Drug Interactions: What You Need to Know About Dangerous Medication Combos
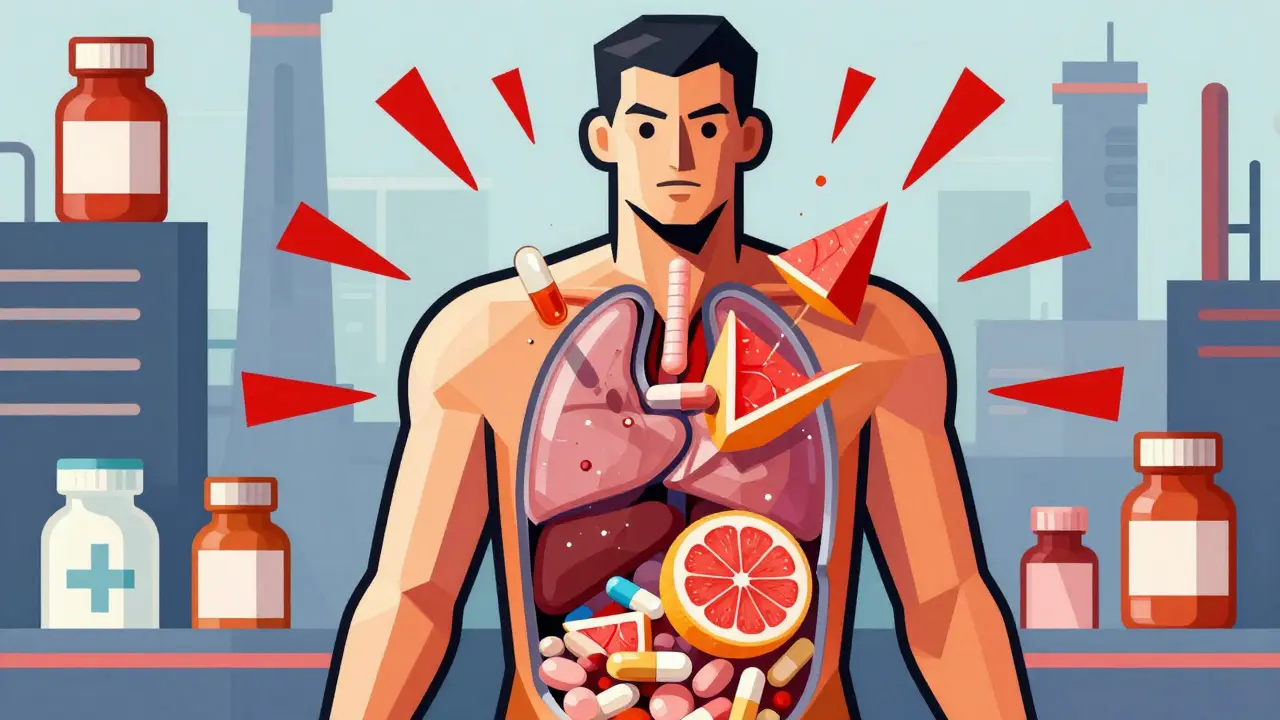
When you take more than one medication, your body doesn’t always handle them the way your doctor expects. This is where drug interactions, harmful or unexpected reactions that happen when two or more drugs affect each other in the body. Also known as medication interactions, it can turn a routine prescription into a life-threatening situation. It’s not just about pills you take together—it’s about what you eat, what supplements you use, even what you drink. A simple combo like steroids and NSAIDs can double your risk of internal bleeding. Statins and certain antifungals can wreck your muscles. These aren’t rare cases. They happen every day, often because no one asked the right questions.
Not all drug interactions, harmful or unexpected reactions that happen when two or more drugs affect each other in the body. Also known as medication interactions, it can turn a routine prescription into a life-threatening situation. are obvious. Some hide in plain sight. For example, antibiotics like doxycycline make your skin burn faster in the sun. Blood thinners like warfarin react wildly based on your genes. Even something as simple as grapefruit juice can stop your body from breaking down common heart meds. And it’s not just about what’s on your prescription list—over-the-counter painkillers, herbal supplements, and vitamins can all play a part. The FDA tracks these risks through real-world reports, but the system isn’t perfect. That’s why you need to be your own advocate. Know what you’re taking. Ask your pharmacist: "Could this interact with anything else I use?"
Some interactions are so dangerous they require constant monitoring. QT prolongation from antibiotics like azithromycin can trigger irregular heart rhythms. Immunosuppressants like prednisone make you vulnerable to infections you’d normally shrug off. And for older adults, benzodiazepines and certain diabetes drugs can lead to falls, confusion, or low blood sugar that slips under the radar. These aren’t theoretical risks—they show up in hospital ERs, nursing homes, and at home, often because no one connected the dots. The good news? Most of these problems are preventable. You don’t need to stop your meds. You just need to understand the risks and know what signs to watch for.
Below, you’ll find real-world guides that break down the most common and dangerous drug interactions people actually face. From how to avoid GI bleeding when mixing steroids with NSAIDs, to why your statin might be unsafe with an antifungal cream, to how to spot early signs of suicidal thoughts in teens on antidepressants—these aren’t theory pages. They’re checklists, warnings, and practical fixes written by people who’ve seen the fallout. Whether you’re managing multiple prescriptions, caring for an aging parent, or just trying to stay safe while taking a new medication, you’ll find answers here—not guesses, not fluff, just what works.
How to Check for Drug Interactions Before Starting New Medications: A Step-by-Step Guide
Learn how to prevent dangerous drug interactions before starting new medications with practical steps, free tools, and expert-backed advice. Protect your health with a complete medication list and smart questions to ask your doctor.
read more
Seizure Medications and Pregnancy: Risks of Birth Defects and Drug Interactions
Certain seizure medications carry serious risks during pregnancy, including birth defects and developmental issues. Learn which drugs are safest, how they interact with birth control, and what steps to take before conceiving.
read more
ACE Inhibitors and ARBs: What You Need to Know About Interactions and Cross-Reactivity
ACE inhibitors and ARBs are both used for high blood pressure and kidney protection, but combining them increases serious risks like hyperkalemia and kidney failure without added benefits. Learn why doctors avoid this mix and what to do instead.
read more




