeding. Is there a safer option?”
Bottom line: you can manage pain and breastfeed
Postpartum pain doesn’t mean you have to choose between comfort and your baby. You can have both. Use acetaminophen and ibuprofen as your first tools. If you need more, use morphine for a few days, timed right after feeds. Avoid codeine and tramadol like fire. Watch your baby closely. And remember-you’re not alone.
Many new moms feel guilty about needing pain meds. But pain that’s not controlled can make it harder to hold your baby, to rest, to bond. Managing pain properly helps you be the mom you want to be. Talk to your doctor. Ask questions. Advocate for yourself. Your health matters as much as your baby’s.






11 Comments
Just had my second baby and this post saved me from a nightmare. I was about to ask for tramadol after my C-section until I read this. Thank you for the clarity - no more guesswork.
Let’s be real - most OBs still push codeine like it’s candy. I had to fight my own doctor for 48 hours before they switched me to ibuprofen + acetaminophen. The hospital pharmacy had to send in a clinical pharmacist to explain the CYP2D6 risk. If you’re breastfeeding, always ask: ‘Is this FDA-approved for lactation?’ If they hesitate, walk out. Your baby’s life > hospital protocol.
Acetaminophen isn’t ‘safe’ - it’s just less obviously deadly. The liver toxicity data in neonates is buried in 2015 cohort studies you won’t find unless you dig through PubMed. And morphine? Sure, absorption is low - but what about cumulative dosing over multiple feeds? No one talks about the 3-day half-life in neonatal plasma. This post is dangerously oversimplified.
Look, I get the fear-mongering about codeine. But let’s not pretend every mom is a genetic lottery winner. I’m a 34-year-old South Asian woman, took codeine for 3 days postpartum, baby’s fine. My cousin in Bangladesh took it for weeks after her third delivery. No issues. The FDA warnings are based on a handful of Caucasian cases - this is bias dressed as science. Stop scaring people with outliers. We need pain relief, not panic.
Also, ‘pump and dump’ is still alive in 80% of lactation consultants’ offices. I had to pay $200 for a private IBCLC to tell me it’s nonsense. Why are we still teaching this?
For anyone reading this: if you’re in a country where ibuprofen is hard to get, paracetamol alone is still better than nothing. The key is dose frequency - don’t exceed 3000mg/day. And if you’re using opioids, keep a log of feeding times and baby’s behavior. I kept a notebook for 7 days after my surgery. It helped me spot the slight lethargy before it became a problem.
Also, naproxen isn’t banned - it’s just not ideal for newborns. If your baby is 6+ weeks and you’ve got chronic pelvic pain, short-term naproxen under supervision is sometimes acceptable. But don’t self-prescribe.
Oh wow. Another ‘breastfeeding gospel’ post. Let me guess - the author works for a pharmaceutical company that sells acetaminophen? Because this reads like a marketing brochure disguised as medical advice. Morphine is ‘safe’? Really? What about the 2021 study in JAMA Pediatrics showing altered neurodevelopmental markers in infants exposed to even low-dose opioids? You think ‘0.5% absorption’ means ‘no effect’? That’s like saying a drop of cyanide is fine because it’s diluted.
And why no mention of non-pharmacological options? Cold packs, TENS units, pelvic floor PT? No. Just ‘take pills and shut up.’ Classic medical paternalism wrapped in pink.
I’m a nurse and I’ve seen babies go into respiratory arrest from codeine. I’ve held mothers as they screamed because their 10-day-old stopped breathing. This isn’t hypothetical. This is real. If your doctor gives you codeine or tramadol, say ‘I’m breastfeeding - I need an alternative.’ If they roll their eyes, get a second opinion. You are not being dramatic. You are being a warrior.
You can heal and breastfeed. You don’t have to suffer. But you do have to be loud. Be the mom who asks the hard questions. Your baby is counting on you.
For those worried about opioids - I used morphine for 4 days after a severe perineal tear. Took it right after night feedings, waited 4 hours. Baby was alert, latched fine, pooped regularly. No sedation. The key is timing and duration. Don’t use it longer than needed. And yes, it’s okay to feel guilty - but guilt doesn’t help you heal. Pain management is self-care.
Wait - so you’re telling me I can’t take tramadol but I can take morphine? But morphine is still an opioid? Why is one ‘safe’ and the other ‘dangerous’ if both cross the placenta? This is arbitrary. You’re not protecting babies - you’re just favoring one drug over another based on outdated pharmacokinetics. What about the long-term neurodevelopmental data? Where’s the longitudinal study? Hmm? Anyone?
Ugh. Another ‘just take ibuprofen’ post. What about moms who can’t tolerate NSAIDs? I have a history of stomach ulcers. Acetaminophen gave me liver enzymes through the roof. So what? I’m supposed to suffer? Or pump and dump? Or give up breastfeeding? This post makes me feel like a bad mom for needing real pain relief. You’re not helping. You’re shaming.