When your thyroid-stimulating hormone (TSH) is high but your free T4 is normal, you have subclinical hypothyroidism a mild form of thyroid dysfunction where the pituitary gland produces more TSH to stimulate a thyroid that’s not quite working hard enough, but not enough to drop thyroid hormone levels below normal. It’s not a disease you can feel, and many people with it never develop symptoms. But here’s the real question: should you take a daily pill of levothyroxine just because your TSH is above 4.0 mIU/L? The answer isn’t simple. It depends on your age, your antibodies, your symptoms, and even which doctor you see.
What Exactly Is Subclinical Hypothyroidism?
Subclinical hypothyroidism isn’t a gray area-it’s a lab result with a clear definition. Your TSH is elevated (usually above 4.12 mIU/L), but your free T4 stays within the normal range. This means your thyroid is still producing enough hormone to keep your body running, but your brain is already sounding the alarm. Think of it like a car’s check engine light turning on before the engine actually fails.
The problem? Not everyone with this lab result will ever progress to full-blown hypothyroidism. Studies show that only about 20-30% of people with TSH between 4.0 and 10.0 mIU/L will develop overt hypothyroidism over five years. The rest? They stay stable. Some even go back to normal on their own.
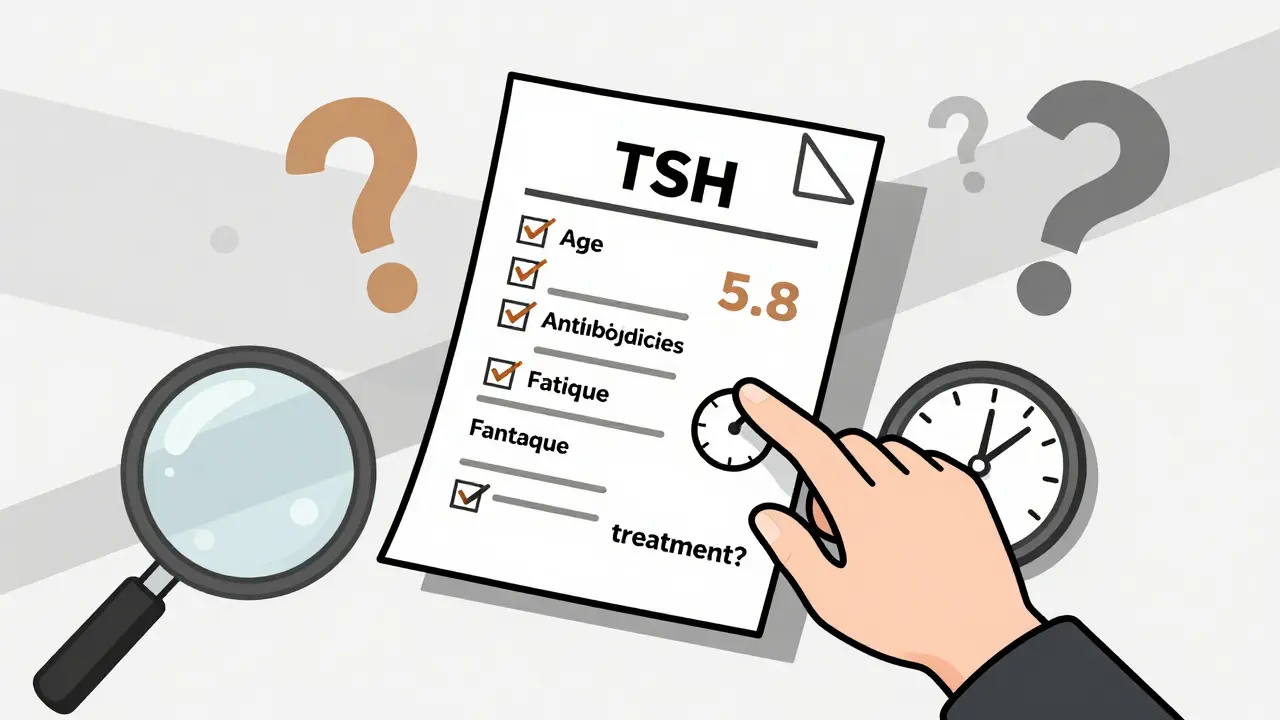
What pushes someone toward progression? Two things: thyroid peroxidase antibodies (TPO) and age. If your TPO antibodies are positive-meaning your immune system is attacking your thyroid-you’re 2.3 times more likely to develop full hypothyroidism. And if you’re under 50, your risk of progression is higher than if you’re over 65.
When Do Guidelines Say to Treat?
There’s no global consensus. In fact, major medical groups in the U.S. and Europe disagree. The American Thyroid Association (ATA) says treat only if TSH is above 10 mIU/L. The American Association of Clinical Endocrinologists (AACE) says consider treatment if TSH is above 7-8 mIU/L, especially if you have antibodies or symptoms. The Royal Australian College of General Practitioners (RACGP) says don’t treat at all if TSH is below 10 mIU/L.
Why such a mess? Because the evidence is mixed. A 2017 JAMA trial of 737 older adults found no improvement in energy, mood, or quality of life after a year of levothyroxine. But a 2020 study in Thyroid showed 32% of people under 50 with TSH between 7 and 10 mIU/L and positive antibodies reported less fatigue and brain fog after treatment.
Here’s the real takeaway: treatment isn’t about the number on the lab report. It’s about context.
Who Benefits Most from Treatment?
If you’re under 50, have positive TPO antibodies, and feel tired all the time despite sleeping enough, you might be a good candidate for treatment. A 2022 Cleveland Clinic algorithm found that 70% of patients with TSH above 8 mIU/L and positive antibodies progressed to overt hypothyroidism within four years. That’s not a coincidence-it’s a warning sign.
Women planning pregnancy should also be treated. Even if their TSH is only mildly elevated, the developing baby relies on the mother’s thyroid hormone in the first trimester. The American Society for Reproductive Medicine recommends keeping TSH under 2.5 mIU/L during preconception and pregnancy.
And what about cardiovascular risk? Some studies suggest higher TSH levels are linked to increased LDL cholesterol and arterial stiffness. A 2019 meta-analysis found a small but measurable drop in bad cholesterol after levothyroxine treatment in patients with TSH above 7 mIU/L. That’s not enough to recommend treatment for everyone-but if you already have high cholesterol or a family history of heart disease, it’s worth discussing.

Who Should Avoid Treatment?
If you’re over 65 and your TSH is between 4.0 and 10.0 mIU/L, treatment can be more harmful than helpful. A 2021 meta-analysis from the American Academy of Family Physicians (AAFP) found a 12.3% higher risk of death from any cause in elderly patients treated with levothyroxine. Why? Because too much thyroid hormone can trigger atrial fibrillation, bone loss, and muscle weakness in older adults.
Also, don’t treat based on symptoms alone. Studies show that 30-40% of people with elevated TSH report fatigue, weight gain, or cold intolerance-but so do 35% of people with normal thyroid function. These symptoms are common. They’re not proof of thyroid disease.
That’s why doctors need to use tools like the Thyroid-Related Quality of Life Patient-Reported Outcome (ThyPRO) questionnaire. It’s a 31-item survey that measures specific thyroid-related symptoms. If your score is high and your TSH is elevated, then treatment might help. If your score is normal? You’re probably fine.
What Happens If You Start Treatment?
If you and your doctor decide to start levothyroxine, you’ll begin with a low dose-usually 25 to 50 micrograms daily. That’s much less than what’s used for overt hypothyroidism (75-125 mcg). You’ll get your TSH checked again in 6 to 8 weeks. If it’s still high, the dose may go up by 12.5 to 25 mcg. The goal isn’t to crush your TSH into the bottom of the range. It’s to get it back into the normal range-usually between 0.5 and 4.0 mIU/L.
Watch out for interactions. Iron supplements, calcium, and even coffee can block absorption. Take levothyroxine on an empty stomach, at least 30-60 minutes before breakfast. And don’t switch brands. Different formulations aren’t always interchangeable.
Once your TSH is stable, you’ll need a check-up every 6 to 12 months. Most people don’t need to change their dose after the first year.
The Bigger Picture: Why This Matters
More than 13 million Americans have subclinical hypothyroidism. In 2020, over $1.8 billion was spent on testing and treating it. A 2019 study in JAMA Internal Medicine found that 22% of TSH tests were ordered without proper reason-like routine screening in healthy young adults with no symptoms. That’s money and stress wasted.
And here’s the twist: some labs still use outdated reference ranges. The upper limit for TSH used to be 5.0 mIU/L. Now, many labs use 4.12 mIU/L. That means thousands of people were told they were fine five years ago who now get labeled with a diagnosis. Is that progress-or overdiagnosis?
Future guidelines are shifting. The American Thyroid Association is reviewing its 2021 guidelines, with early drafts suggesting treatment for people under 30 with TSH above 7 mIU/L and positive antibodies. New tools are emerging too. Roche Diagnostics launched a TSH velocity calculator in 2023 that tracks how fast your TSH is rising. If it’s climbing more than 1 mIU/L per month, your risk of progression jumps 1.8-fold.
The bottom line? Don’t panic because your TSH is 5.8. Don’t rush into pills because a website told you to. Ask your doctor: Do I have antibodies? Am I symptomatic? What’s my cardiovascular risk? Am I over 65? Those questions matter more than the number on the page.
What If You’re Not Ready for Treatment?
Not everyone needs medication. If your TSH is 6.5 but you feel fine, have no antibodies, and are over 60, the safest choice is monitoring. Get your TSH checked every 6 to 12 months. Watch for new symptoms-weight gain, dry skin, constipation, depression. If they show up, revisit the conversation.
And yes, lifestyle matters. Stress, poor sleep, and extreme diets can temporarily raise TSH. Fixing those might help more than a pill.









15 Comments
Just got my TSH back at 5.2 and I’m not even sure if I should care. I sleep fine, no weight gain, and my energy’s normal. Maybe I’m just lucky? 🤷♀️
Let’s be real-the entire subclinical hypothyroidism debate is a product of overzealous lab marketing and endocrinologists chasing RVUs. The moment TSH went from 5.0 to 4.12, we created millions of "patients" out of perfectly healthy people. This isn’t medicine; it’s a surveillance state for thyroids. And don’t get me started on the thyroid industry’s $1.8B annual revenue stream-where’s the FDA oversight? Nowhere.
People are popping levothyroxine like vitamins because they read about it on a blog that cites a single 2020 study while ignoring the 2017 JAMA trial that showed zero benefit. We’ve normalized medicalizing normalcy. The real epidemic isn’t low T4-it’s the cult of biomarker worship.
And yet, the same people who scream about "overdiagnosis" in prostate cancer or mammograms are the first to panic when their TSH hits 5.8. Double standards? Oh, absolutely. But it’s not about evidence-it’s about fear. Fear of aging. Fear of fatigue. Fear of not being "optimally optimized."
My advice? If you’re asymptomatic, over 50, and TPO-negative, your thyroid is doing fine. Stop Googling. Stop obsessing. Stop treating a number like it’s a moral failing. Your pituitary isn’t broken. Your body isn’t failing. You’re just… normal. And that’s okay.
OMG this is the most accurate thing I’ve read all week. I mean, seriously-how many times do we have to be told that symptoms aren’t diagnostic? I had a doc last year who wanted to put me on synthroid because my TSH was 6.1 and I "felt kinda blah." Bro. I just moved apartments, slept 4 hours a night for 3 weeks, and ate nothing but ramen. My thyroid didn’t fail. My life did.
Also, coffee before levothyroxine? That’s not a recommendation-that’s a crime against endocrinology. I’ve seen people take it with their morning latte and wonder why their levels are "fluctuating." It’s not the thyroid. It’s the caffeine.
And don’t even get me started on brand switching. I switched from generic to Synthroid because my "symptoms" got worse. Turns out, my body just needed 2 weeks to adjust. Now I’m stuck paying $80/month for a pill that’s chemically identical to the $4 version. Pharma, you’re a scam.
The notion that subclinical hypothyroidism should be universally treated is not only unsupported by evidence-it is actively dangerous. The literature consistently demonstrates that overtreatment in the elderly leads to iatrogenic hyperthyroidism, with associated increases in atrial fibrillation, bone turnover, and all-cause mortality. To prescribe levothyroxine to a 72-year-old with a TSH of 6.5 and no symptoms is not clinical care; it is iatrogenic harm disguised as precaution.
Furthermore, the reliance on TSH as a standalone biomarker ignores the physiological reality of thyroid homeostasis. TSH is a feedback signal, not a disease marker. Its elevation may reflect transient stress, inflammation, or even circadian variation-not necessarily autoimmune destruction.
The most compelling argument for intervention lies not in population averages, but in individualized risk stratification: TPO antibody status, age, reproductive status, and cardiovascular profile. Without these, treatment is arbitrary. And arbitrary treatment, in the absence of benefit, is unethical.
I’m so glad someone finally wrote this. I’ve been telling my friends for years: if you’re not sick, don’t take a pill. 😊
My mom was put on levothyroxine after her TSH hit 5.5, and she got anxious, lost weight, and started sweating at night. Turns out, she was fine. She just needed more sleep and less sugar. Now she’s off it, and she’s happier than ever. 🌿
Also-yes to the ThyPRO questionnaire. It’s underused, but so helpful. I wish more doctors would use it instead of just staring at numbers. 💬
From a clinical endocrinology standpoint, the key determinant of progression is not TSH alone but the presence of TPOAb in conjunction with a rising TSH velocity. The 2023 Roche TSH velocity algorithm demonstrates that a rate of increase >1 mIU/L/month predicts progression to overt disease with 89% specificity in patients under 50. This is now incorporated into NICE guidelines as a tiered risk stratification tool.
Additionally, in patients with autoimmune thyroiditis, the annual conversion rate is approximately 2.5–4.5%, but this increases to 15–20% if TPOAb titers exceed 500 IU/mL. Serial monitoring every 6–12 months with TSH and TPOAb is more cost-effective than immediate pharmacotherapy in low-risk cohorts.
For preconception patients, the 2.5 mIU/L threshold remains valid due to placental deiodinase activity in early gestation. However, in non-pregnant individuals, the ATA’s 10 mIU/L threshold remains evidence-based and prudent.
Oh, so now we’re supposed to ignore the science because some people "feel fine"? That’s the same logic that kept people from treating hypertension for decades. "I don’t feel dizzy," they said. Then they had a stroke.
High TSH is a biomarker of thyroid failure. It doesn’t need to "feel" like anything to be dangerous. You think your body is fine? You think your cholesterol doesn’t matter if you don’t feel it? You’re lucky you’re young. Wait until you’re 60.
And don’t even get me started on the "lifestyle" nonsense. If your thyroid is failing, kale and meditation won’t fix it. You need hormone replacement. Period. End of story.
It is, without question, a profound disservice to public health that primary care providers are permitted to order TSH tests without clinical indication. The 2019 JAMA Internal Medicine study revealed that over 22% of TSH tests were ordered in asymptomatic individuals under the age of 30-many of whom were undergoing routine physicals or pre-employment screenings. This is not medicine. This is commodification of physiology.
Furthermore, the widespread adoption of the 4.12 mIU/L upper limit, which was derived from a single cohort of healthy adults excluding those with TPO antibodies, has artificially inflated prevalence by over 300%. This is not progress-it is diagnostic inflation.
And yet, the medical-industrial complex continues to profit from this. Levothyroxine is now among the top five most prescribed drugs in the United States. Coincidence? I think not.
Let us return to evidence. Let us return to caution. Let us return to the principle of primum non nocere.
Love how this thread is going. Everyone’s got a take, and honestly? That’s healthy. 🌱
I’ve got a friend who was told she had subclinical hypothyroidism after a routine checkup. She didn’t believe it, got a second opinion, found out her lab used an outdated range, and switched to a better one. Her TSH dropped from 5.8 to 3.9. No meds. Just better testing.
Also-yes to monitoring. I’ve been tracking mine for 3 years. Went from 4.5 to 4.1 to 4.0. No symptoms. No meds. Just chillin’.
Let’s stop treating labs like horoscopes. 😊
Look-I get it. People want to believe that their thyroid is just "a little off" and that they can fix it with lemon water and yoga. But here’s the uncomfortable truth: your thyroid doesn’t care about your Instagram detox. It doesn’t care if you sleep 8 hours or if you’re "in alignment."
If your TSH is above 4.12 and you’ve got positive TPO antibodies, you’re on a ticking clock. The data doesn’t lie. You’re 2.3x more likely to crash into overt hypothyroidism. That’s not a "maybe." That’s a biological inevitability.
And let’s not pretend that elderly patients are immune to harm from overtreatment. Sure, they’re at higher risk. But so are young women with untreated hypothyroidism who end up with miscarriages or babies with developmental delays. This isn’t a debate about fear-it’s a debate about responsibility.
Stop romanticizing "natural" thyroid health. The thyroid is an endocrine gland. It doesn’t need crystals. It needs T4. And if you’re at risk? You owe it to yourself-and to your future self-to take the pill.
Yes, it’s a daily chore. Yes, it’s a pill. But it’s also the difference between dragging through life and actually feeling like yourself.
And if you’re over 65 and asymptomatic? Fine. Don’t take it. But don’t lecture the rest of us who are trying to prevent decades of fatigue, weight gain, and brain fog.
USA: 13 million people with subclinical hypothyroidism. India: 20 million. China: 35 million. This isn’t a medical issue-it’s a global crisis of overtesting and underthinking. Why are we treating a number instead of a person? Because money talks louder than science.
And don’t even get me started on how American labs changed the range from 5.0 to 4.12 overnight. That’s not science. That’s corporate greed with a white coat.
We need a global standard. We need regulation. We need to stop letting private labs decide who’s "sick."
My TSH was 5.1. No symptoms. No antibodies. Waited 6 months. Now it’s 4.0. No meds needed.
I’ve been a nurse for 18 years and I’ve seen this play out a hundred times. A patient comes in with a mildly elevated TSH, panics because they read something online, and begs for levothyroxine. We check antibodies, ask about symptoms, review lifestyle-and 70% of the time, they don’t need it.
But here’s the thing: when we do treat, it’s life-changing. I had a 42-year-old woman with TSH 8.3, positive antibodies, and constant brain fog. Started on 25 mcg. Three months later, she cried in my office because she remembered what it felt like to focus at work. That’s real.
It’s not about the number. It’s about the person. Listen. Watch. Measure. Don’t just prescribe.
While the data on asymptomatic elderly patients is compelling, I must respectfully challenge the assumption that younger patients with TSH 6–8 and positive antibodies are uniformly better off on levothyroxine. A 2023 Cochrane review of 12 RCTs found no statistically significant improvement in cognitive function, mood, or quality of life in this subgroup when compared to placebo-despite TSH normalization. The perceived benefit may be placebo-driven or confounded by heightened health surveillance.
Moreover, the 70% progression rate cited from Cleveland Clinic is derived from a single observational cohort with high selection bias. It is not generalizable to primary care populations. Longitudinal studies show that even in antibody-positive patients, progression is slow, and many remain stable for decades without intervention.
Therapy should be reserved for those with clear, reproducible symptoms AND elevated TSH AND positive antibodies-not based on risk algorithms alone. We must resist the temptation to medicalize ambiguity.
And yet, in that same Cochrane review, the only subgroup with consistent, clinically meaningful improvement was women under 40 with TSH >7 and positive TPO antibodies-precisely the group most likely to be planning pregnancy or experiencing unexplained fatigue. The absence of statistical significance in cognitive tests doesn’t negate the lived experience of hundreds of thousands who feel better. Science doesn’t always capture quality of life-it captures averages. But people aren’t averages.
Also, selection bias? Of course there is. But when 70% of a cohort progresses within four years, and the alternative is untreated thyroid failure, the ethical default is intervention-not observation. We don’t wait for heart attacks to treat hypertension. Why wait for infertility or dementia to treat thyroid failure?
Yes, we must be cautious. But caution shouldn’t mean paralysis.